1. Background
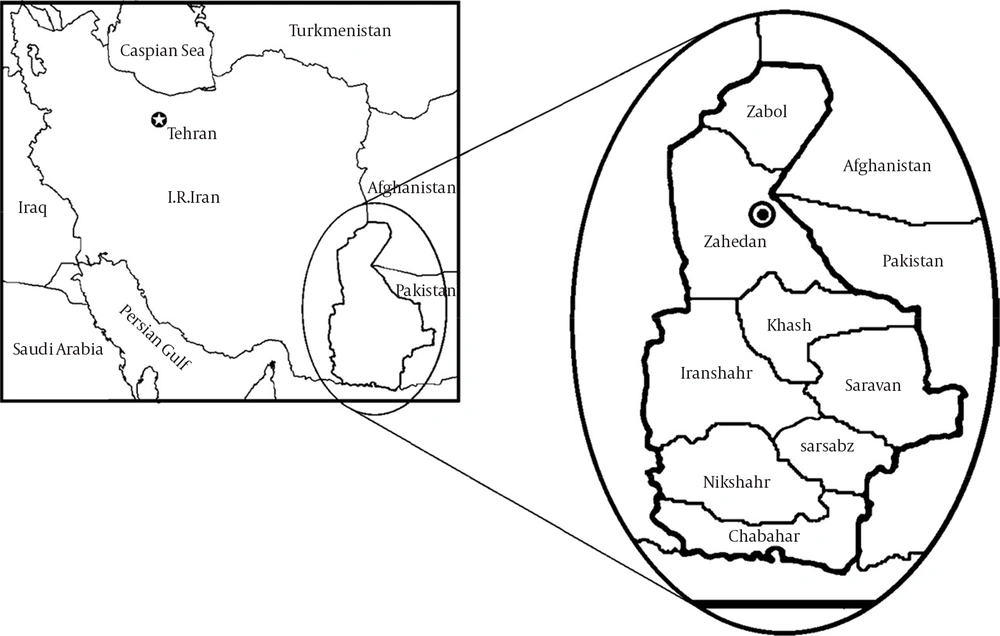
Cholera is an infectious disease, caused by Vibrio cholera. The classic symptom of the disease is severe acute diarrhea. If dehydration and electrolyte imbalance are compensated properly, the disease resolves spontaneously, otherwise causes a high mortality (1, 2). Several hundred thousand people are infected with Vibrio cholera every year worldwide, with a case fatality rate over 2 % (3). There happens 100000–120000 deaths due to cholera every year, of which only a small proportion are reported to WHO (3). The highest incidence of cholera in Iran occurs in Sistan and Baluchestan province, the widest province in Iran, having a long border with Pakistan and Afghanistan (Figure 1). Cholera periodic outbreaks, especially due to ungovernable border crossing, threaten the province population health. Therefore good management and control of cholera can reduce the total burden of this disease and reduce the health costs in Iran. Iran health ministry policy about cholera control is accessibility to safe water, sanitation, control of eastern border crossings and finally reducing the cholera incidence to zero (2). Performing outbreaks control programs and patients’ treatments have human and financial costs. Therefore, cholera is a health priority in Sistan and Baluchestan province.
2. Objectives
In this study we evaluated cholera outbreak changes and its epidemiology during 2010-2013 in Sistan and Baluchestan province. Afterwards the environmental determinants were assessed.
3. Materials and Methods
This is a historical cohort study on the total population, serviced by Zahedan University of Medical Sciences as the population at risk (except Zabol city). Based on cholera surveillance program, epidemiologic data of all patients are documented in every city disease control department and then reported to the province health center in Zahedan. All Cholera patients’ epidemiologic data (including age, sex, nationality, living location and city) were extracted from the epidemiological documents in the disease control department (Zahedan Health Center), during 2010-2013. Afterwards the environmental determinants, like sanitation (percentage of families who had sanitary latrine and wastewater disposal system) and accessibility to safe water (percentage of families who had access to safe water) were assessed in every outbreak. Also every year management indices, including inter-sectoral cooperation, as number of coordinating meetings (between the governor, municipality, the Water and Sewer Department and Department of Transportation) and allocated resources (financial and human resources) were determined. We tried to describe the epidemiology of cholera disease in our population and based on every subgroup population, we calculated the relative risk factors and the relationship between sanitation determinants, management indices and cholera case numbers in every outbreak, by Pearson correlation test.
4. Results
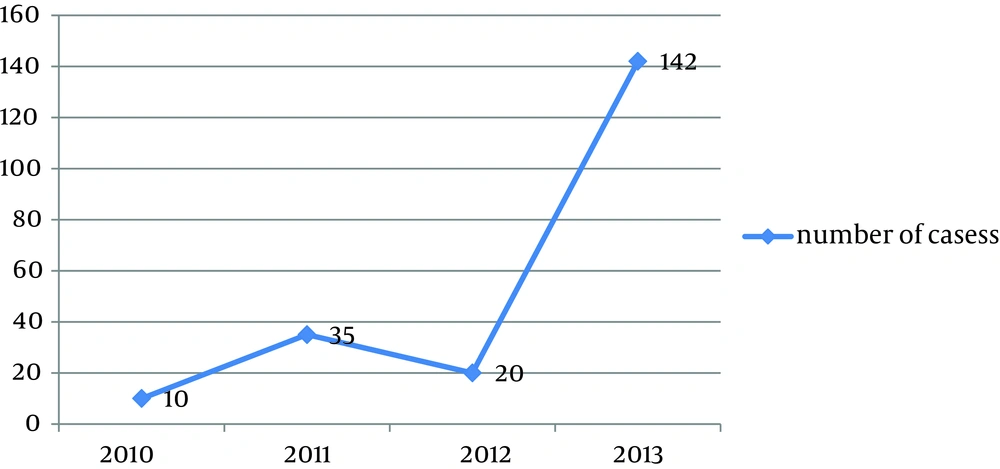
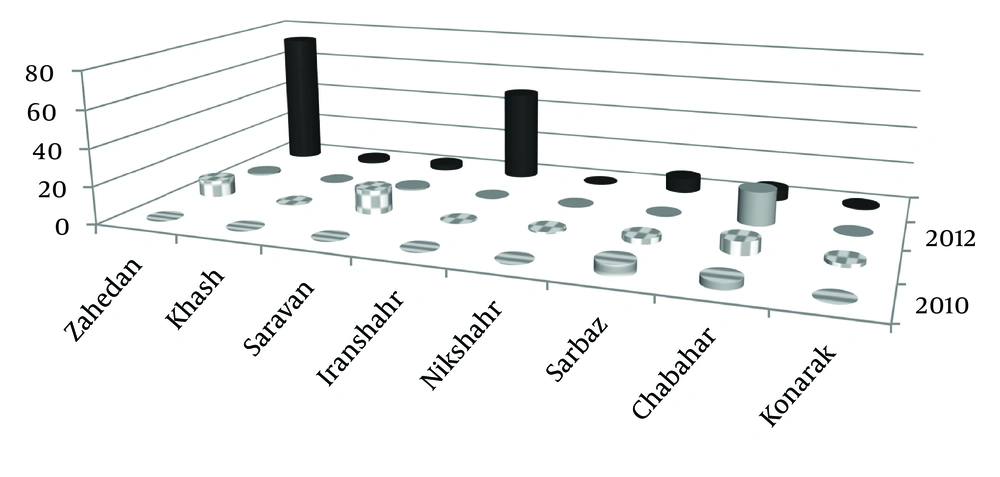
Number of cases in every cholera outbreak, during 2010-2013, is summarized in Figure 2. As demonstrated, the largest outbreak occurred in 2013. In terms of nationality, 63.3% of all cases were Afghan and 46.7% were Iranian. The annual number of cases in every city was different, but generally during all four years, the highest number of cases happened in Zahedan city, due to the biggest outbreak in Afghan immigrant camp in 2013, causing 70 cholera cases (Figure 3). Most cases were reported to be in the age group of 20-29 and 10-19 with 40.8% and 27.5% of cases, respectively. Incidence rate was significantly higher in men than women (RR = 2.8), in foreign immigrants than Iranians (RR = 44.1) and in rural populations than in urban populations (RR = 26.2). We observed an improving trend in city safe water accessibility (percentage of families who had access to safe water) and sanitation system index (percentage of families who had sanitary latrine), for all cities, during these four years, without any significant relationship to number of cholera cases, based on the Pearson correlation test result (P = 0.305), because most cases had occurred in remote rural areas or places with non-sanitary environments, without access to safe water, like immigrant camps. In this study we did not find a significant relation between management indices, including inter-institutional cooperation, as numbers of coordinating meetings (between the governor, municipality, the Water and Sewer Department and the Department of Transportation) and allocated resources (financial and human resources), every year, based on the Pearson correlation test (P = 0.142).
5. Discussion
Although in endemic areas cholera occurs more frequently in children, the epidemics in non-endemic areas more frequently affect adults (1, 2). Findings of this study are compatible with non-endemic areas, probably due to outside origin of infection (Afghanistan and Pakistan). Cholera incidence rate was higher in men than in women in all epidemics, mostly due to their jobs and state of being outdoors (1, 4), as found by our study. Regarding cholera outbreak control, WHO recommends providing safe water, environmental sanitation, providing safe food and healthy behaviors and in addition emphasizes on controlling foreign travelers and imported food safety (5-10). Zahraie et al. evaluated cholera epidemiology in Iran in 2005 and concluded that despite health indices improvements , bordering with Afghanistan and Pakistan, inaccessibility to safe water in some rural areas, lack of personal hygiene and lack of wastewater disposal systems, cholera is still one of the health priorities in Iran (11). As found by this study, some subgroups including rural populations and foreigners, have more risk for cholera, especially in immigrant camps, due to poor water sanitation system and inaccessibility to safe water. In 2005 Kakar, F. et al. studied cholera outbreaks in Afghanistan and revealed that cholera mortality reduction is possible through government participation, inter-sectoral coordination and proper management and treatment of patients (12). But due to our study findings, no significant difference was found regarding inter-sectoral coordination in different years. In a study conducted on Bangladesh rural population, during 1999-2002, Rita et al. emphasized on providing safe water, even by simple filtration (13). Additionally Brown V studied cholera epidemiology among refugees and reported that international cooperation, providing safe water, proper human waste disposal systems, sanitation and personal health behaviors are important factors in epidemics control (14). In our study the higher incidence was found in imimmigrant camps and rural areas, probably due to unsafe water use. Despite the improving trend of safe water accessibility index in all cities, during these four years, providing safe water has not been practically possible for some remote areas in this wide province. In addition, uncontrolled border travelling has intensified the safe water problem. On the other hand, as we found out, foreign immigrants, living in non-sanitary environment and having almost no access to safe water, were at a higher risk for developing cholera. We were not able to find any significant relation between cholera incidence rate and management indices, which can be due to the fact that all management programs, coordinating meetings (the governor, municipality, Water and Sewer Department and Department of Transportation) and allocating resources (financial and human resources) were performed after outbreaks and not before. Problems like poor sanitation and safe water shortage in rural and remote areas and in immigrant camps necessitate allocating more resources, better Inter-institutional cooperation and border travelling control in this province, especially before cholera, for prevention.