1. Background
Leishmaniasis is a vector-borne disease caused by protozoan parasites belonging to the genus Leishmania. The parasites are transmitted by the bite of the Phlebotomine sandfly. Based on the causative agent and clinical manifestation, leishmaniasis is classified into three types of cutaneous, mucocutaneous and visceral leishmaniasis. The most common clinical presentation of CL (cutaneous leishmaniasis) is localized ulcer or nodule (1).
Human infection is caused by about 21 of 30 species that infect mammals. These include Leishmania donovani complex with 2 species (L. donovani, L. infantum [also known as L. chagasi in the New World]), the L. mexicana complex with 3 main species (L. mexicana, L. amazonensis and L. venezuelensis), L. tropica, L. major, L. aethiopica and the subgenus Viannia with four main species of (L. (V.) braziliensis, L. (V.) guyanensis, L. (V.) panamensis and L. (V.) peruviana) (1).
Although spread of CL is globally, its geographical distribution is usually locally due to specific habitat requirements of the sandfly vector and its various reservoir hosts (2).
It is usually a zoonotic disease with many different mammalian reservoirs, but sometimes it can be anthroponotic in epidemics and urban environments; this situation has been reported in Sudan, Afghanistan and India. In the recent years, CL has been considered as a cause of morbidity and social stigma in war-torn countries such as Afghanistan (3, 4).
Although leishmaniasis is responsible for the ninth largest disease burden among individual infectious diseases, it is mainly ignored between tropical disease priorities. The disease has been neglected as a major public health problem because it is not a fatal disease (5).
No effective vaccines or prophylactic drugs are available for prevention of infection. Preventive interventions include contact reduction with sandflies by applying individual protective measures.
Currently, leishmaniasis is endemic in 88 countries, 72 of which are developing countries; 90% of all visceral leishmaniasis cases occur in Bangladesh, Brazil, India, Nepal and Sudan, 90% of mucocutaneous leishmaniasis occurs in Bolivia, Brazil and Peru and 90% of cutaneous leishmaniasis cases occur in Afghanistan, Brazil, Iran, Peru, Saudi Arabia and Syria. More than 20000 CL cases are reported annually in Iran, but due to under-reporting, the real incidence is probably 4 - 5 times more. More than 80% of CL cases in Iran are rural (wet) form and the incidence rate of CL was reported 27/100000 in 2011 (6). Based on Iran health ministry statistics, leishmaniasis incidence rate in Sistan and Baluchestan province was 14 - 36 /100000 in 2011 (6).
2. Objectives
Update epidemiological data about risk factors, high risk groups and geographical distribution of disease are necessary to plan effective control interventions. In this study, we tried to evaluate the incidence trend and epidemiology of CL in south of Sistan and Baluchistan province to provide better interventions.
3. Patients and Methods
This was a historical cohort study performed from April 2008 to March 2014. Our study population was all people covered by Zahedan University of Medical Sciences. (All Sistan and Baluchistan Province population, except population under Zabol University of Medical Sciences service). We studied all registered patients with CL during the mentioned period. We extracted data from Zahedan Health Center registry.
Based on Iranian health ministry policy about leishmaniasis management, there is an electronic registering system in all cities health centers. Patients with CL, after clinical and laboratory diagnosis, refer to such centers for recording epidemiological data, getting their drugs and follow-up. State health services are the main anti leishmaniasis drug supplier and treatment is free in these centers. All patients’ data is reportable in Zahedan Health Center registry. Of course, there is an underestimation due to some misdiagnosis or undiagnosed disease in some patients and lake of referring some patients to this registry, but this registry is the most accurate and available source for patient’s data. We evaluated all patient epidemiological data from April 2008 to March 2014. To adhere to ethical considerations, we kept confidential of all patients’ private data.
Descriptive statistics like range, mode, percentage and 95% confidence interval were used, also incidence rates and reported relative risks for some risk factors were calculated.
To calculate incidence rates, we used subgroup population data from Iran Statistics Center as denominators.
4. Results
During six years study, 2863 CL cases were reported in our population. 59.9% (1698 cases) were male and 40.7% (1165 cases) female, age range of patients was 1 - 92 years with a median of 18 years. Among our patients, 733 cases (25.6%) were living in urban areas and 2130 cases (74.4%) in rural regions.
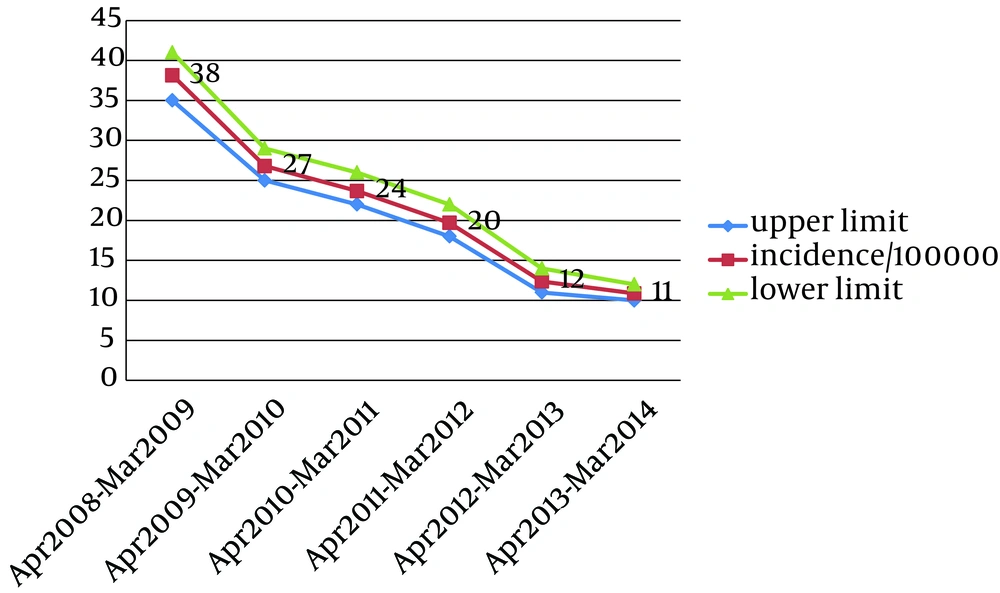
A decreasing incidence trend of CL based on our registry is summarized in Figure 1. As seen, the incidence rate decreased significantly from 38/100000 during 2008 - 2009 to 11/100000 during 2013 - 2014.
Incidence rate of CL in men (27.59/100000) was significantly more than women (19.7/100000) as RR: 1.4 with CI 95%: 1.29 - 1.51.
Our results showed the incidence rate in rural areas as 35.43/100000 and in urban regions 12.07/100000 (RR: 2.9 with CI95%: 2.68 - 3.20).
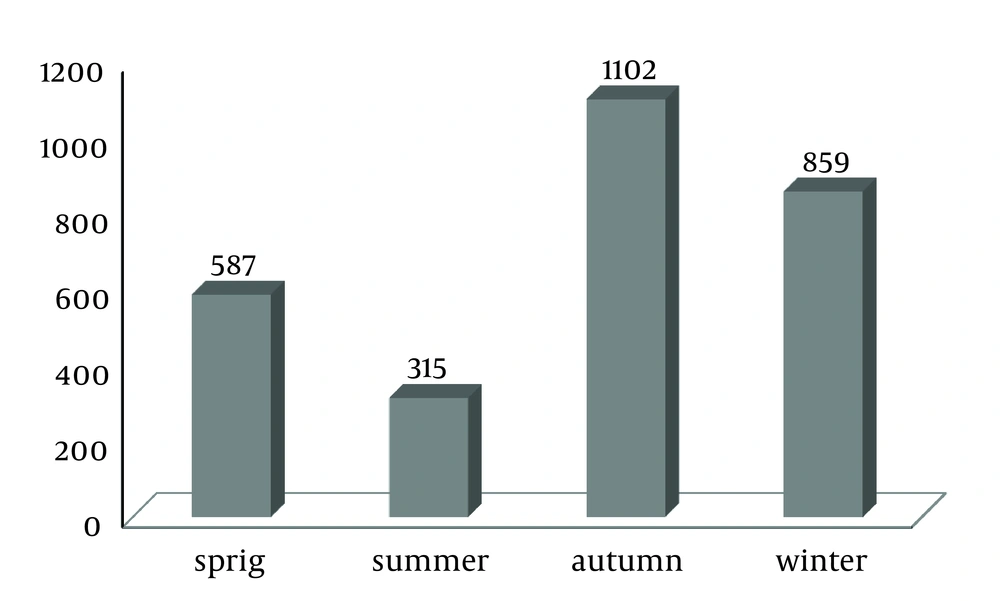
Number of cases in different seasons is shown in Figure 2. As seen, most cases occurred in autumn and winter.
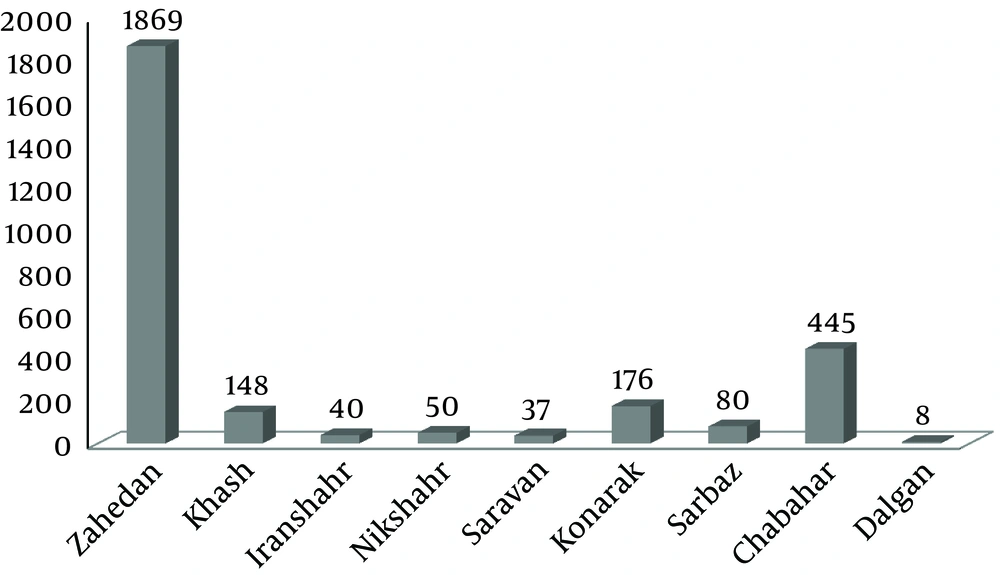
As Figure 3 shows, most cases occurred in Zahedan city (66.5%), Chabahar city (15%), Konarak (5.9%) and then Khash (5.3%). Main CL centers were around Zahedan city (Mirjaveh, Rig Malek regions) and around Chabahar city and Konarak city (Dashtyari, Bahoocalat and Zar Abad regions).
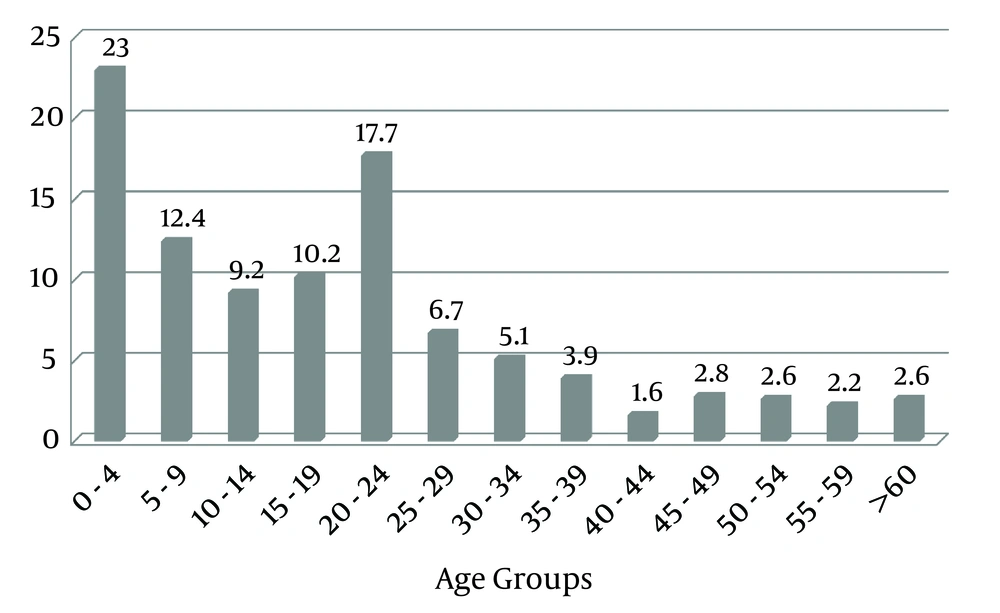
The age range of patients was 1 to 93 years, but age mode was 2. Most cases reported in age group under 5 (23%) following age group 20 - 24 (17.7%). Totally, 72.5% of all cases reported in age group under 25 (Figure 4).
Most CL wounds diagnosed respectively in hands (30.2%), head and neck (22%), feet (17.3) and then legs (10.3%).
Wound number varied from 1 to 22, but in 60.2% of all patients only one wound reported.
5. Discussion
Leishmaniasis is a poverty-related disease. It affects the poorest people and associated with malnutrition, displacement and poor housing and illiteracy, weakness of the immune system and lack of resources. Leishmaniasis is also linked to environmental changes such as deforestation, building of dams, new irrigation schemes and urbanization and accompanying migration of non-immune people to endemic areas (7, 8).
During our six-year study, we observed a significant decreasing incidence trend. Totally, 2863 CL cases were registered. Due to unregistered cases, there is an underestimation and true incidence rate is probably higher than our result. However, the only accessible and reliable epidemiologic data source about leishmaniasis in our province is Zahedan health center registry, because Zahedan health center and its offices around province are the main drug supplier for leishmaniasis and most patients in all cities refer to this center and its offices for free treatment.
We observed a clear decreasing registered trend during these six years, which can reflect a partial success in leishmaniasis control programs.
Vectors in rural leishmaniasis are desert rodents and four spices of them identified in Iran and most cases were reported during October, November and December (6). A seasonal variation with maximum incidence between November and January was reported in Saudi Arabia (9).
Faraj and Lake studied the seasonality of cutaneous leishmaniasis in Asir region, Saudi
Arabian during 1996 to 2007. They found a clear seasonality with peak incidence between October and March (10). In our study, most cases were diagnosed during autumn and winter, which is compatible with other studies.
Yaghoobi-Ershadi et al. (11)in a study in 2001 in Ardestan city (central Iran) found the most highly infected age group as 10 - 14 years.
Nateghi Rostami et al. (12) in 2006 - 2011 evaluated all leishmaniasis cases in Ghomrood and Ghanavat regions (central Iran) and found that most (50%) patients aged 1 - 25 years and most (55.1%) had a single lesion.
Layegh et al. (13) investigated Cutaneous Leishmaniasis in Mashhad (north east of Iran) and showed female to male ratio as 0.9 with the highest prevalence in 6 - 9 year age group. Most of our patients aged below 5 years, which is relatively different from other studies.
Pedrosa and Ximenes (14). performed a multivariate analysis on the association between ACL and risk factors relating to work, school and leisure activities and activities outside home, considering both neighbor and community controls: Alagoas, 2004 - 2007 in Brazil. They showed that rural school or work activity and Forest leisure were risk factors for American Cutaneous Leishmaniasis (14). Our study also showed that CL risk in rural areas was 2.9 times more than urban regions.
Bettaieb et al. (15) evaluated prevalence and determinants of Leishmania major infection in Tunisia and found no significant difference between males and females suggesting that they are equally exposed to infection.
Soares et al. (16) investigated epidemiology of cutaneous leishmaniasis in central Amazonia and observed moderately higher incidence of CL among men than women.
Salman et al. (17) studied cutaneous leishmaniasis cases in Nizip, Turkey after the Syrian civil war and reported that 61% of patients were female and 39% male. Of positive patients, 67.5% belonged to 0 - 19 age group. Male to female ratio in this study was in contrast to our results.
Sharifi et al. (18) evaluated Cutaneous Leishmaniasis in Kerman Province (Southeastern Iran) in 2011 - 2013. They showed that most lesions were single and reported that females were more significantly infected than males.
We found that the risk of disease in men was 1.4 times more than women probably due to outside working in men in comparison with women and differences in dress (clothes for women are more covered than men).
Main CL centers were around Zahedan city (Mirjaveh, Rig Malek regions) and around Chabahar city and Konarak city (Dashtyari, Bahoocalat and Zar Abad regions).
The most common area of CL wound respectively were hands, head and neck and feet. Most patients had only one wound.
Our result such as higher incidence in men and in rural areas, season of highest incidence (autumn and winter), patient’s age (children and young adult), areas of wounds and number of wounds (single wound) were completely compatible with other studies in other cities of Iran (Mashhad, Kashan) (19, 20).
A regional plan on control strategies for leishmaniasis in the Eastern Mediterranean Region is based on four pillars” (a) training program managers and health workers on diagnosis and case management; (b) establishing a harmonized regional surveillance system; (c) creating a regional network of experts and (d) promoting political commitment of national governments” (21).
Based on the Eastern Mediterranean Region plan for leishmaniasis control, in this study we tried to update geographical information systems, epidemiological data and sharing them with health policy makers to better control strategies.
Decreasing registered cases during recent six years reflects the partial success in leishmaniasis control. This incidence reduction can be related to improve in development infrastructures as sanitation systems that could reduce sandfly density and related to control programs performed by health services.
Update data about geographical CL distribution and determination of high risk groups and risk factors can guide our intervention more effectively.