1. Background
Hepatitis B is a potentially life-threatening liver infection caused by the Hepatitis B virus (HBV). A total of 1.5 million new infections occur each year, and more than 800,000 people die from HBV infection, mostly as a result of cirrhosis or hepatocellular carcinoma (1). Globally, Hepatitis B virus is the leading cause of chronic liver disease, and it is estimated that in 2019 approximately 296 million individuals were living with chronic Hepatitis B infection worldwide (World Health Organization, 2022) (2).
In highly endemic areas, Hepatitis B infection is most commonly transmitted perinatally from an infected mother to newborn babies, with most cases associated with intrauterine infection (3). Infants and children who contract the infection before the age of 5 years are highly likely to develop chronic infection (1).
Hepatitis B can be eliminated through the immunization of newborns against HBV and universal screening of pregnant women for Hepatitis B surface antigen (HBsAg) during pregnancy. Evidence suggests that at least 10% of babies born to HBV-infected pregnant mothers with high levels of viremia contract the infection during pregnancy and labor (4). Thus, early detection of Hepatitis B virus infection during pregnancy and timely interventions are crucial to preventing mother-to-child transmission of HBV (1).
Hepatitis B virus DNA testing for HBsAg-positive pregnant women should be performed at 26 - 28 weeks to identify highly viremic mothers and administer antiviral therapy in the third trimester of pregnancy (5). Antiviral therapy can effectively prevent perinatal transmission in mothers with ≥200,000 IU/mL of HBV DNA, combined with the administration of Hepatitis B immunoglobulin and HBV vaccination within 12 hours of birth for newborns (5).
According to three systematic reviews and meta-analyses of epidemiological studies conducted in Iran, the prevalence of HBV infection among pregnant women was estimated at 1.18%, 1.2%, and 0.5%, respectively (6-8). The estimated prevalence of HBV infection ranged from 0.4% in the northern regions of the country to 1.6% in the eastern regions (6).
In more recent studies, the seroprevalence of HBV infection among pre-pregnancy and reproductive-age women in Tabriz was 1.2% (9), and the prevalence of Hepatitis B virus among pregnant women in the south of Iran was 1.05% (10). Lower levels of HBV infection have been reported in other settings. The prevalence of HBsAg in pregnant women in Isfahan Province was found to be 0.5% (11), and only 0.2% of pregnant women referring to the Sari Birth Cohort Center were HBsAg-positive (12).
In addition to an increased risk of vertical transmission, chronic HBV infection in pregnant women may be linked to unfavorable perinatal outcomes, including miscarriage, fetal malformations, low birthweight, large-for-gestational-age infants, increased intrauterine fetal death, stillbirth, and fetal distress (13). Moreover, pregnant women with chronic Hepatitis B infection are at an increased risk of gestational diabetes, post-partum hemorrhage, preterm delivery, pre-eclampsia, eclampsia, intrahepatic cholestasis of pregnancy, premature rupture of membranes, cesarean delivery, and placental abruption (13, 14).
2. Objectives
Sistan and Baluchestan Province has the highest rates of HBV infection in the country, second only to Golestan Province, with an estimated 3.38% of the population being HBsAg carriers (15). However, to the best of our knowledge, no recent studies with large sample sizes have investigated the prevalence of chronic HBV infection among pregnant women in this province. The objective of this study was to determine the prevalence and correlates of chronic HBV infection among pregnant women who were referred to the Central Laboratory of Zahedan, Iran, for prenatal screening tests.
3. Methods
3.1. Study Population
This cross-sectional study was conducted between August and December 2019 in Zahedan, southeast Iran. The study population comprised pregnant women who were referred to the Central Laboratory of Zahedan for prenatal screening tests, including HBsAg. Based on data from this center, among 921 pregnant women tested for HBV infection within the first six months of 2018, 20 subjects (2.2%) had a positive HBsAg test result. Therefore, for sample size calculation, the prevalence of HBV infection was considered as P = 0.022. With α = 0.05, d = 0.008, and accounting for a 10% attrition rate, the sample size was calculated to be 1,435 pregnant women. The pregnant women who visited the Central Laboratory were recruited using a convenient sampling method. After obtaining their written consent, individuals willing to participate in the study were interviewed.
For pregnant women with a positive HBsAg test result at the first prenatal visit, maternal HBsAg testing was repeated at 24 - 28 weeks of gestation. If the result remained positive, these cases were considered chronic Hepatitis B infection, and a real-time quantitative PCR test was performed to assess HBV serum viral load.
3.2. Data Collection
A 32-item semi-structured questionnaire was used for data collection. The questionnaire was developed based on a comprehensive literature review and consisted of four sections: Socio-demographic characteristics (10 questions), pregnancy history (6 questions), history of substance abuse (4 questions), and medical history, including Hepatitis B infection, vaccination, and medical interventions (12 questions). A trained research team member was assigned to collect the data through face-to-face interviews.
3.3. Statistical Analysis
Categorical variables were presented as counts and percentages. The characteristics of pregnant women with chronic Hepatitis B infection were compared with those without infection using chi-square and Fisher’s exact tests, as appropriate. A multiple logistic regression model was fitted using the forward likelihood ratio method to identify factors associated with chronic Hepatitis B infection in pregnant women. The final model included all predictive variables with a conservative significance level of ≤ 0.25 in the binary logistic regression models. A P-Value < 0.05 was considered significant for all analyses. SPSS version 23 statistical software (Chicago, IL) was used for data analysis.
4. Results
A total of 1,474 pregnant women participated in this study, with a mean age of 26.39 ± 0.17 years (range: 13 - 46 years). Overall, 24 (1.6%, 95% CI: 0.9% - 2.2%) of the pregnant women were HBsAg-positive. Among these HBsAg-positive mothers, 7 (29%) were aware of their HBV infection status, while 17 (71%) were unaware of their HBsAg seropositivity.
Of the 24 pregnant women who were HBsAg-positive at their first prenatal visit, 18 were available for repeat HBsAg testing at 24 - 28 weeks of gestation, and a quantitative HBV DNA viral load test was performed. Among the six women who did not continue with the study protocol, 2 had a gestational age beyond the study's age range, 2 declined the viral load test, 1 experienced a miscarriage, and 1 had a stillbirth; these individuals were excluded from the study.
The mean viral load in mothers infected with HBV was (11.1 ± 3.2) × 107 IU/mL. Based on the results, 16 (88.9%) of the HBsAg-positive women had viral loads lower than 200,000 IU/mL, while 2 (11.1%) had viral loads exceeding 200,000 IU/mL and required antiviral therapy.
As shown in Table 1, multiparous pregnant women were more likely to have HBV infection compared with nulliparous women (3.7% versus 0.5%). Similarly, a higher proportion of women with 3 or more children tested positive for HBsAg compared with women who had no children (3.5% versus 0.5%). Women with a family member incarcerated had a higher likelihood of contracting HBV infection compared with those without imprisoned family members (5.3% versus 1.4%). A larger fraction of women with high-risk sexual behaviors and those who had tattoos were infected with HBV. Among smoking pregnant women, 6.2% were HBsAg-positive, whereas only 1.3% of non-smoking pregnant women had HBV infection.
| Variables | HBsAg +; (n = 24) | HBsAg -; (n = 1450) | P-Value a |
|---|---|---|---|
| Age group (y) | 0.068 | ||
| < 25 | 5 (0.9) | 567 (99.1) | |
| ≥ 25 | 19 (1.3) | 883 (10.0) | |
| Age at marriage (y) | 0.868 | ||
| < 18 | 11 (1.7) | 640 (98.3) | |
| ≥ 18 | 13 (1.6) | 810 (98.4) | |
| Education | 0.610 | ||
| Illiterate | 6 (2.0) | 301 (98.0) | |
| Primary School and Higher | 18 (1.5) | 1149 (98.5) | |
| Occupation | 0.327 | ||
| Employed | 0 (0.0) | 29 (100.0) | |
| Housewife | 24 (1.7) | 1421 (98.3) | |
| Ethnicity | 0.086 | ||
| Balouch | 22 (1.9) | 1114 (98.1) | |
| Fars | 2 (0.6) | 336 (99.4) | |
| Polygynous spouse | 0.809 | ||
| Yes | 2 (1.1) | 175 (98.9) | |
| No | 22 (1.7) | 1275 (98.3) | |
| Parity | 0.005 | ||
| Nullipara | 2 (0.5) | 402 (99.5) | |
| 1 - 3 | 12 (1.5) | 789 (98.5) | |
| > 3 | 10 (3.7) | 259 (96.3) | |
| Number of children | 0.011 | ||
| 0 | 2 (0.5) | 414 (99.5) | |
| 1 - 3 | 13 (1.6) | 786 (98.4) | |
| > 3 | 9 (3.5) | 250 (96.5) | |
| Stillbirth | 0.286 | ||
| Yes | 3 (3.7) | 78 (96.3) | |
| No | 21 (1.5) | 1372 (98.5) | |
| Abortion | 0.297 | ||
| Yes | 3 (0.9) | 344 (99.1) | |
| No | 21 (1.9) | 1106 (98.1) | |
| Incarceration | 1.000 | ||
| Yes | 0 (0.0) | 18 (100.0) | |
| No | 24 (1.6) | 1432 (98.4) | |
| Incarceration of family members | 0.035 | ||
| Yes | 4 (5.3) | 72 (94.7) | |
| No | 20 (1.4) | 1378 (98.6) | |
| Tattooing | 0.049 | ||
| Yes | 4 (4.6) | 83 (95.4) | |
| No | 20 (1.4) | 1367 (98.6) | |
| High risk sexual behavior | 0.032 | ||
| Yes | 1 (50.0) | 1 (50.0) | |
| No | 23 (1.6) | 1449 (98.4) | |
| IV drug use | 1.000 | ||
| Yes | 0 (0.0) | 3 (100.0) | |
| No | 24 (1.6) | 1447 (98.4) | |
| Spouse IV drug use | 0.921 | ||
| Yes | 0 (0.0) | 5 (100.0) | |
| No | 24 (1.6) | 1445 (98.4) | |
| Smoking | 0.030 | ||
| Yes | 6 (6.2) | 90 (93.8) | |
| No | 18 (1.3) | 1360 (98.7) | |
| Spouse smoking | 0.084 | ||
| Yes | 7 (3.0) | 224 (97.0) | |
| No | 17 (1.4) | 1226 (98.6) |
a P-Value for chi square test.
Considering the past medical history of pregnant women (Table 2), a positive family history of HBV infection, particularly in first-degree relatives, a history of HBV infection in the mother, and a history of non-alcoholic fatty liver disease in the mother were significantly associated with maternal HBV infection (P < 0.05). However, no significant associations were found between maternal HBV infection and variables such as history of blood transfusion, dental and surgical procedures, endoscopy and colonoscopy procedures, phlebotomy, hemodialysis, sexually transmitted diseases, or HBV vaccination. Additionally, only 197 (13.3%) of the study participants were vaccinated against Hepatitis B.
| Variables | HBsAg +; (n = 24) | HBsAg -; (n = 1450) | P-Value a |
|---|---|---|---|
| Blood transfusion | 0.835 | ||
| Yes | 1 (4.3) | 22 (95.7) | |
| No | 23 (1.6) | 1428 (98.4) | |
| Dentistry Procedures | 0.379 | ||
| Yes | 8 (2.3) | 341 (97.7) | |
| No | 16 (1.4) | 1109 (98.6) | |
| Endoscopy | 1.000 | ||
| Yes | 0 (0.0) | 12 (100.0) | |
| No | 24 (1.6) | 1438 (98.4) | |
| Colonoscopy | 1.000 | ||
| Yes | 0 (0.0) | 3 (100.0) | |
| No | 24 (1.6) | 1447 (98.6) | |
| Phlebotomy | 0.070 | ||
| Yes | 2 (7.4) | 25 (92.6) | |
| No | 22 (1.5) | 1425 (98.5) | |
| Surgery | 0.061 | ||
| Yes | 7 (3.1) | 221 (96.9) | |
| No | 17 (1.4) | 1229 (98.6) | |
| Hemodialysis | 1.000 | ||
| Yes | 0 (0.0) | 3 (100.0) | |
| No | 24 (1.6) | 1447 (98.4) | |
| Sexually transmitted diseases | 0.083 | ||
| Yes | 9 (2.9) | 302 (97.1) | |
| No | 15 (1.3) | 1148 (98.7) | |
| History of Hepatitis B infection | < 0.001 | ||
| Yes | 7 (63.6) | 4 (36.4) | |
| No | 17 (1.2) | 1446 (98.8) | |
| Hepatitis B infection in family members | < 0.001 | ||
| Yes | 6 (12.5) | 42 (87.5) | |
| No | 18 (1.3) | 1408 (98.7) | |
| History of nonalcoholic fatty liver disease (NAFLD) | < 0.001 | ||
| Yes | 2 (15.4) | 11 (84.6) | |
| No | 22 (1.5) | 1439 (98.5) | |
| Hepatitis B vaccination | 0.760 | ||
| Yes | 2 (1.0) | 195 (99.0) | |
| No | 22 (1.2) | 1255 (93.8) |
a P-Value for chi square test.
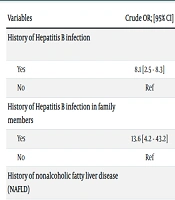
Multiple logistic regression analysis was performed to identify factors associated with HBV infection in pregnant women (Table 3). Pregnant women with a history of Hepatitis B infection had more than a 7-fold increased risk of contracting the infection compared to women without a history of HBV infections (OR = 7.7, 95% CI 1.1 - 5.3, P < 0.001). Similarly, a history of Hepatitis B infection in family members was associated with an 8-fold increase in the likelihood of HBV infection in pregnant women. A history of liver disease in pregnant women was also related to a 12.3-fold increase in the odds of contracting HBV infection. Compared with non-smoking mothers, pregnant women who were smokers were 5 times more likely to be HBsAg-positive (OR = 5.3, 95% CI 1.7 - 16.5, P < 0.010).
| Variables | Crude OR; [95% CI] | Adjusted OR; [95% CI] | P-Value |
|---|---|---|---|
| History of Hepatitis B infection | < 0.001 | ||
| Yes | 8.1 [2.5 - 8.3] | 7.7 [1.1 - 5.3] | |
| No | Ref | Ref | |
| History of Hepatitis B infection in family members | < 0.001 | ||
| Yes | 13.6 [4.2 - 43.2] | 8.3 [2.7 - 25.] | |
| No | Ref | Ref | |
| History of nonalcoholic fatty liver disease (NAFLD) | 0.005 | ||
| Yes | 11.8 [2.4 - 56.8] | 12.3 [2.1 - 70.4] | |
| No | Ref | Ref | |
| Smoking | 0.003 | ||
| Yes | 5.1 [1.9 - 13.0] | 5.3 [1.7 - 16.5] | |
| No | Ref | Ref |
5. Discussion
A total of 1,474 pregnant women who referred to the Central Laboratory of Zahedan Health Center were recruited to investigate the prevalence of HBV infection and associated risk factors among pregnant women. Results showed that the prevalence of HBV infection among pregnant women was 1.6%. This prevalence aligns with the results of systematic reviews and meta-analyses of epidemiological studies on HBV seroprevalence in Iran (6-8), and reflects a decrease from the 6.5% reported by Sharifi-Mood et al. in 2005 from Zahedan (16). However, the prevalence of HBV infection among pregnant women in Zahedan was significantly higher compared to other cities such as Isfahan (0.5%) (11) and Sari (0.2%) (12). Notably higher prevalence rates of HBV infection among pregnant women have been reported in Eastern Mediterranean and Middle Eastern countries, including Yemen (10.8%), Oman (7.1%), Sudan (5.6%), Jordan (4.3%), Tunisia (4%), Egypt (3.2%), Turkey (2.8%), Saudi Arabia (2.6%), and Pakistan (2%) (17). These differences may be partly explained by variations in HBV vaccination coverage, access to healthcare services, socioeconomic status, substance abuse, and the higher prevalence of chronic HBsAg carriers in the general population (15).
A family history of HBV infection was significantly associated with maternal HBV infection, with the presence of a first-degree relative with HBV infection increasing the risk by 8.3 times. High incidence of HBV infection is observed among household contacts of patients with HBV infection (12). A study showed that 19.3% of household members of HBV carriers in Zahedan were HBsAg-positive, and a higher proportion of mothers (53.2%) of index cases were positive compared to their fathers (8.4%) (18). Children have a higher chance of contracting the infection in families where the mother is HBsAg-positive compared to households where the father has HBV infection (19).
A novel finding in our study was that maternal tobacco use significantly increased the risk of HBV infection among pregnant women. Evidence suggests that smoking can accelerate disease progression in patients with Hepatitis B (20). In fact, 33.73% of age-standardized mortality and 34.52% of disability-adjusted life-years (DALYs) among Hepatitis B patients have been attributed to modifiable lifestyle factors such as smoking, alcohol consumption, and high BMI (20). Additionally, smoking adversely affects antibody responses to Hepatitis B vaccines, with a significant proportion of smokers failing to achieve protective antibody levels 3 months after vaccination, thereby increasing the risk of contracting the infection (21).
The results of this study demonstrated a significant association between a history of nonalcoholic fatty liver disease (NAFLD) in the mother and maternal HBV infection; the risk of HBV infection in mothers with fatty liver disease was 12 times higher than in those without it. NAFLD is the most common cause of chronic liver disease, affecting 25% of the world’s population (22). Although NAFLD results in significant liver inflammation, the relationship between NAFLD and HBV infection has not been well established (2).
In this study, 71% of HBsAg-positive pregnant women were unaware of their HBV infection status before enrollment. This finding is consistent with a study conducted in Zahedan in 2005, which reported that 61% of study participants were unaware of their HBV infection status until informed during the study period (16).
We found that only 13.3% of the pregnant women were vaccinated against Hepatitis B. This aligns with a systematic review and meta-analysis that reported HBV immunization coverage (receiving at least one dose of the HBV vaccine) among Iranian pregnant women was 9.8% (7). Another systematic review and meta-analysis reported HBV vaccination coverage in seven studies ranged from 0.8% to 22.8% (8). Additionally, a similar review estimated that only 40% of pregnant women achieved anti-HBs concentrations of >10 IU/mL after vaccination (6).
Hepatitis B can be transmitted through practices such as risky sexual behavior and tattooing. In the univariate analysis of our study data, the risk of developing HBV infection was significantly associated with a previous history of high-risk sexual behavior and tattooing. However, no significant relationship was observed between these risk factors and HBsAg seropositivity in the multivariate regression analysis. This finding is consistent with systematic reviews and meta-analyses of studies on risk factors for Hepatitis B infection among pregnant women in Iran, which found no relationship between tattooing and HBV infection (6, 7). Conversely, a study on the prevalence of HBsAg and high-risk behaviors in pregnant women in Isfahan Province, Iran, reported that a history of high-risk sexual behaviors and tattooing was significantly associated with an increased risk of contracting HBV infection (11).
In conclusion, our study results indicate a relatively high prevalence of HBV infection among pregnant women in southeastern Iran, with the majority of HBV-positive pregnant women unaware of their infection status.