1. Background
A growing number of the global population is aging; accordingly a higher number of elderly patients are hospitalized for various causes. According to several studies (1-3) conducted in this population, age is a risk factor for acquiring nosocomial infections with a subsequent higher mortality rate compared to younger patients. Meanwhile another study (4) found no significant difference between elderly patients and younger population.
The available studies on this subject are mostly based on European population (1, 2, 5-7), and those studies on Latin ethnicity (4) were conducted using a smaller number of patients.
2. Objectives
This study aimed to describe the incidence, type, and microbiological characteristics of nosocomial infections, among elderly and non-elderly patients.
3. Patients and Methods
3.1. Setting
This retrospective study was performed from January 2013 to December 2013 at the University Hospital “Dr. Jose Eleuterio Gonzalez” tertiary care hospital with 450 beds that provides medical attention to an open population in Monterrey, Northeastern region of Mexico.
3.2. Study Population
During the study period, all hospitalized patients were included in the nosocomial surveillance for hospital-acquired infections. We eliminated from the study all patients under the age of 18. Patients were stratified in two groups; non-elderly, including all patients with an age range of 18 - 64 years and elderly, including all patients older than 64 years.
All patients with diagnosis of a hospital-acquired infection were further studied for type of the infection, microbial diagnosis, hospital stay, and mortality.
3.3. Definitions
A nosocomial infection was defined by the site of infection using diagnostic criteria from the Center for Disease Control (CDC) (8). Hospital epidemiological surveillance was performed based on CDC and WHO recommendations (9).
3.4. Case Surveillance and Diagnosis of HAI
The infection control unit includes infectious disease specialists, a hospital epidemiologist, doctors and nurses trained in infection control. All cases of suspected HAI were detected by experienced personnel from the infection control unit and were later discussed with the rest of the unit’s staff for a definitive classification.
3.5. Statistical Analysis
A descriptive analysis was performed using basic parametric test. The Student t-test was used for numerical variables and Chi-square or Fisher exact test for analyzing categorical variables. P < 0.05 was considered statistically significant.
4. Results
Over the study period, 18469 patients were hospitalized with a total of 108555 hospital days. Of those patients, 15796 patients belonged to non-elderly and 2673 to elderly group.
In the elderly population, the primary diagnoses for hospitalization were as follow: cardiovascular (coronary artery disease, cerebral-vascular disease), 17.8%; malignant tumor related illness, 12.9%; trauma and orthopedic related diagnoses, 8.1%; diabetes related complications, 4.8%; and respiratory diseases, 3.6%. For the non-elderly patients, the primary diagnoses were as follows: obstetrics and or pregnancy related: 39.3%; abdominal surgeries: 10.1%; accidents related diagnoses: 8.3%; malignant tumor related illness: 6.8%; and respiratory tract diseases: 2.2%.
We recorded a total of 862 HAIs (79.6% in non-elderly patients and 20.3% in elderly patients) with an overall higher infection rate in the elderly group (6.54 HAI per 100 admissions) versus the non-elderly (4.34 HAI per 100 admissions) group (Table 1).
aDifference between this two groups P < 0.0001.
bDifference between this two groups P < 0.0442.
When comparing both groups with a specific type of hospital acquired infection, we found that ventilator-associated pneumonia (VAP), secondary bacteremia (SB), and catheter associated urinary tract infections (CA-UTI) had a higher incidence in the elderly group compared to the non-elderly group ( 0.67 vs. 1.20 per 1000 ventilator-days for VAP, P = 0.023; 0.23 vs. 0.67 per 1000 catheter-days for SB, P = 0.002; and 1.74 vs. 2.66 per 1000 catheter-days for CA-UTI, P = 0.010) (Table 2).
| Variable | Non-Elderly | Elderly | Total | P | |||
|---|---|---|---|---|---|---|---|
| No. (%) | Infection Rate Per 1000 p-d | No. (%) | Infection Rate Per 1000 p-d | No. (%) | Infection Rate Per 1000 p-d | ||
| Ventilator-associated pneumonia | 60 (8.7) | 0.670 | 23 (13.1) | 1.202 | 83 (9.6) | 0.764 | 0.023 |
| Pneumonia | 20 (2.9) | 0.223 | 5 (2.9) | 0.261 | 25 (2.9) | 0.230 | 0.960 |
| Other respiratory tract infections | 4 (0.6) | 0.044 | 1 (0.6) | 0.052 | 5 (0.6) | 0.046 | 0.888 |
| Primary bacteremia | 46 (6.7) | 0.514 | 8 (4.6) | 0.418 | 54 (6.3) | 0.497 | 0.717 |
| Secondary bacteremia | 20 (2.9) | 0.223 | 13 (7.4) | 0.679 | 33 (3.8) | 0.304 | 0.002 |
| Central line-associated bloodstream infections | 62 (9) | 0.693 | 16 (9.1) | 0.836 | 78 (9) | 0.718 | 0.602 |
| Intravascular catheter insertion site infection | 49 (7.1) | 0.547 | 11 (6.3) | 0.575 | 60 (7) | 0.552 | 0.884 |
| Catheter-associated urinary tract infection | 156 (22.7) | 1.744 | 51 (29.1) | 2.666 | 207 (24) | 1.906 | 0.010 |
| Urinary tract infection | 15 (2.2) | 0.167 | 6 (3.4) | 0.313 | 21 (2.4) | 0.193 | 0.302 |
| Surgical site infection | 196 (28.5) | 2.191 | 28 (16) | 1.463 | 224 (26) | 2.063 | 0.054 |
| Skin and soft tissues infections | 27 (3.9) | 0.301 | 5 (2.9) | 0.261 | 32 (3.7) | 0.294 | 0.948 |
| Eye infections | 1 (0.1) | 0.011 | 2 (1.1) | 0.104 | 3 (0.3) | 0.027 | 0.141 |
| Peritonitis | 3 (0.4) | 0.033 | 0 (0) | 0.000 | 3 (0.3) | 0.027 | 0.965 |
| Gastrointestinal infections | 23 (3.3) | 0.257 | 6 (3.4) | 0.313 | 29 (3.4) | 0.267 | 0.849 |
| Other | 5 (0.7) | 0.055 | 0 (0) | 0.000 | 5 (0.6) | 0.046 | 0.654 |
| Total | 687 (100) | 7.682 | 175 (100) | 9.148 | 862 (100) | 7.940 | 0.044 |
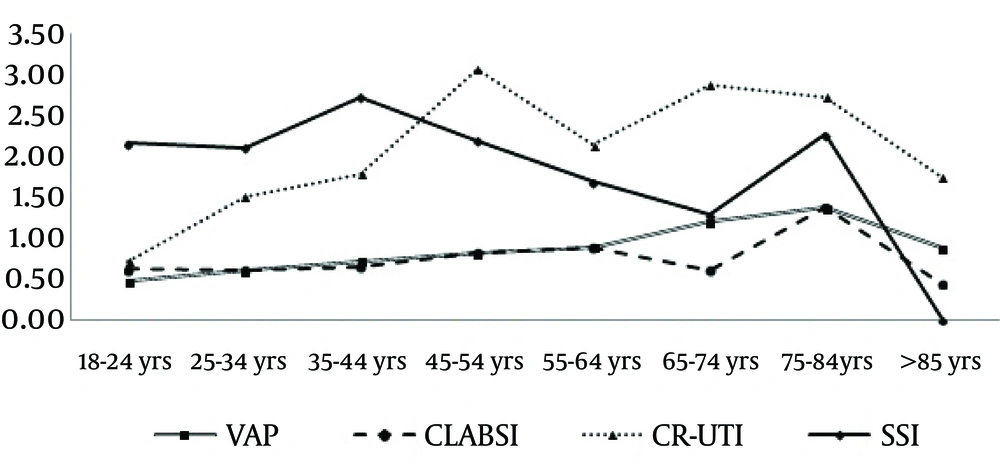
Rates of VAP, CA-UTI, and central line associated bloodstream infection (CLABSI) had an increasing tendency as aged groups progressed and surgical site infection (SSI) had a decreasing tendency. Although in the 75 - 84 age group HAI rates had an increase, the rates were lower in the > 85 years group (Figure 1).
More than two-thirds (67.3%) of the isolates in the whole study group were Gram-negative bacteria while Gram-positive bacteria were reported in only 25.9% of the isolates. The elderly group had a higher frequency of positive cultures for Gram-negative bacteria, particularly Klebsiella spp. and fungal infections (P > 0.05). Clostridium difficile infection rate was not different between both age groups (Table 3).
| Microorganisms | Non-Elderly | Elderly | Total | P |
|---|---|---|---|---|
| Gram-negative | 420 (67.4) | 90 (66.7) | 510 (67.4) | |
| Escherichia coli | 59 (9.5) | 15 (11.1) | 74 (9.8) | 0.209 |
| Pseudomonas spp. | 103 (16.5) | 23 (17) | 126 (16.6) | 0.278 |
| Klebsiella spp. | 62 (10) | 20 (14.8) | 82 (10.8) | 0.016 |
| Acinetobacter spp. | 107 (17.2) | 18 (13.3) | 125 (16.5) | 0.981 |
| Proteus spp. | 10 (1.6) | 0 (0) | 10 (1.3) | 0.394 |
| Enterobacter spp. | 24 (3.9) | 6 (4.4) | 30 (4.0) | 0.547 |
| Stenotrophomonas maltophilia | 7 (1.1) | 1 (0.7) | 8 (1.1) | 0.874 |
| Citrobacter spp. | 8 (1.3) | 0 (0) | 8 (1.1) | 0.508 |
| Morganella morganii | 8 (1.3) | 2 (1.5) | 10 (1.3) | 0.962 |
| Providencia spp. | 21 (3.4) | 3 (2.2) | 24 (3.2) | 0.783 |
| Serratia spp. | 8 (1.3) | 2 (1.5) | 10 (1.3) | 0.962 |
| Other Gram-negative | 3 (0.5) | 0 (0) | 3 (0.4) | 0.476 |
| Gram-positive | 164 (26.3) | 32 (23.7) | 196 (25.9) | |
| Enterococcus spp. | 66 (10.6) | 14 (10.4) | 80 (10.6) | 0.540 |
| Coagulase-negative staphylococci | 20 (3.2) | 2 (1.5) | 22 (2.9) | 0.678 |
| Staphylococcus aureus | 47 (7.5) | 10 (7.4) | 57 (7.5) | 0.637 |
| Streptococcus spp. | 8 (1.3) | 0 (0) | 8 (1.1) | 0.508 |
| Clostridium difficile | 23 (3.7) | 6 (4.4) | 29 (3.8) | 0.436 |
| Yeast | 39 (6.3) | 13 (9.6) | 52 (6.9) | |
| Candida spp. | 39 (6.3) | 13 (9.6) | 52 (6.9) | 0.049 |
| Total | 623 (100) | 135 (100) | 758 (100) |
aValues are presented as No. (%)
Overall, in-hospital mortality in patients with HAI was statistically lower in the non-elderly population 20.5% vs. 38.5% in elderly group (OR 0.41, 95% CI; 0.27 - 0.62, P < 0.0001). In-hospital mortality increased in association with the number of HAIs diagnosed per patient, but it only reached statistical significance when only 1 HAI was diagnosed. In patients diagnosed with only 1 HAI, the mortality rate was 14.2% in the non-elderly vs. 30.8% in the elderly group (OR 2.69, 95% CI; 1.60 - 4.52, P = 0.0002). When 2 HAIs were diagnosed in the non-elderly group the mortality rose to 37.8% vs. 54.5% in the elderly group (OR 1.97, 95% CI; 0.75 - 5.15, P = 0.166). Finally, when 3 or more HAIs were diagnosed, the mortality rose to 52.5% vs. 72.2% in the elderly group (OR 2.4, 95% CI; 0.55 - 10.4, P = 0.23). Unlike the patients without HAI (by age group), all groups showed differences in higher probability of in-hospital deaths (Table 4).
| Non-Elderly | Elderly | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 28 Day-Mortalityb | Alive at Dischargeb | OR | 95% CI | P | 28 Day-Mortalityb | Alive at Dischargeb | OR | 95% CI | P | |
| 1 HAI vs. No HAI | 14.20 | 85.70 | 6.39 | 4.75 to 8.59 | 0.0001 | 30.80 | 69.10 | 4.21 | 2.66 to 6.64 | 0.0001 |
| 2 HAI vs. No HAI | 37.80 | 62.10 | 23.47 | 14.51 to 37.96 | 0.0001 | 54.50 | 45.40 | 11.32 | 4.84 to 26.47 | 0.0001 |
| > 3 HAI vs. No HAI | 52.50 | 47.50 | 42.62 | 22.73 to 79.94 | 0.0001 | 72.70 | 27.20 | 25.15 | 6.63 to 95.45 | 0.0001 |
aAbbreviation: HAI: hospital-acquired infection.
bValues are presented based on %.
5. Discussion
In the present study, the HAI rate per 100 admissions and per 1000 patient days was greater in the elderly group (P < 0.0001 and P = 0.04, respectively); these results are similar to other reports assessing the same topic (2, 3). Whereas, a Brazilian study showed discordant data (4) in which no significant difference was found between both groups, which was probably due to the small number of patients analyzed.
We found that the most common types of HAIs were SSI, CA-UTI, VAP, and CLABSI. Similar to our results, Avci et al. (2) reported a higher incidence of urinary tract infections, respiratory tract infections, surgical site, skin and soft tissue infections, per 1000 patient days in the elderly group. A study on critically ill patients found that bloodstream infections were less frequent in patients aged 85 and older compared to the younger patients and there were no significant difference in the other types of infection (10). Another study on postoperative patients reported no statistically significant difference between young and elderly patients (7).
Stephan et al. found an increased incidence of pneumonia, SSI, ITU, bacteremia, and catheter-associated infection in the 60 - 75 age group (the younger group of the population analyzed) and a decreased incidence in the age group of older than 75 years. These results were similar to those obtained in our study, in which we observed that in 85 years and older group, the major HAIs in our hospital (VAP, CLABSI, CR-UTI, SSI) had a lower incidence, which was probably due to fewer number of invasive procedures in this age group (7).
The most frequent microorganisms isolated were Gram-negative bacteria with a greater incidence in the elderly group (P = 0.03). This finding was also described by Dimopoulos et al. (10) reporting that Gram-negative microorganisms were more frequent in patients aged 85 and older than in all groups younger than 75. They found no significant statistical differences in the frequencies of Gram-positive microorganisms and fungi infections, opposite to our study in which we observed a greater incidence in the fungi infections in the elderly (P = 0.0085).
In this study, the 28 day-mortality in patients with HAIs was higher compared to patients that did not developed HAI in both the elderly and non-elderly groups; this issue has been reported in other studies (11).
According to several studies, elderly patients are associated with an increased mortality rate (2, 3, 5-7, 10). Similar to these, in our hospital the overall mortality in patients with HAIs was statistically higher in the elderly group (P < 0.0001). We acknowledge limitations to our study such as the difference in the primary diagnosis and comorbidities between the groups which made the comparison cumbersome.
In sum, we conclude that HAIs were more frequent in the elderly population predominately with respect to VAP and Gram-negative isolates. Mortally was higher in the elderly population although the associated risk was higher in the younger patients with every diagnosed HAI.