Dear Editor,
Cytomegalovirus (CMV) infection occurs in up to 36% of all critically ill patients, mostly between 4 and 12 days after admission to an intensive care unit (ICU) (1). The effectiveness of treatment for CMV pneumonia in ICU patients remains undefined. We report on a case of difficult-to-treat, life-threatening nosocomial pneumonia caused by CMV in a patient with chronic kidney disease (CKD) and a prolonged hospital stay.
A 66-year-old man presented with diabetes mellitus and chronic kidney disease. Despite taking his regular medication, he had been suffering from a shortness of breath for three days. He was brought to the emergency department on September 8, 2014. Laboratory data showed a white-blood cell (WBC) count of 15300/μL with segment 88%; platelet count, 33400/μL; creatinine, 7.51 mg/dL and K, 6.34 mEq/L. Arterial blood gas analysis showed metabolic acidosis with PH, 7.436; PCO2, 18.3 mmHg; PO2, 153 mmHg; HCO3, 12.4 mmol/L and base excess, −10.3 mmol/L. Emergent hemodialysis was done. He was then transferred to the ward, and regular hemodialysis was maintained.
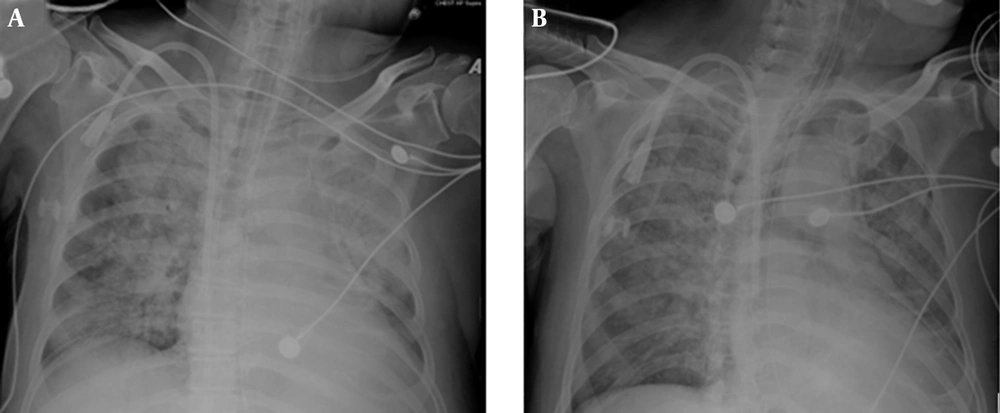
Due to a change in his consciousness, a brain computed tomography was performed, and a small, deep, old infarct was noticed. He was transferred to the ICU on October 12, 2014. Intubation was performed due to dyspnea and respiratory failure. Antibiotic therapy with cefpirome and vancomycin was given. However, CXR showed a progression of mixed airspace and interstitial infiltration over bilateral lungs (Figure 1 A). Sputum culture showed Pseudomonas aeruginosa without resistance to ceftazidime and cefpirone. Laboratory data showed a WBC count of 1600/μL with segment 62%; bandemia, 29%; platelet count, 3400/μL and C-reactive protein, 231 mg/L. As severe sepsis was in progress, antibiotic therapy was shifted to meropenem.
On October 14, 2014, blood and sputum CMV-PCR results showed positive and the patient’s CMV viral load was positive but with a low titer of < 137 IU/mL. Aspergillus Ag index showed 0.15 (negative). Ganciclovir was given then. Unstable blood pressure was noted. CXR still showed mixed alveolar and interstitial infiltration over both lungs (Figure 1 B). Arterial blood gas analysis showed pH, 7.324; PCO2, 42.9 mmHg, PO2, 63.7 mmHg, HCO3, 22.5 mmol/L, base excess, −2.8 mmol/L and a P/F ratio of 75.1 mmHg, suggesting adult respiratory distress syndrome. Profound shock then developed, requiring high-dose vasopressors. His condition deteriorated despite aggressive treatment. Family members requested palliative therapy, and the patient expired on October 24, 2014.
CMV is a virus that infects both normal and compromised hosts. In normal hosts, CMV presents most often as an “infectious mononucleosis-like” illness. CMV reactivation usually occurs in immunocompromised patients, such as patients with cancer, post-organ transplantation, or human immunodeficiency virus infection (2). In compromised hosts, CMV can presents as community-acquired pneumonia, encephalitis, retinitis, hepatitis, or colitis (3). CMV infection may occur in non-immunocompromised critically ill patients hospitalized in intensive care units (4). Prolonged hospital stay with severe disease may cause immune dysfunction in our case, thus nosocomial CMV infection developed. Possibly, early detection and treatment for CMV nosocomial pneumonia could avoid poor clinical outcome. Although the patient did not have cancer, organ transplantation and acquired immune deficiency syndrome, we suggested that CMV should be considered as an etiology in a CKD patient with poorly responsive nosocomial pneumonia.
In conclusion, although not commonly seen in nosocomial pneumonia, cytomegalovirus should be considered among patients with chronic kidney diseases and prolonged hospital stay when they develop delayed-onset nosocomial pneumonia. Importantly, CMV pneumonia may (manifest) as rapidly progressive adult respiratory distress syndrome and result in fatal outcome if timely specific treatment is not initiated.
Ethical approval: The above study has been granted exemption from review by the institutional review board of Chi Mei Medical Center (no.10404-E03).