1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2), has resulted in millions of confirmed cases and deaths worldwide (1). A primary complication in patients with severe illness is acute respiratory distress syndrome, which often requires oxygen therapy and mechanical ventilation. Encephalopathy is also commonly observed in critically ill patients, with ICU-related delirium contributing to reduced overall survival. Other neurological complications, including seizures, ataxia, and motor or sensory deficits, have also been documented (2). Acute necrotizing encephalopathy (ANE) is a specific form of necrotizing lesion affecting brain parenchyma. There are two types of ANE cases reported: (1) the isolated and (2) sporadic type, which is typically triggered by viral infections, particularly influenza and HHV-6, and the familial recurrent type, which is associated with mutations in the RANBP2 gene (3). Although rare, ANE has been identified as a neurological complication associated with COVID-19 (4). Here, we present a rare case of altered consciousness due to COVID-19-related acute necrotizing encephalitis, initially misdiagnosed as opium poisoning. Although the peak of the coronavirus pandemic has passed, cases continue to arise with significant neurological side effects.
2. Case Presentation
A 29-year-old female patient was brought to the emergency department with the chief complaint of loss of consciousness. The patient had been in good health until two days prior to admission, after which she experienced progressive weakness, lethargy, nausea, vomiting, and fever, culminating in a loss of consciousness. The patient’s medical and family histories were non-contributory, with no reported cases of SARS-CoV-2 infection among family members. Her medications included unidentified drugs for obesity.
Initial vital signs showed some abnormalities: BP 85/55 mmHg, PR 84 bpm, RR 15 breaths per minute, and T 39.5°C. Her oxygen saturation was critically low at 70% on room air. On physical examination, the patient was unconscious, disoriented to time and place, and unable to follow commands. She exhibited no cyanosis or jaundice, with a Glasgow Coma Scale (GCS) score of < 8. Neurological examination revealed pinpoint pupils with minimal reactivity to light. Auscultation of the lungs indicated rales and diminished sounds at the bases.
Laboratory evaluations, including blood glucose, complete blood count, liver function tests, electrolytes, and erythrocyte sedimentation rate, were within normal ranges. However, her C-reactive protein was elevated at 2+. Toxicology screening for urine and blood was negative, as were tests for troponin and BHCG. Urine and blood cultures were performed three times, with negative results in each case. Respiratory alkalosis (pH 7.45, PCO2 32.6) was identified in her venous blood gas analysis. A lumbar puncture (LP) was conducted, showing no signs of infection in the cerebrospinal fluid (CSF), with both CSF culture and PCR for HSV returning negative.
Initial management included intubation and hydration. Further diagnostics, including electrocardiogram (ECG), electroencephalogram (EEG), echocardiogram, chest X-ray (CXR), chest Computed tomography (CT-scan), and cerebral CT angiography, were conducted. Electroencephalogram, echocardiography, CXR, CT scan, and CT angiography results were all normal. Electroencephalogram showed generalized slowing, though no seizure activity was detected.
Due to the patient's decreased level of consciousness and pinpoint pupils (miosis), suspicion of opium poisoning was raised, and naloxone treatment was initiated. However, the patient showed no response to naloxone. Given the possibility of brain lesions, a brain CT scan was performed, which revealed no abnormalities. The patient remained under observation for 3 - 4 days with no change in her condition.
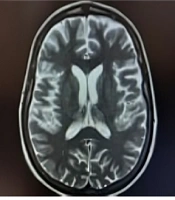
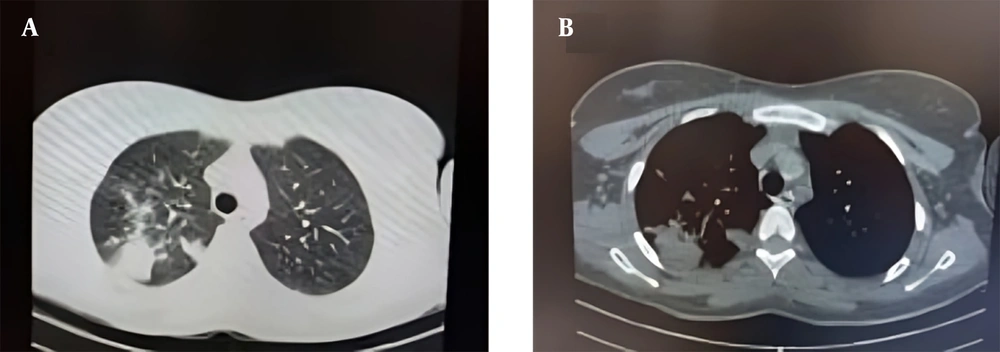
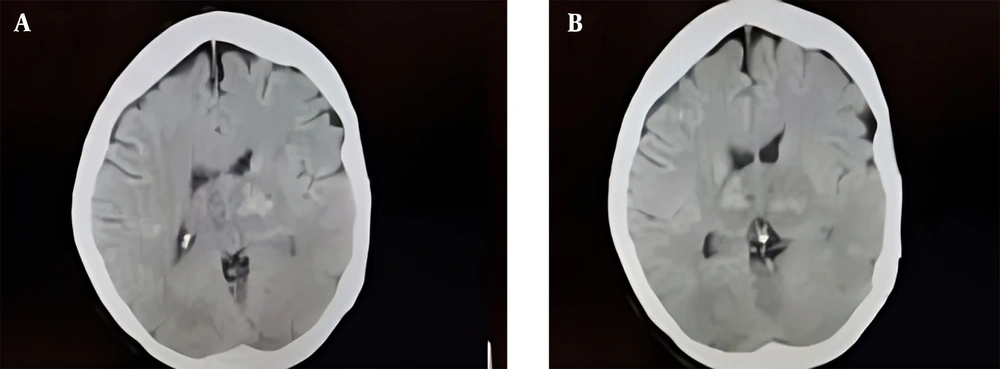
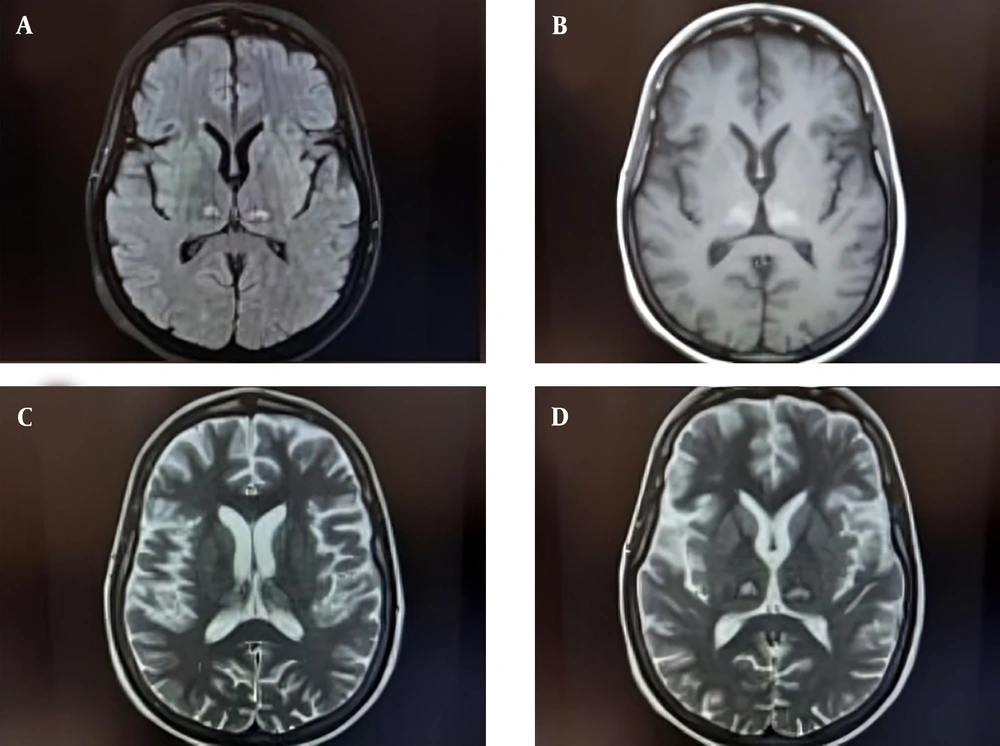
At a follow-up evaluation on day 4 after admission, sedatives were discontinued, but her level of consciousness did not improve. Consequently, a second chest and brain CT scan were ordered. The chest CT scan revealed bilateral ground-glass opacities (GGO) and right-sided consolidation (Figure 1), while the brain CT scan is shown in (Figure 2). Based on the findings from the brain CT, which showed evidence of cerebral hemorrhage, a brain MRI was performed (Figure 3). Additionally, PCR testing for COVID-19 via nasopharyngeal swab returned positive.
With the positive COVID-19 PCR result and imaging findings, a diagnosis of COVID-19-related acute necrotizing encephalitis became the most probable scenario. During her hospitalization, the patient was treated with glucocorticoid pulse therapy combined with intravenous immunoglobulin (IVIG) and supportive care. Eventually, she was discharged with persistent neurological deficits, including athetosis, bilateral dystonia, and quadriplegia, though her symptoms were improving gradually. Written informed consent was obtained from the patient for the publication of this case report.
3. Discussion
Encephalopathy is a term used to describe alterations in brain function, ranging from agitation to confusion, and is associated with both hyperactive and hypoactive delirium. Encephalopathy is one of the most common severe neurological manifestations of COVID-19 infection, with its frequency increasing alongside illness severity (5).
Numerous instances of ANE have been documented in association with SARS-CoV-2. A hallmark of this condition is the presence of multiple, symmetrically distributed lesions—sometimes with accompanying hemorrhages—in various regions of the brain, including the thalamus, basal ganglia, brainstem, and subcortical white matter (6). One report describes a 5-month-old infant who, after developing a fever and experiencing two seizure episodes, was diagnosed with COVID-19-associated acute necrotizing encephalitis, suggesting brain infection (7). In another case, SARS-CoV-2 was detected in brainstem tissue (8). A separate study reported a 70-year-old man who presented with generalized tonic-clonic seizures and confusion, and MRI revealed edematous changes in the thalami, brainstem, and cerebellar peduncles, along with micro-hemorrhages (9). In contrast, our case of ANE manifested with loss of consciousness and meiotic pupils, initially misdiagnosed as opium poisoning, resulting in delayed appropriate treatment.
Most cases of ANE are parainfectious, triggered by viral infections such as influenza-A, influenza-B, parainfluenza, varicella, herpes simplex virus, human herpesvirus-6 (HHV-6), HHV-7, enterovirus, rotavirus, measles, rubella, coxsackie-A9, and dengue virus, with influenza virus and HHV-6 being the most common (10). Symptoms of ANE from different viral infections include fever, upper respiratory tract symptoms, gastroenteritis, erythema, seizures, disturbed consciousness, and focal neurological deficits. Patients with ANE may also exhibit signs of systemic inflammatory response syndrome (SIRS), including shock, multiple organ failure, and disseminated intravascular coagulation (11, 12). There are two main theories regarding COVID-19’s impact on the brain. The first suggests that the virus directly infects brain tissue, as the same receptors it uses to attach to the lungs are also present in the central nervous system. Viral antigens have been detected in brain samples and CSF, supporting this theory. The second theory posits that COVID-19’s hyper-inflammatory state impacts the immune system, leading to an autoimmune or immune-mediated response. This state can trigger the release of cytokines and chemokines that increase blood-brain barrier permeability and initiate neuro-inflammatory cascades (13, 14). The progression of ANE may be controlled, and prognosis improved, if glucocorticoid pulse therapy combined with gamma globulin injection is initiated promptly (15).
MRI findings in the present case revealed involvement of both the thalami and diencephalon. One potential diagnosis considered was pons ischemia; however, this was ruled out as the MRI showed no evidence of pons infarction. The pinpoint pupils were attributed to diencephalic involvement, while the decreased level of consciousness was due to bilateral thalamus involvement. These symptoms were initially mistaken for opium poisoning.
This case highlights the complexity of COVID-19, as the disease can present with a wide range of symptoms, often resembling other conditions. Early detection and prompt treatment of ANE in COVID-19 patients may significantly improve clinical outcomes, particularly given the association between ANE and severe infections.
3.1. Conclusions
COVID-19 infection can lead to a wide range of clinical symptoms and complications, which may be mistaken for other illnesses. One such complication is ANE, a severe condition that can arise as a result of COVID-19. Early diagnosis of ANE is essential for timely and effective treatment, which may improve patient outcomes and prevent long-term neurological deficits.