1. Background
Intestinal parasites are considered as a major public health problem worldwide especially in developing countries. An estimated 3.5 billion people are affected and approximately 450 million individuals currently suffer from these infections, which most of them constitute children. Protozoa and helminthes are 2 categories of pathogenic and non-pathogenic parasites that cause gastrointestinal tract ailments (1). Intestinal parasitic infections (IPIs) is commonly transmitted by both indirect and direct routes via oral-fecal, ingestion of contaminated food, vegetables, and drinking water (2-5). In addition some flies might have a role as mechanical vectors for some intestinal parasites such as Ascaris lumbricoides, Hymenolepis nana, Entamoeba histolytica/dispar, and Giardia lamblia (6). Despite great efforts and improving the hygiene status in order to eliminate the intestinal parasites, these infectious agents are still common in many areas throughout the world. Pathogenesis, morbidity, and mortality of intestinal parasites are depending upon species, climate, age, gender, immune system condition, nutritional status of the host, and differ from person to person (1). IPIs in the majority of cases are asymptomatic; however, it can cause a wide spectrum of clinical symptoms such as: chronic diarrhea, watery diarrhea or mucoidal, nausea, vomiting, dehydration, abdominal pain, fever, iron deficiency anemia, malnutrition, and vitamin deficiencies that may lead to malabsorption syndrome, growth retardation in children, mental, and physical health disorders (1, 5, 7) after a long period. In immunocompromised individuals symptoms are more severe and may cause irreparable consequences (8).
Numerous investigations in various parts of the world have confirmed a direct correlation among the high rate of parasitic infections and lower socioeconomic status of the area. Furthermore, poor sanitary and environmental statuses are other critical epidemiological factors relevant with the prevalence of these infectious agents (1, 9, 10). Recently, many studies throughout the country of Iran have been performed and demonstrated a significant reduction in human helminthic disease compared with previous studies, although intestinal protozoan infection like Entamoeba spp., G. lamblia, and Blastocystis hominis are still prevalent (11-13). High rate of parasitic infections, especially in small towns and rural areas justified with a low hygienic status, illiteracy, social and economic poverty, defects in healthcare system, as well as a lack of safe drinking water filtration system (1, 9).
From intestinal protozoan infections, G. lamblia is the common infection with a prevalence ranging from 20% - 30% in developing countries and 2% - 5% in developed countries that affected about 200 million individuals throughout the world (14). In addition, E. histolytica, agent of amoebiasis, is another IPIs that affects about 180 million indiviuals worldwide and responsible for 40000 - 110000 mortality annually. E. histolytica and E. dispar are absolutely similar and cannot be distinguished by conventional microscopic examination. The first is a potential pathogen, while latter is a non-pathogen protozoa (15). Among helminthic infections, A. lumbricoides is still one of the most prevalent IPIs with 807 - 1221 million cases worldwide especially in sub-Saharan Africa and East Asia. In addition hookworm and whipworm (Trichuris trichiura) are liable for 576 - 740 million and 604 - 795 infections, respectively (16). Prevalence of intestinal parasites in different parts of Iran is varied from 9.1% in Mazandaran province (North Iran) (17), 21.2% in Tehran city (North Iran) (11), 7.6% in Kashan city (Central Iran) (18), and 35.1% in Hamadan city (12). It is noteworthy that climatic conditions are a key factor for prevalence of IPIs all around Iran (9).
2. Objectives
During the time, distribution patterns and prevalence of intestinal parasitic diseases fluctuate as a result of changing in behavior and life style of society population. Hence, periodic epidemiological surveys, in order to determine the exact burden of infection in region and adopting suitable strategies, is required and should be continued. Thus the aim of the current survey was to describe the prevalence of IPIs in individuals referred to central health center in Haftkel district, located at southwest of Iran.
3. Methods
3.1. Study Area
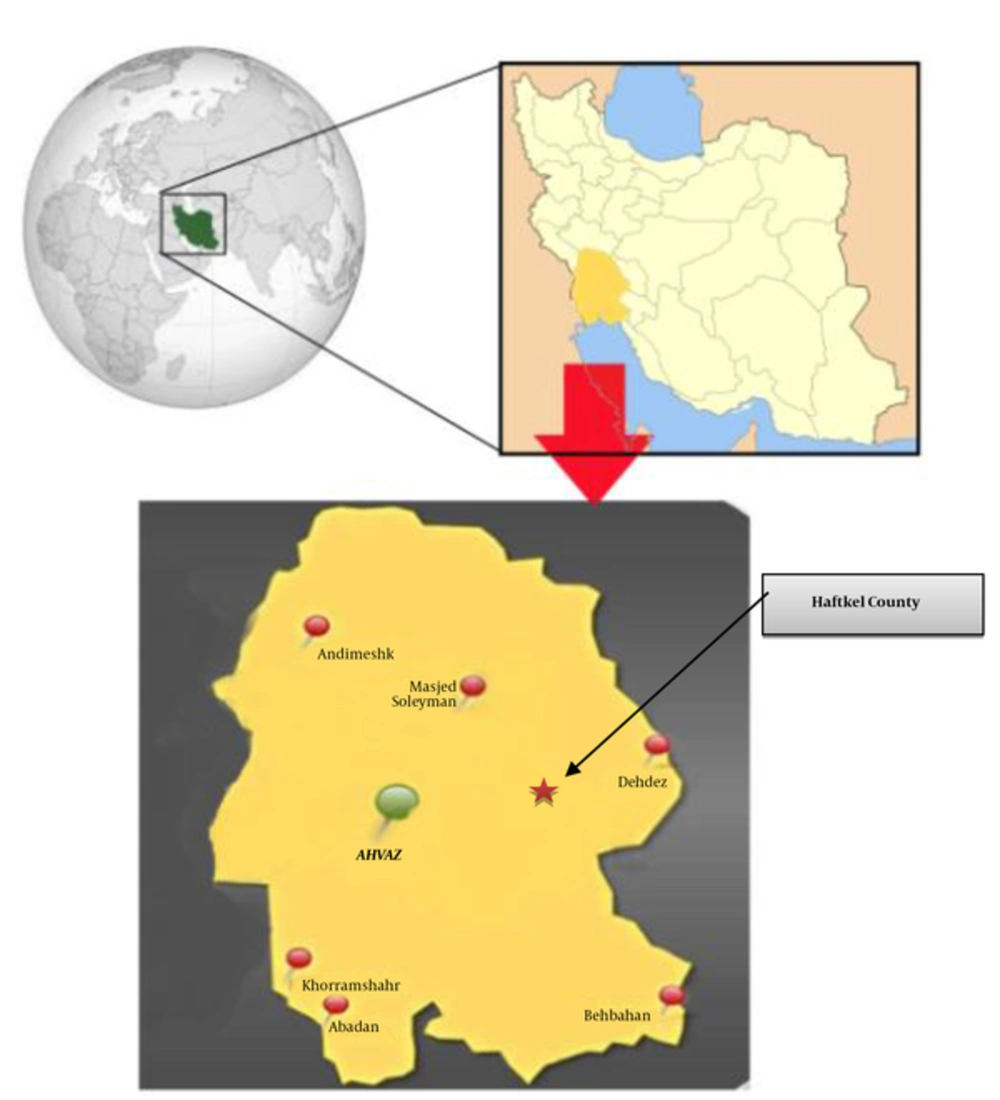
Haftkel County is located in southwest Iran (east of Khuzestan province) (Figure 1). Based on the 2011 census, the county’s population estimated 22391 people in 5399 families included both rural (7514 people) and urban (14,77 people) areas. The climate of Haftkel is generally hot and occasionally humid, while winters are much more pleasant and dry. Summertime temperatures routinely exceed 50°C and in the winter, it can drop below freezing point. The annual average rainfall is about 380 mm.
3.2. Study Population
This descriptive cross-sectional study was carried out in the laboratory of the central health center of Haftkel County during 4 r consecutive years (2010 - 2013). The study population included all individuals who were referred to laboratory the for s parasitology stool exam request.
3.3. Stool Examination
Stool specimens (1 - 4 g) were taken in labeled plastic containers without any preservatives and less than 1.5 hours after collecting underwent examination. For all samples, both direct smear and formalin ether concentration methods were done. Direct wet-mount smear was carried out to detect parasites motility using saline and lugol’s iodine solution. The formalin ether concentration technique was performed. Briefly, a piece of stool (0.5 - 1.5 g) was mixed with 4 g formol saline. Mixture passed through filter and then diethyl ether was added and mixed again. Mixture centrifuged by 3000 rpm for 2 minutes. Finally sediments after staining with 0.85% iodine, was placed on a clean slide, and were examined by a light microscope (× 100 magnification) in order to parasite detection. The diagnosis of helminth and protozoa was based on microscopic morphological features such as trophozoite size, cyst, and ova shape.
3.4. Statistical Analysis
Data analysis was done using SPSS version 11.0.1 (SPSS Inc., Chicago, IL, USA) software and Chi-square statistical test.
4. Results
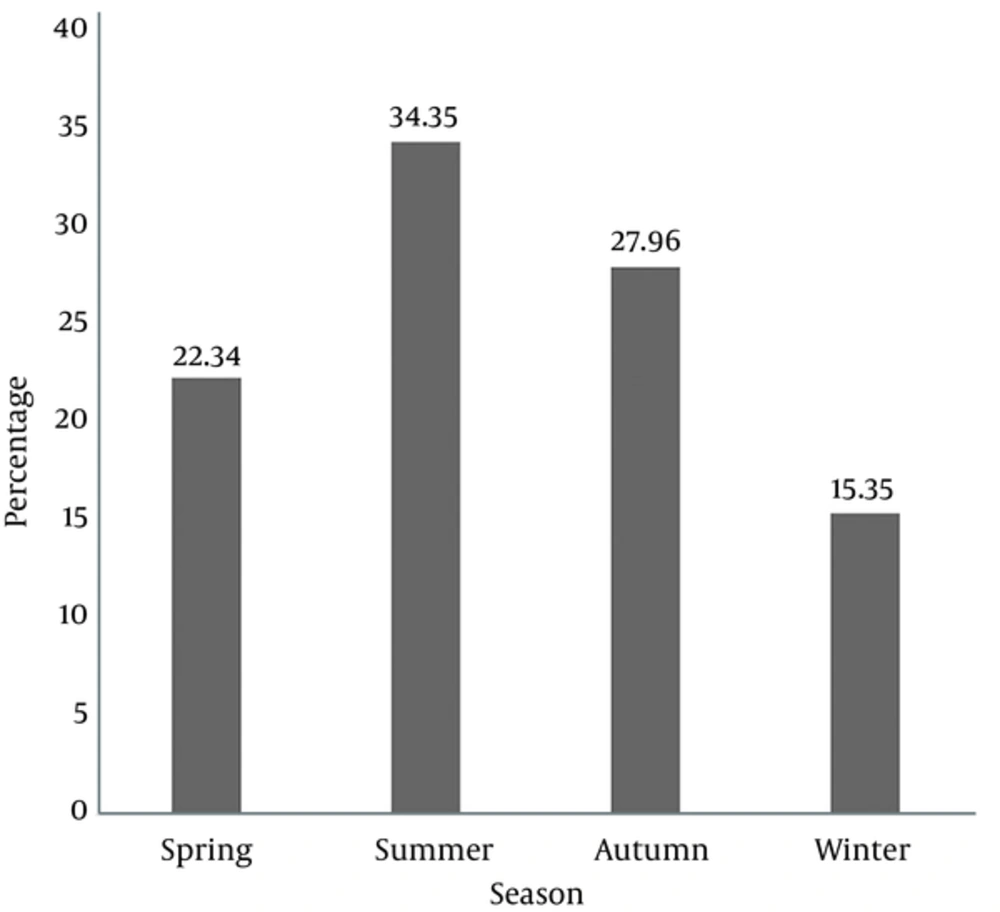
Out of 13698 stool specimens, 658 positive cases (424 male and 234 female) were diagnosed for IPIs and the overall prevalence was calculated 4.8% (Table 1). Between these number, 649 (4.73%) and 9 (0.07%) belonged to protozoan and helminth infections, respectively (Table 2). Among infected men and women significant differences were seen (Table 1). Our findings indicated a decreasing trend in rate of infection so that the prevalence from 6.42% in 2010 fell down to 3.83% in 2013 (Table 1). Also maximum infection was observed in summer season (34.35%) and autumn (27.96%) placed in second rank (Figure 2). The most common protozoa and worm belonged to G. lamblia (3.16%) and H. nana (0.04%), respectively (Table 2). Prevalence of other parasites are summarized in Table 2. No positive cases with A. lumbricoides, hookworm, T. trichiura and Strongyloides stercoralis were reported.
| Year | Number of Referred, No. (%) | Positive Cases, No. (%) | Female, No. (%) | Male, No. (%) |
|---|---|---|---|---|
| 2010 | 4375 (31.94) | 281 (6.42) | 101 (36) | 180 (64) |
| 2011 | 3373 (24.63) | 136 (4.03) | 51 (37.5) | 85 (62.5) |
| 2012 | 2981 (21.76) | 127 (4.26) | 50 (39.4) | 77 (60.6) |
| 2013 | 2969 (21.67) | 114 (3.83) | 32 (28) | 82 (72) |
| Total, No. (%) | 13698 (100) | 658 (4.8) | 234 (35.5) | 424 (64.5) |
| Parasite Species | Frequency, No. | Percentage, % |
|---|---|---|
| No. of people examined (N = 13698) | ||
| E. histolytica/dispar | 96 | 0.7 |
| E. coli | 77 | 0.56 |
| E. hartmanni | 29 | 0.21 |
| G. lamblia | 433 | 3.16 |
| B. hominis | 14 | 0.1 |
| H. nana | 6 | 0.04 |
| E. vermicularis | 1 | 0.007 |
| Taenia spp. | 2 | 0.014 |
| Total | 658 | 4.8 |
5. Discussion
Globally helminth and protozoan parasites are one of the most serious public health concerns with a widely distribution pattern in many countries and territories particularly in tropical and subtropical developing countries and seen mainly in children (1, 7, 9, 19-26). Prevalence of intestinal parasitic diseases in each society considered as an indices of health condition of region. Some personal (immunity condition, nutrition status, hygiene, literacy, cultural habits, and etc.) and environmental factors like climate, geographical position, poverty and socioeconomic status, poor sanitary conditions, and high density of population may contribute to IPIs prevalence (1). In recent years numerous investigations have been done throughout the country of Iran and all of them demonstrated a dramatical slump in the frequency of IPIs, particularly in helminthic infections (13, 27, 28) in comparison with past decades (29). This sharp decrease may be due to improving the sanitation status, hygienic level, and knowledge of majority of people.
Based on our findings, a continual decline was seen in the rate of infection. The overall prevalence of IPIs was 4.8% (Table 1), which is consistent with studies such as Nasiri et al. (27) in the city of Karaj (4.7%), and, Sadeghi and Borji (28) in Qazvin city (5.8%), while higher prevalence of IPIs was reported from the Mazandaran province (9.1%) (30), Isfahan city (10.42%) (31) as well as Hamadan city (35.1%) (12). At Sayyari et al., in the study in the general population of Islamic Republic of Iran, which was done during 1999 - 2000, IPIs infection were reported 19.3% and G. lamblia with 10.9% placed at first rank that is consistent with our study. Furthermore, proportion of other parasites were as follows: E. histolytica 1%, A. lumbricoides 1.5%, E. vermicularis 0.5%, Taenia saginata 0.2%, Trichostrongylus colubriformis 0.2%, T. trichiura 0.1%, Ancylostoma duodenale 0.1% and, others 5.1% (9).
Current findings showed that the rate of infection caused by protozoa is dramatically higher than helminthic cases (4.73% and 0.07%, respectively) (Table 2). One reason for this fact is that protozoa could transmit easier than larvae and ova of helminths. From protozoan, G. lamblia was diagnosed as the most frequent parasite with 3.16%, which is similar to studies such as Yemen (17.7%) (10), Karaj city (3.8%) (27), Kashan city (2.7%) (18), and Ghaemshahr town (32), while in some researches E. coli (12, 28), E. histolytica/dispar (33) or B. hominis (11, 31) were most common. Giardia is found in food, soil, and any surface that was contaminated with infected feces (2). Additionally, polluted water supplies could be a potential factor for amebiasis and giardiasis. Many intestinal parasite outbreaks, due to contamination of municipal water resources, have been reported during the past decades (34). Based on a systematic review and meta-analysis study done by Karambaigi et al., in Iran during 1988 - 2009, from 234570 individuals who were examined, the prevalence of E. histolytica/dispar was reported as 1.3% (2.5% and 0.8% in rural and urban regions, respectively) (35). In the present survey, only 96 (0.7%) E. histolytica/dispar cases were detected, which is lower than the average prevalence of Karambaigi study.
In our study, among helminthic infections, H. nana with 0.04% was the most common detected worm that is in agreement with Akhlaghi et al. (11) in Tehran city (0.2%), Hooshyar et al. (18) in Kashan city (0.02%), and Sedeghi and Borji (28) in Qazvin city (0.1%), while in the Shobha et al. study in India, A. lumbricoides (2.04%) was reported as a major infection (36). Previous conducted studies in the province of Khuzestan have demonstrated the potential presence of intestinal parasites in food handlers, soils, water resources, and vegetables that indicated the establishment and persistence of IPIs in all parts of the region (2, 3, 13, 37-39). In a 10-year retrospective study, performed by Saki et al., in the province of Khuzestan, among food handlers, 62007 stools were examined and 7.78% of total population were identified positive for pathogenic IPIs. Frequency of G. lamblia, H. nana, E. histolytica/dispar and, A. lumbricoides was 4.52%, 1.29%, 1.39%, and 0.57%, respectively (37).
In the present study, the prevalence of IPIs in males with 64.5% was significantly higher than females. This issue could be explained by the number of study population and cultural habit such as working women in agricultural farms. Overall, the differences between our results and other studies may be attributed to the sample size, type of sampling, methodology, cultural habits of the region, occupations, geographical location, sanitary status, and many other factors.
5.1. Conclusion
According to the current paper, the trend of IPIs in samples that be received to the central health laboratory of Haftkel county was decreased and the prevalence from 6.42% in 2010 dropped to 3.83% in 2013. Health education and improving facilities environmental, especially in rural and semi-urban areas can be helpful. Along with those epidemiological studies done for screening, determining the severity of infection and early treatment of patients in order to adopting prevention program is necessary. Furthermore it is highly recommended to choose a specific staining including Trichrome for better discrimination of amoeba in the future study.