1. Background
The COVID-19 pandemic, caused by the novel SARS-CoV-2 virus first detected in Wuhan, China (December 2019), has precipitated unprecedented global morbidity and mortality (1). Iran faced early and sustained transmission, with significant clinical and societal repercussions (2). While COVID-19 predominantly manifests as a respiratory illness, its systemic effects — spanning renal, cardiovascular, gastrointestinal, and neurological systems — underscore its pathophysiological complexity (3). Clinical presentations range from asymptomatic infection to critical respiratory failure, often progressing dynamically after the first week. Common symptoms include fever (72% - 90%), cough (64% - 82%), fatigue (11% - 70%), and dyspnea (31%), with less frequent reports of sputum production (28%), headache (8%), hemoptysis (5%), and diarrhea (3%). Fever patterns remain inconsistently characterized, frequently presenting as prolonged or intermittent (4).
Radiological evolution in COVID-19 parallels clinical progression. Early-stage imaging may appear normal, but characteristic computed tomography (CT) findings — such as ground-glass opacities (GGO), crazy-paving patterns, consolidation, traction bronchiectasis, and subpleural bands — emerge with advancing disease (5, 6). These features correlate strongly with pulmonary severity and clinical outcomes, offering critical prognostic insights.
Vaccination has demonstrably attenuated COVID-19 severity, reducing hospitalization rates and mitigating pulmonary complications (7, 8). Laitin et al. (8) found that vaccinated patients had significantly lower rates of severe pulmonary involvement compared to unvaccinated patients. Vaccinated individuals also had shorter hospital stays. Additionally, chronic pulmonary diseases and stroke were less prevalent among vaccinated patients, highlighting the protective effect of vaccination. Therefore, COVID-19 vaccination significantly reduces the severity of the disease, particularly in preventing severe pulmonary involvement, which is a major determinant of patient outcomes. However, the emergence of variants (alpha, beta, gamma, delta, omicron) challenges vaccine efficacy, necessitating ongoing evaluation of their impact on disease modulation (9). Age and comorbidities remain key determinants of adverse outcomes, amplifying the imperative for vaccination in high-risk populations (7).
2. Objectives
This study aimed to investigate CT imaging disparities between vaccinated and unvaccinated COVID-19 patients aged 20 - 50 years.
3. Methods
3.1. Study Design and Population
This retrospective analytical study included 189 COVID-19 patients aged 20 - 50 years, divided equally into three groups based on their vaccination status: Fully vaccinated (n = 63), partially vaccinated (n = 63), and unvaccinated (n = 63). Participants were selected through consecutive sampling from medical records at Ali Ebn Abitalib Hospital, affiliated with Zahedan University of Medical Sciences in Zahedan, Iran, in 2023.
To be included in the study, participants were required to have a polymerase chain reaction (PCR)-confirmed SARS-CoV-2 infection, available chest CT scans showing documented pulmonary involvement, and no history of comorbidities such as diabetes, hypertension, immune disorders, hyperlipidemia, or vasculitis, as these conditions could affect radiological findings.
Exclusion criteria included incomplete medical records, missing CT imaging, a history of the aforementioned comorbidities, or prior COVID-19 infection, in order to minimize the influence of natural immunity.
3.2. Diagnostic Testing
To ensure an accurate diagnosis, both nasal and pharyngeal sampling techniques were systematically employed. Nasal swabs served as the primary method for specimen collection. If the nasal sample yielded inconclusive or unreliable results, a follow-up pharyngeal sample was obtained. This stepwise approach was designed to enhance diagnostic reliability while prioritizing patient comfort.
3.3. Data Collection
Demographic data, vaccination status, and CT findings were extracted using a structured, researcher-developed checklist. Data were collected from medical records and, when necessary, through direct patient contact or telephone calls.
3.4. Vaccination Status Definitions
Vaccination status was classified based on the 2023 WHO and national health guidelines.
3.4.1. Fully Vaccinated
Completion of the primary vaccine series (typically 2 or 3 doses, depending on the vaccine type and eligibility for boosters) at least 14 days prior to symptom onset. If a booster was considered part of the primary series in 2023, three doses were required for full vaccination.
3.4.2. Partially Vaccinated
Individuals who started but did not complete the primary series, or those who completed it but did not receive a booster (if one was deemed necessary).
3.4.3. Non-vaccinated
Individuals who had not received any COVID-19 vaccine doses before symptom onset.
3.5. Computed Tomography Imaging and Analysis
Chest CT scans were performed using a 128-slice Siemens SOMATOM Definition AS scanner with standardized protocols. Radiologists, who were blinded to the patients’ vaccination status, analyzed the scans to minimize bias. The following CT findings were recorded: Consolidation, bronchial wall thickening, GGO, nodules, halo sign, reverse halo sign, pleural effusion, pericardial effusion, subpleural bands, and lung involvement.
To quantify pulmonary involvement, the total lung volume and the volume of affected areas were measured using the picture archiving and communication system (PACS). The ratio of involved lung volume to total lung volume was calculated to determine the percentage of lung involvement.
3.6. Statistical Analysis
Data were analyzed using SPSS version 22 (IBM Corp.). Categorical variables were summarized as frequencies (%) and compared using chi-square or Fisher’s exact tests. Continuous variables were expressed as mean ± SD and analyzed using independent t-tests for normally distributed data or Mann-Whitney U tests for non-normally distributed data. Intergroup comparisons across the three cohorts were conducted using ANOVA or Kruskal-Wallis tests, as appropriate. Normality was assessed using the Shapiro-Wilk test. A two-tailed P-value < 0.05 was considered statistically significant.
3.7. Ethical Considerations
The study protocol was approved by the Institutional Review Board of the university (IR.ZAUMS.REC.1402.089). Informed consent was waived due to the retrospective nature of the study and the use of anonymized data.
4. Results
The study cohort comprised 189 participants (mean age 35.71 ± 6.56 years; range 20 - 50), with a female predominance [109 (57.7%)] and 80 male participants (42.3%). Vaccine distribution analysis revealed Sinopharm as the most frequently administered vaccine (n = 85, 67.5%), followed by AstraZeneca (n = 35, 27.8%), while Barakat demonstrated the lowest utilization (n = 6, 3.2%). Among the 189 patients, 96 (50.8%) exhibited diffuse pathological changes affecting all lung lobes, while 36 (19.0%) demonstrated no radiologically detectable abnormalities. The GGO emerged as the predominant radiological feature, observed in 146 cases (77.2%).
Table 1 demonstrates significant disparities in pulmonary CT manifestations stratified by vaccination status. A striking disparity emerged in consolidation prevalence, observed in 60.3% of unvaccinated patients, 27% of partially vaccinated individuals, and 7.9% of fully vaccinated subjects (χ2 = 40.887, P < 0.001). Bronchial wall thickening showed similar trends, affecting 54% of unvaccinated, 27% of partially vaccinated, and 4.8% of fully vaccinated individuals, with statistically robust intergroup differences (P < 0.001). The GGO, though prevalent across all groups, revealed a dose-dependent attenuation: 96.8% (unvaccinated), 90.5% (partially vaccinated), and 44.4% (fully vaccinated) (χ2 = 58.585, P < 0.001). Conversely, nodular lesions and pleural effusion exhibited no statistically significant association with vaccination status (P > 0.05).
| Finding | Unvaccinated (n = 63) | Partially Vaccinated (n = 63) | Fully Vaccinated (n = 63) | P-Value | χ2 |
|---|---|---|---|---|---|
| Consolidation | 38 (60.3) | 17 (27) | 5 (7.9) | < 0.001 | 40.887 |
| Bronchial wall thickening | 34 (54) | 17 (27) | 3 (4.8) | < 0.001 | 37.489 |
| GGO | 61 (96.8) | 57 (90.5) | 28 (44.4) | < 0.001 | 58.585 |
| Nodules | 6 (9.5) | 9 (14.3) | 8 (12.7) | 0.707 | 0.693 |
| Halo sign | 26 (41.3) | 1 (1.6) | 0 (0) | < 0.001 | 56.259 |
| Reverse halo sign | 28 (44.4) | 5 (7.9) | 1 (1.6) | < 0.001 | 45.69 |
| Pleural effusion | 8 (12.7) | 3 (4.8) | 8 (12.7) | 0.232 | 2.926 |
| Pericardial effusion | 5 (7.9) | 2 (3.2) | 4 (6.3) | 0.509 | 1.351 |
| Subpleural band | 1 (1.6) | 4 (6.3) | 0 (0) | 0.069 | 5.341 |
Abbreviation: GGO, ground-glass opacity.
a Values are expressed as No. (%).
Quantitative analysis of pulmonary involvement (Table 2) demonstrated pronounced stratification by vaccination status. Unvaccinated patients exhibited heterogeneous disease severity, with lung involvement ranging from 12% to 87%. Partially vaccinated individuals showed moderate attenuation of pathology, with involvement confined to 37 - 50%. Fully vaccinated patients displayed the most striking reduction, with lung involvement limited to a narrow range around 12%, underscoring a statistically significant protective association (P < 0.001).
| Characteristic | Unvaccinated (n = 63); (%) | Partially Vaccinated (n = 63); (%) | Fully Vaccinated (n = 63); (%) | P-Value |
|---|---|---|---|---|
| Lung involvement | 62 (12 - 87) | 43 (37 - 50) | 12 (11 - 14) | < 0.001 |
Table 3 shows the gender-specific disparities in CT manifestations. Significant sex-based differences emerged across multiple radiological features. Consolidation prevalence was two-fold higher in males (44.3%) compared to females (22.9%) (χ2 = 9.625, P = 0.002). Similarly, bronchial wall thickening showed a marked disparity, affecting 44.3% of males compared to 17.4% of females (χ2 = 16.156, P < 0.001). The GGO, though prevalent in both sexes, was 13.2% more frequent in males (84.8% vs. 71.6%) (χ2 = 4.559, P = 0.033). Nodules and reverse halo sign exhibited similar trends: Nodules in 19% of males vs. 7.3% of females (χ2 = 5.788, P = 0.016) and reverse halo sign in 29.1% of males vs. 10.1% of females (χ2 = 11.187, P = 0.001).
Notably, subpleural bands were exclusively observed in females (Fisher’s exact test, P = 0.075), suggesting a marginal association. No significant sex-linked differences were identified for halo sign, pericardial effusion, or subpleural bands (P > 0.05).
| Finding | Female (n = 109) | Male (n = 80) | P-Value | χ2 |
|---|---|---|---|---|
| Consolidation | 25 (22.9) | 35 (44.3) | 0.002 | 9.625 |
| Bronchial wall thickening | 19 (17.4) | 35 (44.3) | 0.001 | 16.156 |
| GGO | 78 (71.6) | 67 (84.8) | 0.033 | 4.559 |
| Nodules | 8 (7.3) | 15 (19) | 0.016 | 5.788 |
| Halo sign | 12 (11) | 15 (19) | 0.124 | 2.37 |
| Reverse halo sign | 11 (10.1) | 23 (29.1) | 0.001 | 11.187 |
| Pleural effusion | 15 (13.8) | 4 (5.1) | 0.051 | 3.814 |
| Pericardial effusion | 9 (8.3) | 2 (2.5) | 0.099 | 2.725 |
| Subpleural band | 5 (4.6) | 0 (0) | 0.075 | Fisher’s exact test |
Abbreviation: GGO, ground-glass opacity.
a Values are expressed as No. (%).
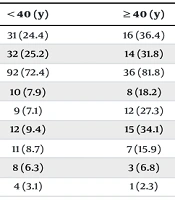
Table 4 presents the age-stratified radiological patterns. Age-related divergences were prominent in specific CT features. While consolidation prevalence did not differ significantly between age groups (24.4% in those < 40 years vs. 36.4% in those ≥ 40 years; χ2 = 2.343, P = 0.126), halo sign and reverse halo sign demonstrated robust age dependency: Halo sign in 27.3% of patients aged ≥ 40 years vs. 7.1% of those < 40 years (χ2 = 12.361, P = 0.001) and reverse halo sign in 34.1% of patients aged ≥ 40 years vs. 9.4% of those < 40 years (χ2 = 14.924, P = 0.001). Pericardial effusion showed comparable frequencies across age strata (P = 0.904).
| Characteristic | < 40 (y) | ≥ 40 (y) | P-Value | χ2 |
|---|---|---|---|---|
| Consolidation | 31 (24.4) | 16 (36.4) | 0.126 | 2.343 |
| Bronchial wall thickening | 32 (25.2) | 14 (31.8) | 0.393 | 0.729 |
| GGO | 92 (72.4) | 36 (81.8) | 0.217 | 1.527 |
| Nodule | 10 (7.9) | 8 (18.2) | 0.055 | 3.687 |
| Halo sign | 9 (7.1) | 12 (27.3) | < 0.001 | 12.361 |
| Reverse halo sign | 12 (9.4) | 15 (34.1) | < 0.001 | 14.924 |
| Pleural effusion | 11 (8.7) | 7 (15.9) | 0.177 | 1.823 |
| Pericardial effusion | 8 (6.3) | 3 (6.8) | 0.904 | 0.015 |
| Subpleural band | 4 (3.1) | 1 (2.3) | 0.999 | Fisher’s exact test |
Abbreviation: GGO, ground-glass opacity.
a Values are expressed as No. (%).
5. Discussion
The findings of this study, corroborated by emerging global evidence, underscore the profound impact of COVID-19 vaccination on attenuating pulmonary pathology, as reflected in CT imaging. Our cohort of 189 patients demonstrated that fully vaccinated individuals exhibited significantly fewer severe radiological manifestations, such as consolidation (7.9% vs. 60.3% in unvaccinated) and bronchial wall thickening (4.8% vs. 54%), aligning with prior reports of vaccine-mediated mitigation of lung injury (9-13).
Ground-glass opacity, though prevalent across all groups, showed a dose-dependent reduction in fully vaccinated patients (44.4% vs. 96.8% in unvaccinated), consistent with Lee et al. (13), who observed normal CT scans in 59% of vaccinated individuals compared to 22% in unvaccinated cohorts. These findings reinforce the protective role of vaccination in limiting alveolar inflammation and interstitial edema, likely through reduced viral replication and systemic immune dysregulation (11, 14).
Notably, our study revealed striking gender-based differences in CT manifestations, with males exhibiting higher rates of consolidation (44.3% vs. 22.9%; P = 0.002), bronchial wall thickening (44.3% vs. 17.4%; P < 0.001), and GGO (84.8% vs. 71.6%; P = 0.033). This disparity may reflect biological factors, including androgen-driven ACE2 receptor expression or sex-specific immune responses, though behavioral confounders (e.g., smoking, occupational exposures) warrant further investigation.
The male predominance of nodules (19% vs. 7.3%) and reverse halo signs (29.1% vs. 10.1%; P = 0.001) further suggests heightened inflammatory or fibrotic responses in males, a finding echoed in Zarifian et al.’s meta-analysis (15), which linked male sex to bilateral lung involvement. Age emerged as a critical determinant of specific CT patterns, with halo and reverse halo signs disproportionately affecting patients ≥ 40 years (27.3% and 34.1% vs. 7.1% and 9.4% in younger cohorts).
These findings are consistent with the observations reported by Shi et al. (16), who documented a progression to consolidation and mixed patterns in the later stages of COVID-19, particularly among older adults. The higher prevalence of these signs in older patients may reflect factors such as age-related immune decline (immune senescence), microvascular dysfunction, or fibrosis driven by underlying health conditions (14, 16).
Interestingly, the absence of age-related differences in consolidation or pleural effusion highlights the complex nature of pulmonary injury. This suggests that factors such as vaccination status and baseline health may play a more significant role than chronological age in determining outcomes (7, 14).
Although breakthrough infections were observed in vaccinated individuals, these cases were notably less severe, as reflected by reduced CT severity scores (13) and fewer ICU admissions (13, 14). Bergwerk et al. (12) similarly reported that 94% of vaccinated individuals with breakthrough infections experienced mild or asymptomatic illness, accompanied by lower viral loads. This aligns with our observation of limited lung involvement in fully vaccinated patients (12%) compared to unvaccinated patients (87%), with a statistically significant difference (P < 0.001).
However, Brosh-Nissimov et al. (14) cautioned that immunocompromised and comorbid populations remain at increased risk, reporting a 22% mortality rate among fully vaccinated hospitalized patients. This underscores the importance of tailored booster strategies to protect vulnerable groups (17).
The broader evidence, including insights from Jung (17), emphasizes vaccination as a cornerstone of pandemic control. Our findings further support the protective role of vaccines in reducing severe radiological manifestations, consistent with the conclusions of Lee et al. (13) and Antonelli et al. (11), even in the context of emerging variants.
Nonetheless, certain limitations should be acknowledged. The single-center design, retrospective data collection, and predominant use of the Sinopharm vaccine (67.5% of cases) may restrict the generalizability of our results. Future studies should incorporate multivariate analyses to account for comorbidities, vaccine types, and variant-specific responses. Additionally, longitudinal imaging would provide valuable insights into the long-term pulmonary consequences of COVID-19.
5.1. Study Limitations
The relatively small cohort and equal subgroup stratification may limit the statistical power to detect subtler associations, particularly for less common CT findings and gender- or age-stratified analyses. Larger, multicenter cohorts are needed to validate these trends.
5.2. Conclusions
In conclusion, this study elucidates the triad of vaccination status, gender, and age as pivotal factors shaping the radiological footprint of COVID-19. Full vaccination significantly attenuates severe CT manifestations, while male gender and advanced age independently correlate with heightened pulmonary pathology. These insights advocate for the prioritized vaccination of high-risk demographics, sustained genomic surveillance for emerging variants, and the implementation of sex- and age-tailored clinical management protocols to optimize outcomes in the pandemic’s evolving landscape.