1. Background
An estimated 15 million infants, that is, more than 1 in 10 infants, are born prematurely every year (1). In a study in 2015 in Iran, the overall prevalence of preterm birth was estimated at 9.2% based on the results of 14 studies (2). These infants usually spend the first week of their life in the neonatal intensive care unit. As part of diagnostic and therapeutic care, they are subject to 10-16 painful procedures (3, 4). Almost 80% of these infants do not receive any treatment for pain relief (5). Repeated exposure to pain during critical developmental phases of the central nervous system leads to temporary and permanent changes in brain structure and function, pain perception and processing, impaired endocrine and nervous system development, which in turn leads to changes in pain threshold, in responses to stress, cognitive changes, behavioral disorders and long-term disability in future (6, 7). Efficient pain management is a patient’s right and a priority in care (8). The first step in efficient pain management is a proper assessment. Pain assessment is known as the fifth vital sign that should be included in routine clinical practices (9, 10). According to international association for the study of pain (IASP), pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage (11). Since experience of pain is subjective, the expression of pain is a valuable measure for its assessment, which is not applicable in infants as they are not able to express their pain verbally (5).
Accurate assessment of pain is necessary for pain control (12) with a proper and reliable tool. More than 30 tools have been designed for assessing infants’ pain with a unique capability to determine pain scores during the painful procedures (13). They are divided into two types of uni-dimensional and multidimensional tools. The former measures only one aspect of pain that is the infants’ behavioral responses, and the latter assesses behavioral and physiological responses simultaneously in combination with other contextual factors (14).
Since pain is a complex and multidimensional phenomenon, a tool capable of assessing multidimensional tools are more desirable and better to assess pain in infants (15).
Premature Infant Pain Profile (PIPP) is a valid and reliable multidimensional tool for measuring pain in infants, developed by Stevens and colleagues in 1996 (16).
PIPP consists of 7 indicators being able to assess behavioral, physiological and contextual symptoms of acute pain in preterm and term infants. Three indicators are related to behavioral changes (facial changes), two indicators related to physiological changes (heart rate and oxygen saturation percentage) and two indicators related to contextual factors (gestational age and behavioral state). It has scores of 0 - 21 where 0 - 6 indicate no pain, 7 - 12 indicate moderate pain, and 12 - 21 indicate severe pain. The tool was revised and its scoring method was modified in 2014 as premature infant pain profile-revised (PIPP-R), in that the gestational age and behavioral state indicators are scored after the behavioral and physiological response to pain assessment (17).
The use of a validated tool for assessing pain in infants is the first step for proper diagnosis treatment of pain (13). Validation of the tool reduces errors in proper assessment and diagnosis of pain in clinical practices (18). The quality of pain assessment depends on the type of pain assessment tool and patient’s specific condition. Since the infants are not able to express their pain, its diagnosis is based on the judgment of caregivers. One of the most important problems in this field is the difference in pain assessment by different people leading to inappropriate control of pain in prematures and ill infants (19). Therefore, it is necessary to separately validate pain assessment tools for each community before use in clinical practice. Translation and validation of tools are essential to ensure consistency between the original version and the translated version and to maintain the psychometric properties of the tool. The process of translation and validation of the tools in other languages save time and money. In addition, the translation and validation of the tools have made the researchers aware of the results of the research carried out in different countries, and thus they will be able to compare and share the results of their research (20).
The use of non-validated tools may lead to inappropriate pain assessment in premature infants and is a serious threat to their evolving nervous system (21). Nurses as supporters of premature infants who spend a lot of time with them, are responsible for protecting the rights of infants with regard to effective control of pain (7). Hence, it is essential that nurses use a valid tool with high applicability to assess pain in infants in clinical practice in order to ensure proper pain assessment and management (21). The existence of a valid pain assessment tool in NICU will increase the accuracy of nurses in assessing pain in premature infants in routine care, also it will enhance nursing ethical decision making in pain management in this vulnerable population who cannot properly express their pain (22).
PIPP was used for clinical research in Iran (23, 24), but a literature review in Medline and Google Scholar revealed the revised PIPP has not been used or validated in Iran.
Because PIPP-R is one of the most reliable tools for assessing pain in infants, the present study aimed to determine the construct validity and reliability of this tool in preterm and term infants hospitalized in neonatal intensive care units.
2. Methods
This is a methodological study for validating PIPP-R in the neonatal intensive care units of Buali Hospital and Imam Khomeini hospital affiliated with Mazandaran University of Medical Sciences in Sari, northern Iran. It was carried out from September 2015 to May 2015. “Premature Infant Pain Profile-revised” was translated and revised in 3 steps.
Step 1: translation of the PIPP-R. After receiving permissions from Dr. Stevens, the tool designer, PIPP-R was translated into Persian based on the World health organization quality of life (HOQOL) suggestions (25) by a neonatologist and a general practitioner who were fluent in Persian and English. Then forward-translated version was back-translated into English by two professional translators, fluent in English, who were not familiar with the English version of tool prior to translation in order to ensure the accuracy. Finally, by comparing the two English texts (the original text and the one translated from Persian), necessary modifications were applied by the researcher and a pain specialist and the final Persian version of the PIPP-R was prepared and sent to the tool designer to receive his comments and ensure the correctness of the translation. The designer confirmed the translation by email.
Step 2: Determining the construct validity: The easiest way to determine the construct validity of a tool is using it in two different situations or groups (26). Therefore, in this phase of the research, the construct validity of the PIPP-R was determined through discriminant validity and in form of two separate quasi-experimental sub-studies on infants admitted to the neonatal intensive care units of Bu’ali Sina and Imam Khomeini hospitals in Sari. A total of 145 infants hospitalized in neonatal intensive care units with 26 to 39 weeks gestational age were included, of whom 100 were preterm and 45 term infants. The infants were classified into four groups in terms of gestational age according to the PIPP-R: The first group consisted of infants with of less than 28 weeks, the second group 28 - 32 weeks, 32 - 36 weeks and the fourth group 37 - 39 weeks of gestational age.
Samples were selected by purposive sampling based on the inclusion criteria: infants’ being younger than 30 days old at the time of data collection, no neurological disorders and anomalies, administration of no analgesic and sedative drugs 12 hours before the intervention, and having a stable physiological status according to judgment of a neonatologist. The exclusion criteria were infants being under mechanical ventilation and Nasal Continuous Positive Airway Pressure (NCPAP).
The sample size in each group, considering the type I error of 1% and power of 95%, was calculated at least 43 subjects. The analysis of variance was used to determine the sample size because there were several groups.
2.1. Definition of Pain Event
The infants eligible for the study were examined in terms of pain in three phases (basic, during the painful and non-painful procedures):
The basic phase definition: The infant was quiet without any interference or diagnostic and therapeutic intervention.
The painful phase definition: The painful procedure was a heel prick carried out by a nurse.
The non-painful phase definition: Changing diapers was the non-painful procedure performed by a nurse.
2.2. Data Collection
2.2.1. The First Sub-Study
In the sub-study pain score was compared in 4 different groups according to gestational age. Studies have shown that behavioral and physiological changes when exposed to pain are different in lower gestational age infants compared to other infants (27, 28). Since the pain score is different in infants with different gestational ages, data analysis was performed in the first step with the aim to determine pain score comparisons in infants with different gestational ages during heel prick. Qualified infants were divided into four groups according to gestational age. The first group included infants with gestational age of less than 28 weeks, the second group of 28 - 31 weeks, the third group those of 32 - 36 weeks, and the fourth group of 37 - 39 weeks. At this phase, 100 preterm and 45 term infants were enrolled in the study.
The painful procedure was heel prick in all infants which was part of the diagnosis and treatment process performed to measure blood sugar as directed by a neonatologist. A glucometer (BIONIME) was used to determine the infant’s blood sugar. A similar needle, G21 (NRK, Nik Rahnama Co.), was used for taking blood samples from the heel of all infants.
All blood samples were taken by a BSc nurse with 10 years of experience in the neonatal intensive care unit, at infant’s bed in the neonatal intensive care unit. The samples were collected while the infants were lying on their back. There were no manipulations 30 minutes before blood sampling. The infant’s heel was sanitized with alcohol cotton and a lancet inserted in the side of the foot. The blood samples were then taken to measure blood sugar. There were no manipulations 30 minutes after heel prick even rubbing the site.
2.2.2. The Second Sub-Study
In the second sub-study pain scores after a painful and a non-painful procedure were compared in the premature infants. This quasi-experimental sub-study was conducted on 100 premature infants admitted to the neonatal intensive care unit to determine and compare the pain scores of premature infants during a painful and a non-painful procedure.
At this phase, heel prick was the painful procedure and changing diapers was the non-painful procedure (17, 29). The data used in this section were those on 100 premature infants in the previous study under the heel prick procedure.
In the study, changing diapers was performed 1.5 hours after the painful procedure. The infants did not have any manipulation during this time. Changing diapers was done by the same nurse and at the infant’s bed.
The cardiorespiratory monitor ABADIS 707 was used to record physiological parameters. All infants were under a monitor that recorded their heart rate and oxygen saturation before undergoing painful and non-painful procedures.
A high-quality video camera (Canon SX 720) was used to record infants’ responses to the pain caused by heel prick, and to determine physiological changes and facial changes due to changing diapers. All infants were filmed 30 seconds before the painful and non-painful procedures, during the procedures and up to 30 seconds after the procedures. The camera was placed so, that the physiological facial changes of the infant could be completely recorded during painful and non-painful procedures. The filming was in a way that only the infant’s face was visible and thus the viewer could not identify whether it is of the painful group or the non-painful group. It was only distinguishable by the codes given by the researcher.
Recorded videos were observed and interpreted by the researcher and a pain specialist familiar with the scoring tool. The scores were determined based on the final Persian version of the PIPP-R.
Step 3: Reliability: The reliability of the PIPP-R was assessed in premature infants hospitalized in the neonatal intensive care units. The pain score was calculated by two nurses competent in the use of the tool, independently and simultaneously in 10 infants, at the basic phase and during the heel prick. Inter-rater reliability was determined by ICC. The internal consistency of the tool was determined by Cronbach’s alpha in 145 infants during a painful procedure based on 6 PIPP indicators including behavior state, facial expression, and physiological criteria.
2.3. Data Analysis
The present study used SPSS software version 21 for data analysis. Descriptive statistics such as mean, standard deviation, frequency, and percentage were used for demographic variables. Independent t-test and Pearson’s correlation coefficient were used to determine the relationship between demographic variables and pain scores among the four groups. In the descriptive statistics, the paired t-test was used to determine the pain score differences in the two separate procedures among the groups. The one-way ANOVA was used to compare pain scores among groups. Inter-rater reliability was determined by ICC. The internal consistency of the tool was determined by Cronbach’s alpha. The significance level was assumed P<0.05.
2.4. Ethical Considerations
The study was approved by the ethics committee of School of Nursing and Midwifery Shahid Beheshti University with a SBMU2.REC.1394.110 ethics code. Informed consent for filming was obtained in writing from the parents of infants. Written consent for conducting the study was obtained from the head of the study hospitals as well as the heads of the neonatal intensive care units. All obtained information and videos were used only for research purposes.
3. Results
The present study examined 145 preterm and term infants whose demographic characteristics are presented in Table 1.
| Variable | < 28 Weeks (n = 10) | 28 - 31 Weeks (n = 31) | 32 - 36 Weeks (n = 59) | ≥ 37 Weeks (n = 45) |
|---|---|---|---|---|
| Birthweight, g | 977 ± 32.6 | 1290 ± 46.4 | 2255 ± 71.45 | 3168 ± 58.9 |
| Postnatal age, d | 7.80 ± 6.46 | 1.68 ± 9.64 | 4.88 ± 3.29 | 4.67 ± 2.18 |
| Gender | ||||
| Girl | 7 (70) | 18 (58.1) | 24 (40.7) | 18 (40) |
| Boy | 3 (30) | 13 (41.9) | 35 (59.3) | 27 (60) |
| Type of delivery | ||||
| Cesarean delivery | 8 (80) | 28 (90.3) | 52 (88.1) | 39 (86.7) |
| Normal delivery | 2 (20) | 3 (9.7) | 7 (9.11) | 6 (13.3) |
Demographic Characteristics of Infants Hospitalized in Neonatal Intensive Care Units, According to Gestational Agea
3.1. Construct Validity
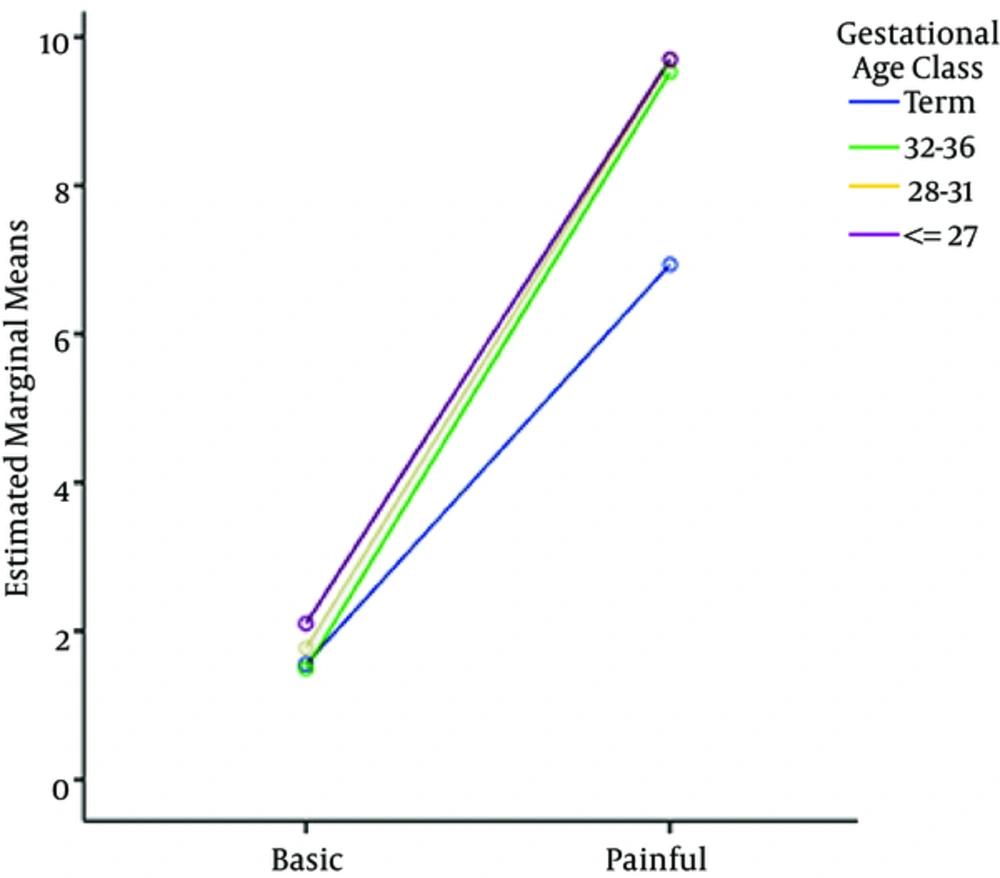
The first sub-study results, comparing the pain scores among four term and preterm groups of infants, showed a significant difference in heel prick scores among the groups (P < 0.001). It indicates that the highest pain score calculated by PIPP-R in heel prick was for neonates less than 28 weeks (9.40 ± 2.40) and the lowest score was for the term neonates (6.93 ± 3.12) (Table 2).
| Groups, w | Basic Phase | Heel Prick Phase | P Value |
|---|---|---|---|
| < 28 | 2.10 ± 0.87 | 9.70 ± 2.40 | < 0.001 |
| 28 - 31 | 1.77 ± 1.17 | 9.68 ± 2.76 | < 0.001 |
| 32 - 36 | 1.49 ± 1.19 | 9.53 ± 2.50 | < 0.001 |
| ≥ 37 | 1.56 ± 1.23 | 6.93 ± 3.12 | < 0.001 |
The Changes of Pain Scores Calculated by the PIPP-R Among the Four Gestational Age Groupsa
The greatest changes in the basic phase pertain to heel prick among the four groups of gestational age was in infants with gestational age of less than 28 weeks (Figure 1).
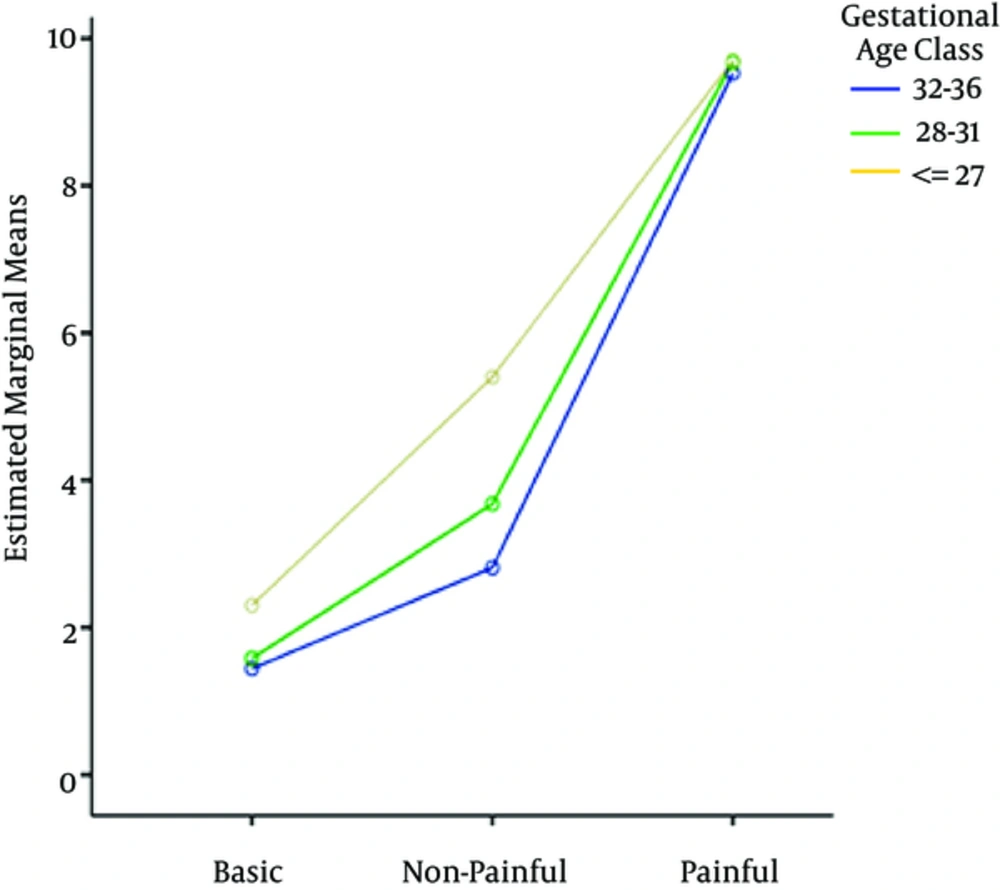
The second sub-study results, calculating the pain scores in three groups of preterm infants, showed that the mean and standard deviation of pain scores calculated by PIPP-R during diapers and heel prick were 3.34 ± 1.48 and 9.59 ± 2.55, respectively. It indicates that the scores calculated by the PIPP-R during changing diapers was less than that during the heel prick. This difference was statistically significant (P < 0.001). The results of the comparison of scores by paired t-test at the basic phase showed no significant differences in pain scores calculated by the PIPP-R in the procedures. The comparison between the scores of changing diapers and heel prick among the three groups showed that the highest score pertained to that of infants with gestational age of less than 28 weeks in both the painful and non-painful phases (Table 3). The biggest changes in the basic phase pertain to changing diapers and heel prick in infants with gestational age of less than 28 weeks (Figure 2).
| Gestationl Age | Basic Phase | Changing Diapers | Basic Phase | Heel Prick Phase | P Value |
|---|---|---|---|---|---|
| Group 1, < 28 w | 2.30 ± 0.82 | 5.40 ± 0.69 | 2.10 ± 0.87 | 9.70 ± 2.40 | < 0.001 |
| Group 2, 28 - 31 w | 1.58 ± 1.11 | 3.68 ± 1.19 | 1.77 ± 1.17 | 9.68 ± 2.76 | < 0.001 |
| Group 3, 32 - 36 w | 1.44 ± 1.20 | 2.81 ± 1.37 | 1.49 ± 1.19 | 9.53 ± 2.50 | < 0.001 |
| P Value | 0.2 | < 0.001 | 0.25 | < 0.001 | < 0.001 |
| 3.34 ± 1.48 | 9.59 ± 2.55 | < 0.001 | |||
Changes of Pain Scores Calculated by the PIPP-R Among the Three Gestational Age Groupsa
3.2. Reliability
Inter-rater reliability was determined by ICC. Its level in the basic phase and the painful phase was 0.98 and 0.99, respectively.
The internal consistency of the tool was determined by Cronbach’s alpha. Cronbach’s alpha was 0.71 for the 6 indicators of the tool. Small changes in alpha coefficients were observed when each indicator was excluded separately (Table 4). Cronbach’s alpha had a more significant decrease in 3 behavioral indicators compared to other indicators. The Cronbach’s alpha obtained for the three indicators of facial changes was 0.97. After excluding the amount of oxygen and behavioral states, Cronbach’s alpha was 0.77. Data showed that the four indicators of heart rate, brow bulge, eye squeeze, and nasolabial furrow were more sensitive in showing the infants’ responses to pain in preterm and term infants.
| Cronbach’s Alpha in Case of Excluding Each indicator | Tool’s Indicators |
|---|---|
| 0.48 | Brow bulge (frown) |
| 0.49 | Eye squeeze |
| 0.48 | Nasolabial furrow |
| 0.52 | Heart rate increase |
| 0.76 | Reduction in oxygen saturation |
| 0.57 | Behavioral states |
| Alpha for 6 indicators of the tool | 0.71 |
The Internal Consistency of PIPP-R by Cronbach’s Alpha
4. Discussion
The most important finding of our study is that the pain score both in response to the painful procedure (heel prick) and the non-painful procedure (changing diaper) was higher in infants with gestational age of less than 28 weeks. Our study also revealed that term infants had the lowest score in response to the painful procedure.
Although pain is a subjective phenomenon, it is hard to determine its intensity and quality, especially in premature infants whose responses to pain are different due to their less developed central nervous system (18, 19). Gestational age is an important factor in response to pain (30).
A study by Gibbins et al (2008) showed a significant difference in pain score after heel prick between preterm and term groups such that the highest score belonged to infants with gestational age of less than 28 weeks and the lowest score belonged to term infants at this stage (27).
The findings of two studies showed that the response to pain in infants with a gestational age of less than 30 weeks is much higher than that of infants with gestational age of more than 30 weeks, because the self-regulating mechanism used to adapt to the environment in the latter is far more developed (31, 32).
Badr et al (2010) concluded that the pain score in infants varies according to gestational age such that the mean score of pain calculated by PIPP in infants with gestational age of 27 to 32 weeks was much higher than that in infants with gestational age of 36 to 40 weeks (33).
Infants are able to fully understand and respond to pain after week 24 of pregnancy due to development of cerebral cortex (30, 34). In preterm infants, the recipient area of painful stimuli is wider, descending mechanisms develop later than ascending mechanisms at birth, and neurons in the spinal cord are more irritable and more sensitive to local damage (35). The highest pain score was reported in extremely preterm infants with gestational age less than 28 weeks (29, 33, 36).
Jonsdottir et al also showed that infants with gestational age less than 28 weeks had higher pain scores than other groups during heel prick and changing diapers (19). A study on 50 infants less than 28 weeks by Gibbins et al found that the behavioral changes during the heel prick were significantly higher than that during changing diapers (27). In a study assessing the effectiveness of facilitated tucking in reducing pain during venous blood sampling in preterm infants, the mean pain score calculated by the PIPP in the intervention group was significantly lower than that in the control group (37). The study is consistent with the present study as it showed that PIPP can discriminate painful conditions from those after pain relief measures.
In addition, the results of a comparison between the scores of changing diapers and heel prick among the three groups of premature infants showed that the highest score was that of infants with gestational age of less than 28 weeks in both painful and non-painful procedures. A similar study shows that the pain scores of infants with gestational age of 26 - 31 weeks was higher than other infants in both painful and non-painful phases (17). Vederhus et al showed that the highest pain score at changing diapers was that of infants with gestational age of less than 28 weeks, suggesting that changing diapers as a routine non-painful procedure might lead to pain in extremely preterm infants. That is because premature infants are more sensitive to pain than other infants due to the fact that their pain modulation system is not completely developed and even a non-painful stimulation may create a pain response (29). Therefore, changing diapers may cause pain or stress in extremely preterm infants due to manipulation of the legs, pelvis, and spine (27).
The reliability of a tool means that various measurements by the tool lead to same or similar results. In other words, reliability refers to reproducibility or trustworthiness of measurement. The reliability of PIPP in the present study was a degree of stability of the research tool in determining the pain score in infants (29).
The reliability of PIPP-R was determined with two methods of inter-rater correlation and internal consistency. The inter-rater reliability in the initial study of designing the PIPP tool was reported more than 0.9 (26). However, in the initial study to validate PIPP, the neonatal pain response was evaluated by 4 raters independently and simultaneously. There was a very high correlation (0.93 - 0.96) (38). The present study is consistent with the initial study in terms of the high correlation between raters. Inter-rater reliability in the two studies that examined the psychometric properties of the tool was more than 0.90, that is, no significant difference was observed between the scores calculated by the raters at the basic, painful and non-painful phases (19, 29). In a study by Campbell-Yeo et al in 2012 to determine the effect of cobedding of twin premature infants in response to the pain of heel prick, the inter-rater reliability determined was 0.85 through the process of observing 6 videos by two professionals, independently and simultaneously (39).
PIPP tool indicators were evaluated using Cronbach’s alpha to determine the internal consistency of the tool. Internal consistency was assessed for initial development and validation of the tool (26). In an initial study, Cronbach’s alpha coefficient increased by excluding facial changes. However, in the present study, Cronbach’s alpha coefficient increased after excluding facial changes and the amount of oxygen reduction, which is not consistent with the initial study. A different sample size might be a reason for this difference. In the initial study, 124 infants with gestational age of 32 to 34 weeks were examined in order to determine the internal consistency, whereas in the present study 145 infants were examined in four different groups. Moreover, the samples in the initial study were more homogeneous. The difference might be attributed to different sampling methods and interpretation of pain scores by raters in the two studies. The Cronbach’s alpha coefficient of all 6 items in the initial study (Stevens et al, 1996) and in the present study were 0.71 and 0.78, respectively, indicating a high correlation between the two studies. The internal consistency of the tool was appropriate in both studies (26).
A study that compared three multidimensional tools, neonatal infant pain scale (NIPS (neonatal pain assessment scale) NPAS), PIPP and one uni-dimensional tool Douleur Aigue du Nouveau-ne (DAN), reflected the ease of use of DAN in clinical practices while indicating that scoring facial changes indicator would be difficult in mild to moderate pains. The NIPS assessment also indicated that the bent hands and feet positions indicator in the tool cannot differentiate between moderate and severe pain, especially in premature infants. The present study showed that since the PIPP is more accurate in the assessment of more intense pains than low-intensity pains, it can detect subtle differences in the quantity and quality of pain. In addition, since PIPP is a combination of behavioral, physiological and contextual indicators, it is a valuable tool in premature infants’ pain assessment (14).
A study by Macnair et al. in 2004 to compare the PIPP and CRIES (Crying, Requires increased oxygen administration, Increased vital signs, Expression, Sleeplessness) tools in assessing postoperative pain showed a positive and significant correlation between pain scores calculated by the PIPP and CRIES in 72 hours after surgery (40). In addition, a study by Ahn and Jun showed that the PIPP is more sensitive in showing the effect of environmental stimuli on pain in premature infants compared to CRIES (41, 42). Another tool for measuring pain in infants is neonatal pain, agitation and sedation scale (N-PASS). However, this one does not include gestational age as a variable in pain assessment (43). The pain response pattern in premature infants with different gestational ages varies (30), and pain response in premature infants is very different from term infants (28). Therefore, due to the effect of gestational age on pain scores, it can be concluded that PIPP is a more accurate pain assessment tool, particularly in premature infants. This is the only multidimensional tool that has gestational age as one of its contextual indicators intended for premature infants’ pain assessment (44).
The pain response in infants is based on a set of observable and measurable behavioral and physiological reactions such as facial expression (brow bulge, eye squeeze, nasolabial furrow), crying, increased heart rate, and decreased arterial blood oxygen saturation that the infants show in response to painful stimuli (45). Therefore, behavioral tools are not able to assess all aspects of pain which leads to inadequate infant pain assessment. Since both behavioral and physiological indicators are considered in determining pain scores in PIPP, it can be used in clinical decision-making with greater certainty.
One of the disadvantages of the tool is that all the behavioral indicators of PIPP associated with facial changes have limitations in pain assessment of NCPAP or intubated infants. PIPP can also be used for research purposes and clinical practices. However, additional equipment (heart and respiratory monitors) are needed to be used with this tool.
A limitation of the study was the lack of adequate samples in the less-than-28-week group. The reason is that most of these babies were under the ventilator for their survival in the neonatal intensive care unit.
4.1. Conclusions
The results showed that the Persian version of premature infant pain profile-revised has high construct validity and reliability and can be used as a valid tool to assess acute pain in preterm and term infants. The availability of such a tool increases the reliability of relevant studies in Iranian society and can be used for research purposes and in clinical practices.
Using a valid tool in clinical practice will reduce pain assessment errors and thus will reduce the side effects of pain in infants, especially in premature infants (21). According to the studies, if there is a specific instruction, nurses can benefit more from a valid tool in clinical practice (17). Therefore, in order to ensure the proper use of a pain assessment tool by nurses, it is essential to train them, so that they use it routinely in clinical practice. It is recommended to evaluate the feasibility of the tool in clinical practice in future studies.
As extremely preterm infants are not able to appropriately respond to painful stimuli due to their underdeveloped central nervous system, it is required that pain assessment be performed in extremely preterm, intubated, and critically ill infants with a greater sample size in various clinical situations in the future studies.