1. Background
Sleep is a core contributor to human health, particularly during adolescence, which is a time of accelerated growth and psychological development (1). Insufficient sleep in adolescents has been consistently linked to adverse mental consequences, including mood disturbances (2, 3), which have become a public health concern. The deleterious impact of inadequate sleep during week nights result in a “sleep debt”, and thus a compensatory behavior occurs on the weekend. A large sleep debt may indicate severe sleep loss during weekdays, the effects of which cannot be remedied by additional weekend sleep. Sleep debt has also been connected to poor mental health in adolescents (4).
Sleep characteristics are often inter-related, and sleep debt can be affected by sleep quantity during weekdays. However, most prior research on sleep debt has failed to consider weekday sleep duration. Additionally, to the best of our knowledge, no studies on the independent associations of sleep debt with mental health have used nationally representative samples.
2. Objectives
This analysis aimed to examine whether sleep debt is independently associated with mental health quality among adolescents in the population cohort represented by KNHANES.
3. Methods
This study was conducted using data from KNHANES. This is a nationwide survey annually conducted by the Korea Centers for Disease Control and Prevention to assess the health and nutritional status of Koreans. KNHANES is composed of three components: health interview, health examination, and nutrition survey, using a multistage, probability-based sampling design to select household units (5). The KNHANES data are publicly available. In contrast to the previous survey, the 7th KNHANES (2016 - 2017) distinguished the average sleep duration on weekdays from average sleep duration on the weekend. Of 1,514 students between 13 - 18 years old, 1,392 individuals with available data on sleep duration were included in the final analysis.
Beginning KNHANES, individuals were informed that they have been selected to participate in the survey and could refuse to participate in accordance with the National Health Enhancement Act. All participants provided written informed consent, and researchers followed the guidelines put forth in the Declaration of Helsinki. The Institutional Review Board (IRB) of the Korea Centers for Disease Control and Prevention approved the KNHANES, and the IRB of Gachon University, Gil Medical Center, approved our study protocol (GCIRB2020-028).
Height and weight were measured by a trained medical staff. Body mass index (BMI) was calculated as the proportion of weight (kg) to height2 (m2). To obtain data regarding sleep debt, we used the average weekday sleep duration and average weekend sleep duration values from the survey question, “How many hours do you usually sleep per day?” Sleep debt was calculated as weekend sleep duration minus weekday sleep duration. Demographic information (age, sex, and household income) was obtained from health interviews. We considered mental health in terms of perceived stress and depressive mood. To measure perceived stress, we used self-reported responses to the survey question “How much stress do you have in your daily life?”. Response options included “none”, “mild”, “moderate”, or “severe”. Participants who answered “moderate” or “severe” were classified into the perceived stress group. The scale for perceived usual stress was used in the other studies based on KNHANES (6). To measure depressive mood we used responses to the survey question: “Have you ever felt sadness or despair continuously for more than 2 weeks during the past year?”, to which participants responded with either “yes” or “no”. The validity of the single question on depressive mood was evaluated in previous studies (7).
Characteristics of the participants according to the presence of perceived stress or depressive mood were compared using t test or chi-square test. In the multivariate logistic regression analysis, factors associated with perceived stress or depressive mood were identified with the odds ratios (ORs) and 95% confidence intervals (CIs) after adjusting for confounding variables, including age, sex, BMI, household income, average sleep duration on weekdays, and sleep debt. All analyses were performed using STATA SE 9.2 (Stata Corp, College Station, TX, USA). All statistical tests were two-sided, and P values < 0.05 were considered statistically significant.
4. Results
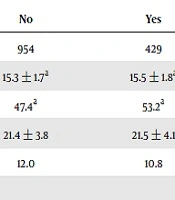
Mental health characteristics of participants are shown in Table 1. Participants in the poor mental health group were more likely to be older, and there was a higher percentage of females particularly in the group that reported depressive mood. Those in the poor mental health category also slept less on weekdays (P = 0.0006 in perceived stress and P = 0.0003 depressive mood categories) and thus had greater sleep debt (P = 0.0105 in perceived stress category). Table 2 presents the factors associated with mental health from a stepwise multivariable logistic regression analysis. In both the perceived stress and depressive mood categories, short sleep duration was positively associated with perceived stress and depressive mood.
| Perceived Stress | Depressive Mood | |||
|---|---|---|---|---|
| No | Yes | No | Yes | |
| N | 954 | 429 | 1,257 | 126 |
| Age, years | 15.3 ± 1.7a | 15.5 ± 1.8a | 15.3 ± 1.7a | 15.8 ± 1.7a |
| Female, % | 47.4a | 53.2a | 47.6a | 65.1a |
| Body mass index, kg/m2 | 21.4 ± 3.8 | 21.5 ± 4.1 | 21.4 ± 3.9 | 21.2 ± 3.7 |
| Low economic statusb, % | 12.0 | 10.8 | 11.6 | 11.9 |
| Mean sleep duration, h | ||||
| On weekdays | 7.0 ± 1.2a | 6.7 ± 1.3a | 6.9 ± 1.2a | 6.5 ± 1.4a |
| On weekend | 8.8 ± 1.5 | 8.8 ± 1.8 | 8.8 ± 1.6 | 8.6 ± 1.8 |
| Sleep debt | 1.8 ± 1.6a | 2.1 ± 1.9a | 1.9 ± 1.7 | 2.1 ± 2.1 |
aStatistical significance (P < 0.05) from t-test or chi-squared test
bThe lowest quartile of household income
aFrom the stepwise multivariate logistic regression models
bThe lowest quartile (vs. others)
5. Discussion
In this nationally representative study, we aimed to examine the associations between sleep debt and mental health among Korean adolescents. We did not identify any relationships between sleep debt and mental health among school-age adolescents. Rather, short sleep duration is a significant factor associated with perceived stress and depressive mood.
There is a lack of data on the impact of sleep debt resulting from short sleep duration during weekdays on mental health. A recent review indicated that sleep debt was positively correlated with depressive symptoms or perceived stress levels in adolescent populations (4). However, just one study considered weekday sleep duration as a potential covariate, which is consistent with the findings from our study. In a self-report survey of 242 high school students, sleep debt was not related with depressive symptoms when controlling for potential confounding factors, such as weekday sleep duration (8).
There is consistent evidence supporting the relationship between sleep deficits and negative mental health outcomes (1). Restricting sleep in adolescents leads to mood disorders, such as depression and anxiety as well as lower positive affect scores (9, 10). Furthermore, an earlier interventional study verified that increasing sleep duration on weekdays reduces depressive mood or irritability in students (11).
Some limitations should be admitted in interpreting our results. First, the cross-sectional design of our study precludes a causal inference between sleep characteristics and mental health. Sleep debt may reflect a circadian rhythm misalignment, such as the delayed sleep phase syndrome, leading to subsequent poor mental health (12). Second, we used self-report to measure sleep patterns rather than objective measures of sleep, and misclassification bias could occur due to the use of a simple questionnaire to evaluate stress and depressive mood. Third, our results may overestimate the effect of shortened sleep duration because students in Asian countries tend to sleep for shorter time periods compared with students in non-Asian countries (13). Finally, in the present study, we were not able to assess all possible dimensions of sleep or some barriers for sleep, such as caffeine intake or the use of electronic devices before bedtime. It may be interesting to examine those additional measures, for example, sleep-wake patterns or sleep quality (14). Future work is needed in alternate populations, employing longitudinal study designs and using objective sleep measures to corroborate and expand upon our findings.
In conclusion, mental health among Korean adolescents was not associated with sleep debt, but with short sleep on weekdays. Our study highlights the importance of attaining sufficient weekday sleep for optimal mental health in adolescents. In addition, weekday sleep duration should be considered as a critical variable in the future sleep research.