1. Background
Children comprise a substantial percentage of the world’s population. For this reason, maintaining and promoting their health are among the first health priorities (1). As the most common endocrine disorder, diabetes is nowadays increasing in prevalence among children and adolescents worldwide (2-4). Studies have indicated that diabetic children are at risk of developing other diseases such as depression (5, 6). Researchers believe that younger individuals, especially children, suffer from depression more than the general population (7). Nevertheless, it frequently goes undiagnosed and untreated because its symptoms are passed off as normal psychological and emotional changes that take place during growth (8). Some signs of depression in children include a sad look, a feeling of distress, decreased interest in activities children found pleasurable before developing diabetes, worsening school performance, social withdrawal from friends or after-school activities, and a talk of suicide (9). The comorbidity of depression and diabetes may lead to decreased metabolic control, weakness, noncompliance with treatment, the poor quality of life, increased medical care costs, increased insulin requirements, an increased risk of macrovascular and microvascular complications, and even a premature death (10).
The enormous burden of diabetes and depression both nationwide and worldwide, the necessity of diagnosing and treating depression of children as shapers of the country’s future have all necessitated considering the mental health of the diabetic children. Indeed, some studies on diabetes and depression have been conducted during the past decades in the world (11-20). However, it is not long since such studies were undertaken in diabetic children in Iran. Nonetheless, these studies have examined only very few variables such as the quality of life of patients, effects of education and therapies such as behavioral therapy on the control of their anxiety and depression, and injection-induced anxiety in patients with insulin-treated diabetes (21-24). Therefore, it is found necessary to conduct a relevant and comprehensive study. A study that looks at the relationship between more different variables and depression in children with diabetes.
2. Objectives
The main object of this study was to determine the association between diabetes mellitus and depression in diabetic children who had attended the Endocrinology and Metabolism Clinic of a Children’s Medical Center in Tehran, and identify risk factors associated with the presence of depression in these diabetic children.
3. Methods
In this cross-sectional study, the population consisted of diabetic children who attended the Endocrinology and Metabolism Clinic of the Children’s Medical Center affiliated to Tehran University of Medical Sciences in 2018. The study was approved by the Ethics Committee of Tehran University of Medical Sciences (code: IR.TUMS.MEDICINE.REC.13.96.2929).
Inclusion criteria were the children in the 7 - 16 age range with type 1 diabetes; with a minimum disease duration of three months since the onset having a basic level of literateness, and parental consent for participating in the study. Exclusion criteria were suffering from other serious medical problems other than diabetes, or having history of a common childhood psychiatric disorder.
Convenience sampling was used in the study. The sample size with alpha = 0.05 and power = 80% was estimated 125. Depression in diabetic children was assessed using the children’s depression inventory (CDI), which is a 27-item self-report questionnaire. This questionnaire had previously been translated into Persian by Rajabi and Atari (25). It quantifies depressive symptoms mood disturbances, anhedonia, vegetative disturbances, interpersonal problems, and negative self-esteem. The child selects the choice that best describes feelings he or she had over the two weeks prior to completing the evaluation. Responses are scored on a 0 - 2 scale with 0 representing the absence of a depressive symptom and 2 representing the severe form of the symptom. The total score ranges between 0 and 54. Those who score below the cut-off point are considered to have depressive symptoms. In addition, the child’s score in the assessment shows the severity of his or her depression. In different studies, the optimal cut-off point for the CDI varies, ranging from 10 to 20 (26). In the present research, it is 20.
The following data were acquired: age, gender, disease duration, frequency of hospitalization due to problems resulting from diabetes, frequency of injections, number of injected insulin units, insulin injection tools, frequency of blood glucose monitoring, number of children in the family, level of parental education, and socioeconomic status of family. Questionnaire about demographic characteristics of the patients was filled out by the researchers.
The level of HbA1c was recorded using laboratory reports the patients had taken with to the clinic.
3.1. Statistical Analysis
The data were analyzed using the SPSS 18. The mean and standard deviation were calculated for quantitative variables and the frequency and percentage were measured for qualitative variables. The Kolmogorov-Smirnov test was used to test the normality of data, the means comparison between the three groups (depressed, borderline, non-depressed) were done using ANOVA (for comparison of age) and nonparametric Kruskal-Wallis test (for comparison of BMI) for continuous outcomes, while chi-square and Cramer’s V-test used for categorical outcomes (gender, socioeconomic status and insulin injection tools). The Pearson’s correlation coefficient was used to examine the correlation between quantitative variables such as frequency of hospitalization due to problems resulting from diabetes, frequency of injections, number of injected insulin units and level of parental education with score of depression test. The linear regression analysis (stepwise) was used to test whether the proposed association between the dependent variable (depression score) and the predictor independent variables was significant or not and also to provide a risk predictive model to estimate the probability of a diabetic child experiencing depression. A P value less than 0.05 was set as the level of statistical significance.
4. Results
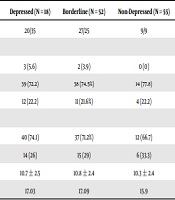
Of 125 children, 69 (55.2%) were male. Their mean age was 10.82 ± 2.4 years. The study showed that 18 (14.4%) of the children were depressed (score > 20), 52 (41.6%) borderline (score 9 - 19) and 55 (44%) non-depressed (score 0 - 8). The median of depression score for the depressed, borderline and non-depressed children were, respectively, 22, 12, and 6.
As shown in Table 1, the average of age (P = 0.62) and BMI (P = 0.64) did not differ significantly among the three groups. In the depressed and borderline groups, girls had the majority, although the difference was not significant (P = 0.24). In all three groups, the majority lay in the middle socio-economic status (P = 0.89) and the majority used insulin pen as injection tool (P = 0.82), however the differences were not significant.
| Variable | Depressed (N = 18) | Borderline (N = 52) | Non-Depressed (N = 55) | Chi-Square Value | Cramer’s V Value | P Value |
|---|---|---|---|---|---|---|
| Gender (boy/girl) | 20/35 | 27/25 | 9/9 | 2.84 | 0.15 | 0.24 |
| Socio economic status | 1.1 | 0.07 | 0.89 | |||
| High | 3 (5.6) | 2 (3.9) | 0 (0) | |||
| Middle | 39 (72.2) | 38 (74.5%) | 14 (77.8) | |||
| Low | 12 (22.2) | 11 (21.6%) | 4 (22.2) | |||
| Insulin injection tools | 0.38 | 0.06 | 0.82 | |||
| Pen | 40 (74.1) | 37 (71.2%) | 12 (66.7) | |||
| Syringe | 14 (26) | 15 (29) | 6 (33.3) | |||
| Age | 10.7 ± 2.5 | 10.8 ± 2.4 | 10.3 ± 2.4 | - | - | 0.62 |
| BMI, kg/m2, Median | 17.03 | 17.09 | 15.9 | - | - | 0.64 |
Association Between Depression, Patients’ Characteristics and Insulin Injection Toolsa
As shown in Table 2, depression score was significantly increased by increasing the HbA1c level (P = 0.03), the frequency of hospitalization (P = 0.04) and inversely related to increased parental education (P = 0.01 and < 0.001).
| Factor | Number of Children in the Family | Disease Duration | HbA1c | Frequency of Hospitalization | Frequency of Injection | Number of Injected Units Per Day | Mother’s Education (Number of Years) | Father`s Education (Number of Years) | Frequency of Blood Glucose Monitoring Per Day |
|---|---|---|---|---|---|---|---|---|---|
| CDI Score Pearson correlation | 0.04 | 0.04 | 0.21 | 0.18 | -0.14 | 0.09 | -0.28 | -0.24 | -0.001 |
| P value | 0.66 | 0.66 | 0.03 | 0.04 | 0.13 | 0.33 | < 0.001 | 0.01 | 0.95 |
The Association Between Score of Children’s Depression Inventory and patient’s Other Characteristics and Disease Related Factors
There was not significant association between depression score in diabetic children with the frequency of injections, disease duration, the number of injected units, the frequency of blood glucose monitoring, and the number of children in the family (Table 2).
Table 3 shows the results of the linear regression analysis. These results demonstrate that the risk of depression in the diabetic child can be predicted by the mother’s educational level and frequency of child’s hospitalization. The risk predictive model is given as follows:
Y= 13.4 - 0.4*(mother’s educational level) + 1.2 × (The frequency of hospitalization)
| Unstandardized Coefficients | Standardized Coefficients | P Value | 95.0% Confidence Interval for B | |||
|---|---|---|---|---|---|---|
| B | Standard Error | Beta | Lower Bound | Upper Bound | ||
| Constant | 13.4 | 2 | < 0.001 | 9.4 | 17.4 | |
| Mother’s education | -0.4 | 0.2 | -0.2 | 0.02 | -0.7 | -0.06 |
| Frequency of hospitalization | 1.2 | 0.6 | 0.2 | 0.04 | 0.08 | 2.4 |
Results of Linear Regression Analysisa
According to this regression equation for one unit of increasing in maternal education, the depression score decreases by 0.4, and for one unit increasing in the frequency of hospitalization, the depression score increases by 1.2 units.
5. Discussion
The results of this research showed that 14.4% of the children suffered from depression. Sendela et al. (27) had previously achieved similar results in a study on the prevalence of depressive symptoms in school-aged diabetic children. They reported that 17% of the children presented with depressive symptoms (27). Likewise, in Butwicka et al.’s study (28) of diabetic children, 26.6% of patients revealed mental disorders. Rzeszut (29) has reported the most severe psychological problems in diabetic children was anxiety disorders with a frequency of 15.5% and then mood disorders such as depression with a frequency of 6.7%. Besides, according to his study, certain phobias, such as severe fear of injections are common in these children (29). Khosroshahi and Khanjani (30) compared diabetics and nondiabetics with respect to the quality of life and the level of depression. According to their results, diabetics suffer from depression, suicidal thoughts, state and trait anxiety, and violence due to socio-psychological stresses (30). The results of these studies are consistent with those of the current study. In justifying this finding, it could be mentioned that dietary restrictions, drug treatment, blood sugar control, and poor clinical outcomes, concerns about possible harm, social and family crisis, and maladaptation are among the causes of depression in diabetic patient (31). Likewise, chronic distress associated with the recurrence of treatment procedures, apart from the effect of the disease itself, can also put the child at risk for psychological and behavioral disorders and hurt his or her adjustment (32). However, the claim that the prevalence of depression, as a debilitating disease with complications, in Iranian diabetic children is always more than the general population apparently requires detailed studies. There is similarly a second hypothesis regarding the relationship between diabetes and depression, which identifies depression as the fundamental cause of diabetes, this issue makes it difficult to determine which disease has previously affected the child. In any case, depression has a substantial effect on the course and outcome of diabetes, altering the quality of life, poor blood sugar control, high complications of the disease, mortality, and increased costs of care and financial burden for the family (31). So, in the treatment of these children, should not only the physical signs and symptoms of the disease be eliminated, but the quality of life of this group and issues such as anxiety and depression should also be reflected.
The results of the present study showed that depression in the diabetic children was not significantly related to age, gender, injection tools, BMI, disease duration, frequency of injections, the number of injected units, frequency of blood glucose monitoring, number of children in the family, and socio economic status. Park indicated that the most important risk factors associated with depression in diabetics were old age, diabetic complications, female gender, low income, and medications received orally or by injection (33). It can be said, with some justification, that the discrepancy between the results arose from social and cultural distinctions and, moreover, differences in facilities available to the samples and data-collection tools. However, the age of the target community and the sample was the most important distinction between the above-mentioned studies and the present one. For example, the study by Park was conducted on adults. Furthermore, a study by Lernmarket al. (12) reported that factors such as age, gender, the general quality of life, insulin dosage, and disease duration proved ineffective. Therefore, the identification of depression in children and factors behind it using self-report techniques is problematic. Due to the complex nature of depression in children, it is recommended that, while designing future research projects, the significance of the above-mentioned factors be considered with respect to the underlying context, onset, progression, and exacerbation of the disease.
The results of this study also showed that depression in diabetic children was significantly associated with the level of parent’s education, frequency of hospitalization, and HbA1c level. Hashim and Rahman (34) achieved similar results. Their study revealed that depressive symptoms in children and adolescents were significantly correlated with the HbA1c level and the frequency of hospitalization in a six-month period. Puri et al. (35) carried out research on the quality of life of Indian children and adolescents with diabetes and concluded that the elevated HbA1c level was associated with a higher prevalence of depression. Furthermore, results of Jansouz et al.’s (36) study on Iranian children with diabetes are consistent with the results of the current research with respect to the role of metabolic control, the frequency of hospitalization, and the level of parental education. Mosaku et al. (37) indicated that people with low blood sugar control were significantly more likely to show signs of anxiety. The presence of these symptoms, particularly depression, meaningfully reduces the recovery chances and affects patients’ sense of well-being (37). Allen’s study found that in the group with the most behavioral disorders, the mean HbA1C was significantly higher (38). Westrupp et al. (39) states parents of children with the disorder believe they can often detect fluctuations in their child’s blood sugar levels from their behaviors. High blood sugar causes damage to a child’s cognitive function, negativism, negative mood, and isolation (39). On the other hand, studies have revealed that if depression affects people’s behavior, it can be effective in predicting HbA1C levels (40). At large, the amount of HbA1c is an indicator of diabetes-related metabolic control. Diabetes treatment aims to reach the normal level of glycated hemoglobin in the blood. The high level of hemoglobin indicates the severity of the disease. Sobhi et al. (41), in a study recommended measuring the relationship between these children’s behavioral problems and HbA1c. The mechanism of the relationship between HbA1c and depression in diabetic patients is that it is associated with inadequate blood sugar control and decreased physical function, poor glycemic control and increased A1C (31). Based on these findings, optimal metabolic control seems to reduce not only their HbA1c level but also the frequency of their hospitalization (due largely to diabetic ketoacidosis). Nevertheless, it is uncertain whether strict blood glucose monitoring with the aim of reducing the risk of mental disorders in the diabetic children will ultimately benefit them or not. Hence, it is necessary to conduct further studies because the more we obsess about blood glucose monitoring and a reduction in the HbA1C level, the higher the risk of hypoglycemic attacks will be. These attacks not only cause physical dangers but also affect children’s compliance with treatment in the future.
A detailed analysis in this study revealed that increased level of mother’s education predicts decreased chance of child depression. To support this statement, it could be said that mothers are commonly considered to have the main responsibility for the care of children when they develop a chronic disease. Diabetes is considered a family disease. Having a child with a disease is stressful for parents. Experiencing an unpleasant lifestyle after diagnosing of childhood diabetes, social and communication limitations and mental disorders resulting from diabetes management, has been reported to be a major cause of poor quality of life for parents of diabetic children (42). Parental adjustment can affect the health of a diabetic child. When parents, especially mothers, feel competent in stressful situations, they will be able to support their sick child and make the treatment process possible for him/her (43). Education enables mothers to have a better understanding of the disease mechanism and its complications and improves their adaptation to the disease and their children’s compliance. There are studies that reported the role of educated mothers in controlling the disease of diabetic children and their adaptation to specific circumstances caused by the disease (44). Al-Odayani et al.’s (44) study demonstrated that there is a significant association between mothers’ knowledge of diabetes and their diabetic children’s HbA1C level.
Given that the data-collection tool was a questionnaire, respondents may have overestimated or underestimated their depressive symptoms. This was one of the limitations of the current study. Moreover, using the present results, one cannot claim that diabetic children are more at risk of depression than healthy children of the same age. Therefore, it is recommended that studies be conducted to simultaneously examine these two groups (i.e., healthy and unhealthy).
5.1. Conclusions
In this study, depression in the diabetic children was associated with the frequency of hospitalization and the HbA1c level. In other words, there appears to be a relationship between the remission of depression and optimal metabolic control, which reduces both the HbA1c level in children and the number of times they are hospitalized. Furthermore, the educational level of the parents, especially mother, can reduce the risk of depression in the diabetic.