1. Background
Currently, Coronavirus Disease 2019 (COVID-19) has attracted global attention for unexpected rapidly spread attributed to extensive traveling among countries. Until February 24, 77658 cases were confirmed in China within just two months, leading to 2663 deaths (1). Around 1630 (2.1%) cases were children under ten years old (2). Compared to adults, pediatric patients were fewer and disease manifestation in them milder (3). Since many suspected patients were in quarantine, the actual number of infected cases may increase with widely used pathogen tests.
With the disease spreading, people pay more attention to COVID-19 and find that COVID-19 seems to have a lower fatality, but higher infectivity compared with the Middle East respiratory syndrome (MERS) and the severe acute respiratory syndrome (SARS) (4). Although only two severe pediatric cases were reported in China and no cases of death, we still need to be vigilant as children are a particular population. Children are susceptible to be infected with respiratory viruses due to the immature immune system and respiratory tract structure (5).
The spread of COVID-19 among children is mainly conducted by human-to-human in family settings (6). Their clinical symptoms may be diverse and atypical, even without symptoms, and the incubation period could be more than 14 days, all of these make the diagnosis more difficult (7). It is worth noting that since respiratory viruses are common during the fall and winter, children with COVID-19 also could be infected with other viruses.
2. Objectives
Although there are many diagnosis and treatment recommendations, prevention and isolation remain the primary effective control measures. Since it is a new challenge never met before, we designed this study to summarize the characteristics of pediatric patients with COVID.
3. Methods
3.1. Study Design and Participants
This retrospective study was performed from January 17 to February 24, 2020, at Xiangyang Central Hospital. A total of 166 suspected child patients were admitted, and eight of these patients were diagnosed with laboratory-confirmed COVID-19 by quantitative real-time reverse transcription-PCR using nasopharyngeal swab specimens. Three children had negative nCoV-RNA tests at first, the results became positive after 3 to 5 days follow-up. Eight patients with laboratory-confirmed SARS-CoV-2 were finally enrolled based on the “Diagnosis, Treatment, and Prevention of 2019 Novel Coronavirus Infection in Children: Experts’ Consensus Statment” (8).
This study was approved by the Ethics Committee of Xiangyang Central Hospital. Written informed consent was not obtained as the study was retrospective.
3.2. Data Collection
The final data, containing epidemiological, clinical manifestation, laboratory indicators, radiological features, treatment and outcomes, were obtained from the electronic medical records. After admission, nucleic acid test and high-resolution CT pulmonary scanning were performed immediately. We collected clinical manifestations data of all suspected patients, including fever, fatigue, dry cough, expectoration, running nose, pharyngalgia, headache, and some gastrointestinal symptoms such as abdominal discomfort, abdominal pain, nausea, vomiting, diarrhea. Laboratory examinations were obtained, including blood routine, blood clotting index, hepatorenal function, myocardial enzyme, procalcitonin (PCT), C reactive protein (CRP), erythrocyte sedimentation rate (ESR), and other pathogens as influenza B, mycoplasma pneumoniae, chlamydia pneumoniae. Typical CT findings were defined as interstitial changes and multiple small plaques in the lung periphery at early-stage, with further deteriorated to bilateral multiple ground-glass opacities or infiltrating shadows. Lung consolidation was observed in severe cases; pleural effusion was rare. The normal range of white blood cell (WBC) counts was 5 - 10 × 109/L while lymphocyte counts were 1.1 - 3.2 × 109/L. Suspected cases were defined as those who had an epidemiological history and two of the following clinical manifestations: (a) Fever, fatigue, dry cough; (b) chest CT findings as mentioned above; (c) in the early stage, WBC count was normal or decreased, or lymphocyte count decreased; (d) no other pathogens were detected to explain the clinical manifestations. Confirmed cases were defined as suspected cases with 2019-nCoV nucleic acid positive. The release and discharge criteria included: (a) normal body temperature for more than three days in a row; (b) obvious improvement of the respiratory symptoms; (c) negative nCoV-RNA finding in two consecutive tests with an interval of at least one day (9).
4. Results
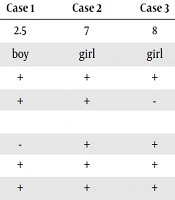
All patients aged from 1 to 14 years (Table 1). Five were boys, and three were girls. Two patients (25%) had underlying diseases: congenital ventricular septal defect in case 1 and cough variant asthma in case 2. Seven children (87.5%) associated with a family cluster outbreak. According to clinical manifestation, they were categorized into 3 types: 1 common case (case 3, 12.5%), 4 mild cases (cases 1, 2, 4 and 5, 50%), and 3 asymptomatic cases (cases 6 - 8, 37.5%). Fever was observed in cases 2 - 5 (50%); cough, expectoration and sore throat were seen in cases 1 - 3 (37.5%). Case 4 also had an occasional mild headache. Their breathing rate, heart rate, blood pressure, and blood oxygen saturation were stable.
| Items | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 |
|---|---|---|---|---|---|---|---|---|
| Age (year) | 2.5 | 7 | 8 | 9 | 1 | 7 | 14 | 11 |
| Sex | boy | girl | girl | boy | boy | girl | boy | boy |
| Exposure history | + | + | + | + | - | + | + | + |
| Comorbidities | + | + | - | - | - | - | - | - |
| Signs and symptoms | ||||||||
| Fever | - | + | + | + | + | - | - | - |
| Cough | + | + | + | - | - | - | - | - |
| Expectoration | + | + | + | - | - | - | - | - |
| Pharyngalgia | + | + | + | - | - | - | - | - |
| Headache | - | - | - | + | - | - | - | - |
| Pathogens | ||||||||
| nCoV-RNA | -a | -a | + | + | + | + | -a | + |
| Influenza B | - | - | + | - | - | - | - | - |
| Mycoplasma pneumonia | - | + | - | - | - | - | - | - |
| Chlamydia pneumonia | - | + | - | - | - | - | - | - |
| Chest CT scan | +b | +c | +b | +d | +b | - | +e | +c |
| Laboratory results | ||||||||
| WBC (× G/L) | 7.19 | 5.36 | 3.36 | 2.32 | 6.35 | 4.15 | 12.07 | 5.40 |
| Neutrophil (× G/L) | 19.20 | 37.40 | 32.70 | 32 | 4.32 | 41.70 | 45.70 | 37 |
| Lymphocyte (× G/L) | 65.60 | 50.70 | 53 | 60 | 3.41 | 44.10 | 47.60 | 43.70 |
| Monocyte (× G/L) | 10.20 | 5.60 | 12.50 | 8 | 7.13 | 10.80 | 45.40 | 10.20 |
| D-dimer (mg/L) | 0.38 | NA | 0.26 | 6.28 | 0.63 | 0.32 | NA | 0.14 |
| CK (U/L) | 222 | 130 | NA | 73 | 119 | 70 | 72 | 45 |
| CK-MB (U/L) | 19 | 8 | NA | 27 | 21 | 8 | 5 | 16 |
| LDH (U/L) | 395 | 269 | NA | 196 | 338 | 236 | 153 | 208 |
| ALT (U/L) | 14 | 11 | 11 | 14 | 9 | 23 | 29 | 13 |
| AST (U/L) | 50 | 26 | 22 | 25 | 37 | 28 | 16 | 22 |
| UN (mmol/L) | 4.40 | 4.0 | 3.00 | 2.70 | 3.90 | 6.20 | 3.90 | 4.90 |
| Scr (µmol/L) | 20.20 | 36.90 | 28.80 | 28.70 | 27.80 | 32.90 | 42.80 | 53.70 |
| PCT (ng/mL) | 0.03 | NA | NA | NA | 0.13 | 0.04 | NA | 0.03 |
| CRP (mg/L) | 5 | 3.02 | 4.49 | 5.01 | 5 | NA | - | - |
| Treatment | ||||||||
| Oxygen therapy | - | - | + | - | - | - | - | - |
| Antiviral therapy | + | + | + | + | + | + | + | + |
| Antibiotic treatment | + | + | - | - | + | - | + | - |
| Glucocorticoid therapy | - | + | - | - | - | - | - | - |
| Interferon therapy | + | - | - | - | - | - | - | - |
| TCM | - | + | + | + | - | - | - | + |
| Days of hospital stay (d) | 14 | 7 | 17 | 17 | 11 | 14 | 13 | 19 |
| Duration of illness (d) | 18 | 11 | 18 | 18 | 14 | 15 | 16 | 20 |
| Clinical outcome | D | D | D | D | D | D | D | D |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CK, creatine kinase; CK-MB, creatine kinase-MB; CRP, C reactive protein; D, discharge; LDH, lactate dehydrogenase; NA, not available; PCT, procalcitonin; Scr, serum creatinine; TCM, traditional Chinese medicine; UN, urea nitrogen; WBC, white blood cell
aThree children had negative nCoV-RNA tests at first, then had positive results after 3 to 5 days follow-up
bScattered patchy ground-glass opacities in both lungs
cPatchy lesions in the upper lobe of the right lung
dMultiply ground-glass opacities and patchy lesions in the middle and lower lobes of the right lung
eGround-glass opacity in the lower lobe of the left lung
Besides COVID, two patients were infected with other pathogens: Case 3 (12.5%) combined with influenza B; case 2 (12.5%) combined with mycoplasma pneumoniae and chlamydia pneumoniae (Table 1). WBC counts of 5 patients were normal (62.5%); only case 7 (12.5%) had more than 10 × 109/L; in cases 3 and 4 (25%) it as less than 4 × 109/L. Neutrophils counts of 6 cases (cases 1 to 4, 6, and 8, 75%) decreased. Lymphocyte counts of 6 cases (cases 1 to 4, 6, and 8, 75%) and monocyte counts of 4 cases (cases 1, 3, 6, and 8,50%) increased. Two patients (cases 4 to 5, 25%) had mild increased D-dimer, three patients (cases 1, 2 and 5, 37.5%) had increased serum lactate dehydrogenase, and six patients (cases 1 to 5, and case 8, 75%) had decreased serum creatinine. However, other biochemical items were normal, including PCT, CRP, and ESR.
Every patient had received chest CT scanning after admission. The first CT imaging of 7 cases (87.5%) showed pneumonia except case 6 (Table 1), whose follow-up CT images after three days showed virus pneumonia. Follow-up CT scans indicated their pneumonia relieved.
All patients were given antiviral treatment (lopinavir/ritonavir oral solution) (Table 1). Case 3 also took oseltamivir phosphate granules for the disease being combined with influenza B and received intermittent oxygen inhalation due to unstable blood oxygen. Four cases (50%) received antibiotic treatment (azithromycin) as combined with mycoplasma pneumoniae and chlamydia pneumonia. Four patients (cases 2, 3, 4 and 8) also received traditional Chinese medicine (TCM), which was made from glycyrrhiza, bitter almond, ephedra, gypsum, amomum, reed root, and trichosanthes.
According to the criteria (9), all patients were discharged within three weeks. The follow-up was ended after two negative nucleic acid tests (one test per week). No poor prognosis or recurrence was found during the follow-up period.
5. Discussion
No case of death was reported among pediatric patients to date; only two children with severe novel corona virus pneumonia (NCP) are published. However, the risk of death remains to be taken into account since pediatric death cases were reported during the SARS and MERS epidemics (10, 11). The clinical features of children with COVID-19 are variable. The primary presentations are respiratory symptoms such as fever, cough, and expectoration, while the gastrointestinal symptoms including nausea, vomiting, and diarrhea are uncommon (5). Three patients without overt symptoms were diagnosed with RNA test due to their family exposure. Since the parents of case 5 denied any exposure history, we consider he could be infected through aerosols. Aerosols are a suspension system of solid or liquid particles in air. The droplet nucleus containing novel coronavirus could hover in the air for a long time. Flushing toilets may also generate aerosols leading to diffusion (12). Since excretion can also produce aerosols, it is unlikely that NCP spread through the fecal-oral route, aerosols and breathing may serve as the main routes of transmission.
After admission, blood routine tests showed often normal WBC counts; case 7 had more than 10 × 109/L, indicating an accompanying bacterial infection; cases 3 and 4 had less than 4 × 109/L, which met the diagnostic criteria of COVD-19. Case 1, 2, 5 had slightly increased D-dimer and LDH levels while in other cases these were normal, high levels being features of severe cases (8). Due to the above results, blood routine test can provide the clue for mild virus infection in pediatric patients. Typical images of NCP showed single or multiple patchy or nodular ground-glass shadows accompanied by septal thickening (13). Our research indicated that the most pulmonary CT findings were high-density shadows. The primary CT features included multiple ground-glass opacities (cases 1, 3, 4, 5, and 7) and patchy lesions (cases 4 and 8). Case 6 had a normal chest CT result on admission. Yet, the follow-up CT scan showed multiple ground-glass opacities mainly located in the subpleural area of both lungs after three days. Ground-glass opacities were the most common CT features, with a ratio of 14% to 77% in recently published studies (14-16), which were consistent with our CT findings. However, the CT images of NCP were diverse and overlapped with other inflammatory conditions sometimes. For those patients with atypical imaging features, we need to identify NCP by combining clinical characteristics and nucleic acid test.
Although a variety of guides and experts’ consensuses recommend lots of treatment options, there is no specific treatment for COVID-19. The key measures to control the disease are early diagnosis and isolation. In the early stage, the essential treatment for infected patients was antiviral therapy with supportive treatment. All treatments were based on the “Diagnosis, Treatment, and Prevention of 2019 Novel Coronavirus Infection in Children: Experts’ Consensus Statment” (8), which also recommended TCM. TCM primarily functions to remove heat from the lungs to relieve cough, to clear heat and remove toxicity, and to increase immunity (17). The Chinese herbals we used mainly include glycyrrhiza, bitter almond, ephedra, etc. Case 1 and case 2 were treated with atomizing inhalation according to their corresponding respiratory symptoms. In China, all hospitals responsible for the treatment of COVID-19 patients are assigned by the government. In these hospitals, patients are treated in single rooms equipped with independent oxygen sources to minimize the risk that COVID-19 may transmit through aerosol. Because of the particularities and limitations of pediatric patients, the safety and efficacy of nebulizer therapy for children need to be further confirmed. All patients were discharged within three weeks with a good prognosis, and no poor prognosis or recurrence was found after 14 days follow-up.
5.1. Limitations
This report, as a retrospective study, has its limitations. It is a single-center study with only 8 confirmed cases, which may have impact on the representativeness of the conclusions. Besides, many asymptomatic and mild patients maybe have not referred to the hospital. So, it was tough to recruit sufficient patients for our research. As for the present cases, we have done a lot of work to ensure the rigor of the research. All patients enrolled in our study were jointly diagnosed and treated by a multidisciplinary diagnosis and treatment team composed of respiratory medicine staff, infectious disease experts, emergency medical staff, and critical care medical staff. Therefore, our results are reliable. In future, we will conduct multicenter studies to analyze the characteristics of pediatric COVID-19 patients.
5.2. Conclusions
Pediatric patients with COVID-19 were mainly transfected through family cluster outbreaks. The common clinical manifestations were mild without a typical pattern. High-resolution CT and nCoV-RNA tests have great value for early-stage diagnosis.