1. Background
A concealed penis is a congenital anomaly that affects the appearance and function of genitalia in children and adults. The causes of concealed penis mainly include inadequate outer penile skin, narrow opening of the prepuce, hypoplasia of the penile sarcolemma, lack of elasticity, abnormal attachment of the sarcolemma to deep tissues, inadequate subcutaneous attachment to Buck’s fascia, fat accumulation above the pubic arch, and a tight phimosis (1-4). A literature search indicated that there are several classifications of concealed penis. In 1977, Crawford described the terms of concealed penis, buried penis and webbed penis (5). Based on the mechanism of concealment, Maizels et al. (6) described a classification of 4 subtypes, including buried penis, trapped penis, webbed penis and micropenis, which are helpful for understanding pathophysiology (7, 8). Shirley Tsang demonstrated that micropenis is different from concealed penises, which was further categorized as buried penis, webbed penis and trapped penis (9). A micropenis is characterized by a small penis with a median raphe, glans and no hypospadias. In contrast, concealed penis is normal in size but looks small, and is concealed in the subcutaneous tissue. Buried penis is a typical-sized penis that is enclosed in the fat pad due to lack of skin attached to the shaft. Trapped penis refers to the penis wrapped by dense cicatricial scar, usually caused by excessive circumcision. Webbed penis is caused by the scrotal skin extending to the abdominal penis, resulting in the penis buried in the scrotum or tethered to the scrotal midline by a fold or web of skin. These abnormal penis types are more common in infants and prepubertal boys. Most patients or these parents will seek medical consultation for their abnormal penis appearance. In general, an experienced physician can diagnose the type of abnormal penis by careful observation and provide the appropriate treatment. Trapped penis and webbed penis are easier to distinguish from another abnormal penis. However, congenital concealed penis is easily confused with phimosis and obesity-caused concealed penis (named obesity concealed penis in this study), especially for non-clinical personnel or inexperienced physicians. Excessive suprapubic fat is also the cause of concealed penis in children (10). For concealed penis caused by obesity, the penis may gradually return to normal after weight loss. However, reconstruction or surgery for the concealed penis will be delayed when the condition is mistakenly attributed to the patients’ obesity.
Concealed penis not only affects the appearance of males, but long-term penile concealment also affects its structure and function (11). These anomalies are often accompanied by multiple urologic concerns in adulthood, including sexual dysfunction, voiding dysfunction, and health problems. As a result, these patients often suffer severe psychological distress, and their quality of life may be negatively affected, especially in terms of body image and psychology (12-14). Surgical repair is still the primary treatment for concealed penis (15). Devine surgery and modified Devine surgery were often used for children with congenital concealed penis and showed good postoperative outcomes (10, 16). However, the identification of congenital concealed penis and obesity concealed penis still lacks auxiliary diagnostic indicators. The type of concealed penis is usually distinguished based on the experience of the physician. However, it will not be easy for inexperienced physicians to identify different types of concealed penis, and thus some patients may receive the unnecessary surgery or delayed treatment. This unnecessary treatment does not improve the disease and makes subsequent corrective treatment more difficult (17-19) and brings huge psychological stress on patients (4).
2. Objectives
Therefore, there is an urgent need to provide an auxiliary recognition method to provide clinicians in determining the type of concealed penis of patients and reduce the occurrence of misjudgments.
3. Methods
From July 2016 to September 2018, a total of 271 children over 6 months of age were recruited from Xuzhou Children’s Hospital in China. This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethical Committee of Xuzhou Children’s Hospital (#ETYY2016037). Written informed consent has been obtained from the patients or legal guardians of all children. The participants were recruited based on the diagnostic criteria of Campbell-Walsh Urology, 11th edition,
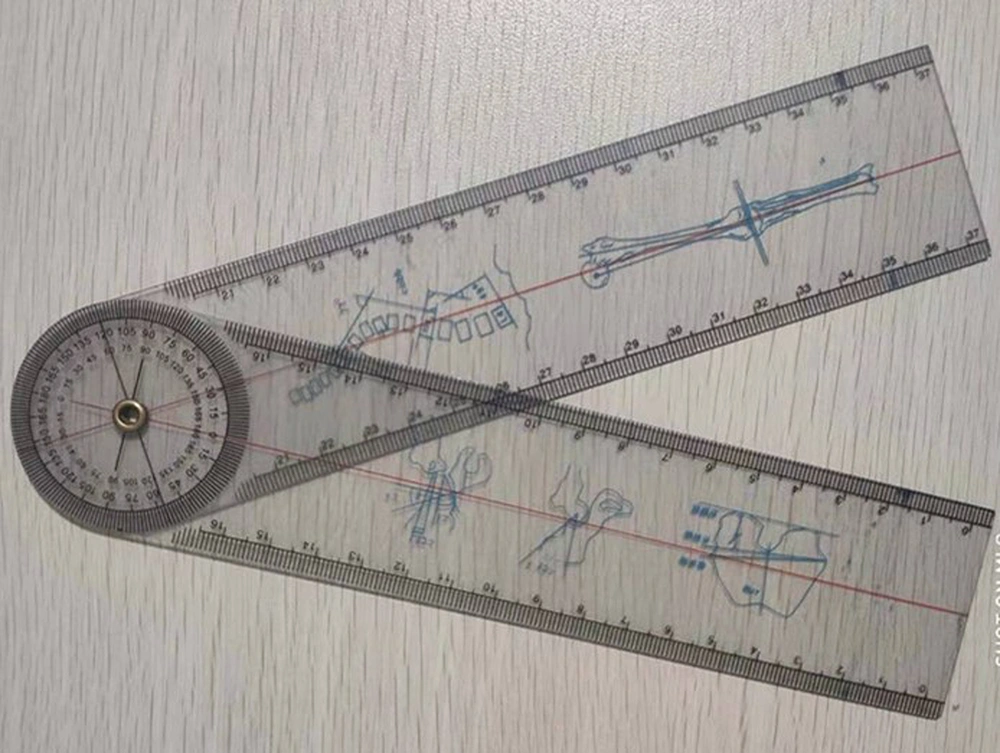
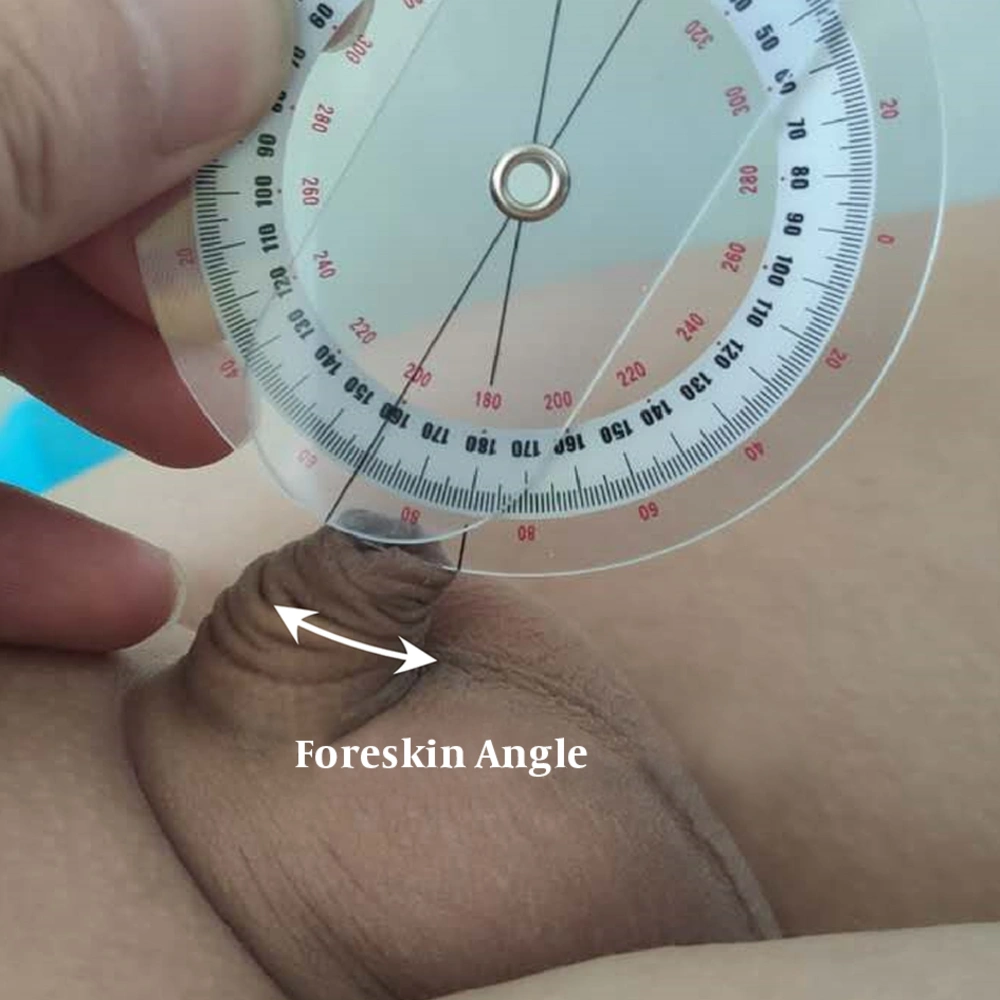
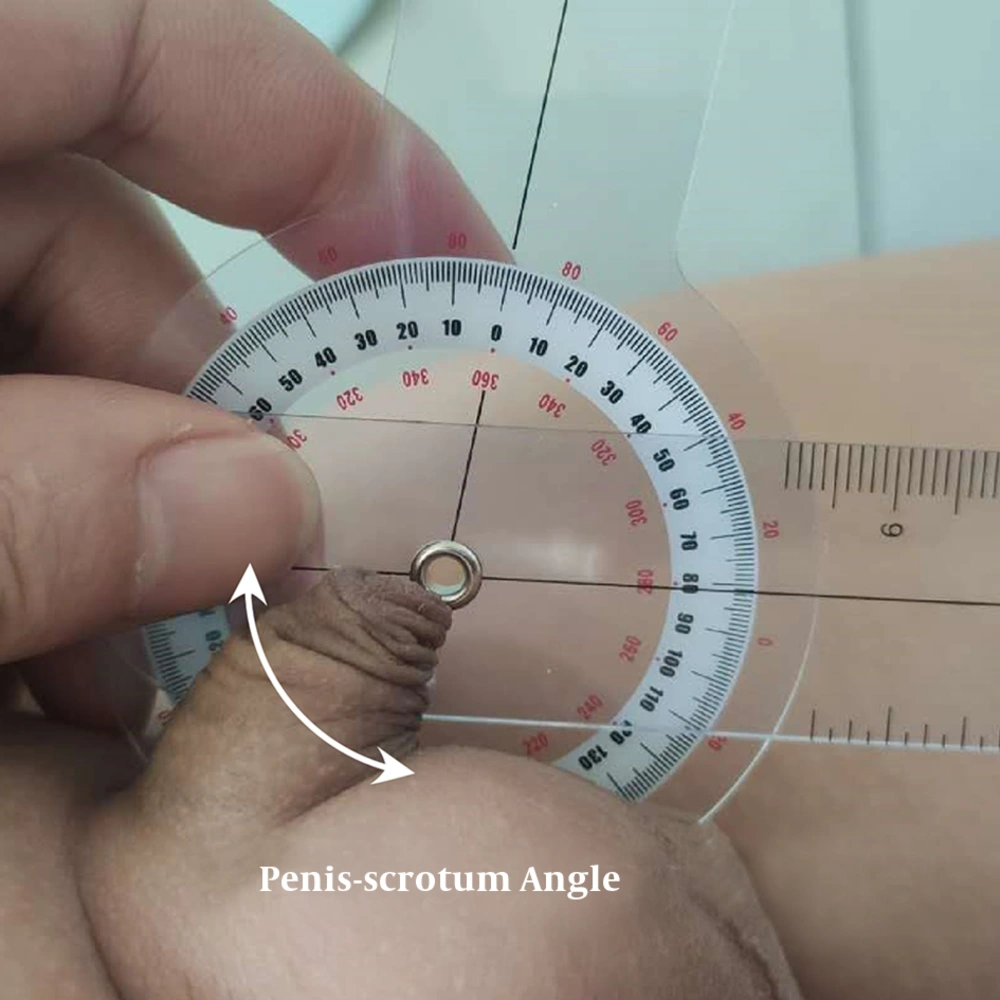
The type of concealed penis was independently diagnosed by two physicians, and the disagreements were resolved by a third physician with more than 10 years of experience. After diagnosis, 105 cases were diagnosed as phimosis, 88 cases as congenital concealed penis, and 78 cases as obesity concealed penis. The foreskin angle, penis-scrotum angle, and number of annular wrinkles of foreskin surface of all 271 participants were independently measured by two professional technicians of our hospital. Foreskin angle and penis-scrotum angle were measured using a professional protractor (Brand: CARENT, Figure 1). The inclusion criteria were (1) the child has a concealed penis, and the type of concealed penis was diagnosed as phimosis or congenital concealed penis or obesity concealed penis; (2) children under 13 years old; (3) the penis has no other serious deformities or penile-related diseases. The exclusion criteria were (1) the penis of the child has serious deformities or penile-related disease; (2) parents or legal guardians refused to participate in this study or did not obtain a signed informed consent. The foreskin angle was defined as the angle between the ventral and dorsal sides of the penis body and the line extending to the foreskin, which was the sagittal position of the natural state of the penis when the child lay down (Figure 2). The penis-scrotum angle was defined as the angle between the ventral side of penis and the scrotum (Figure 3). Except for the natural wrinkles around the outer foreskin, other wrinkles that were more than one-half of the circumference on the surface of the penis body were classified as annular wrinkles (Figure 4). All data were recorded by professional physicians, and differences between different groups were compared using t-test. All analyses were performed by IBM SPSS statistical software version 22 (IBM Corp., Armonk, New York, USA). A two-tailed P value < 0.05 was considered statistically significant.
4. Results
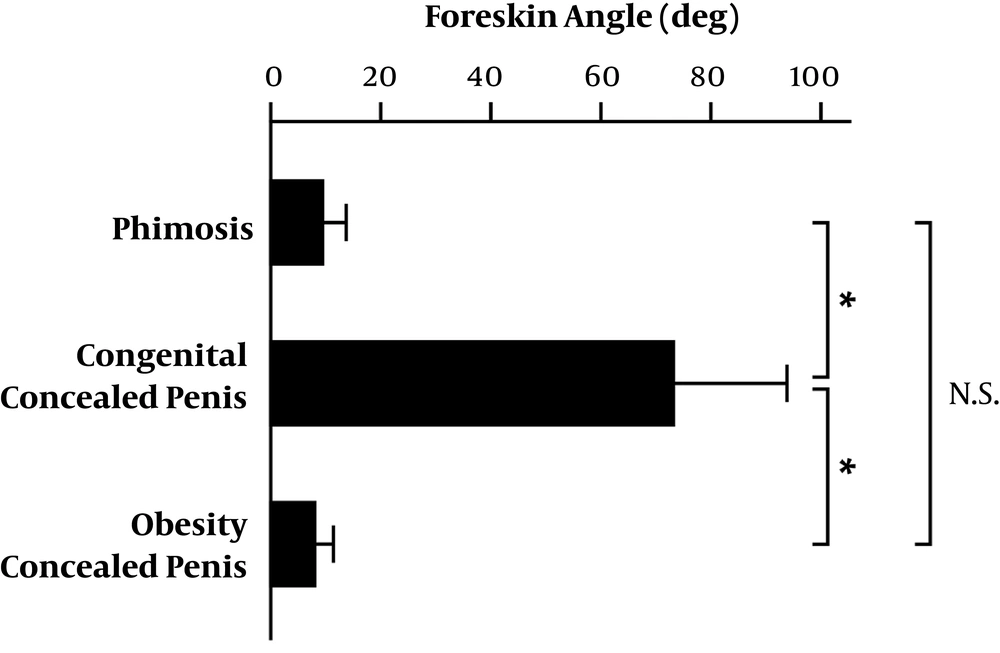
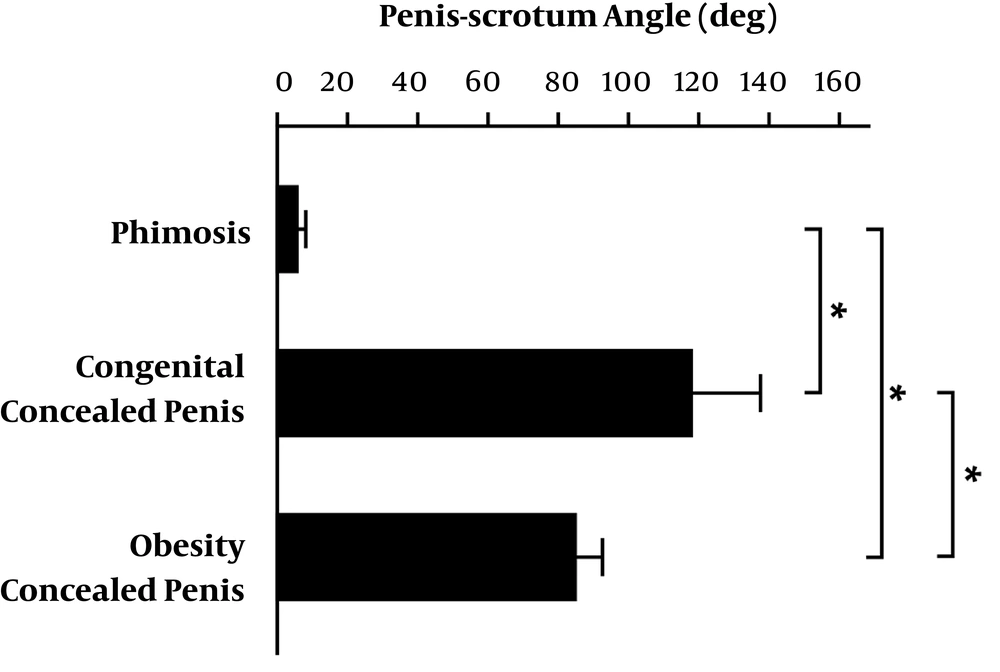
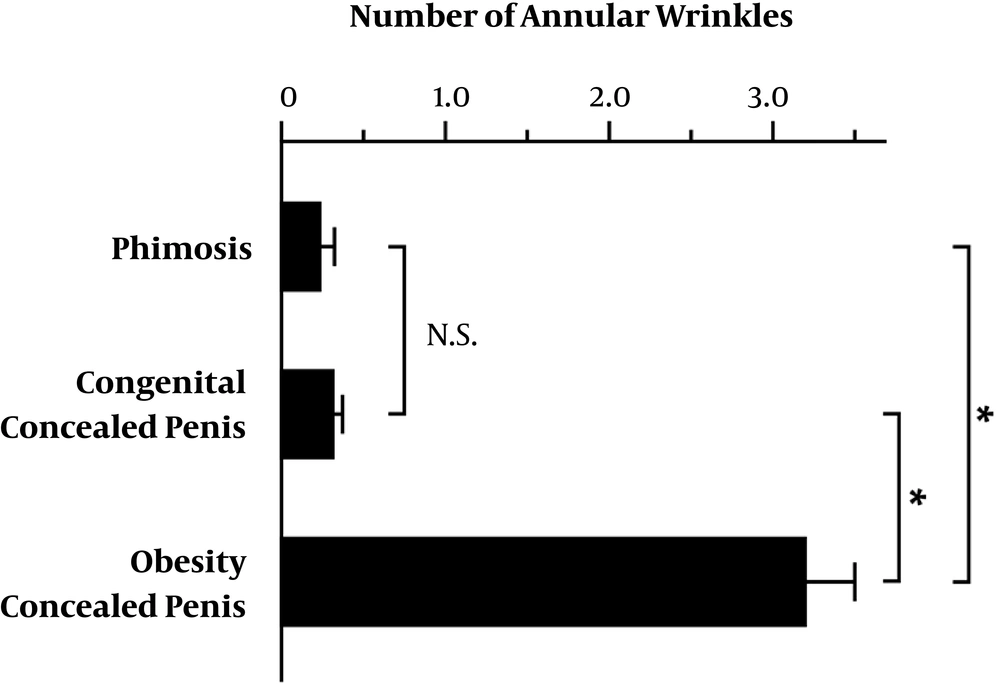
The average of foreskin angle in the phimosis group, congenital concealed penis group and obesity concealed penis group was 10.05° (ranging from 0° to 20°), 74.34° (ranging from 30° to 155°) and 8.86° (ranging from 0° to 20°), respectively (Table 1). The foreskin angle of patients in the congenital concealed penis group was significantly larger than that in the phimosis group and obesity concealed penis group (Figure 5, P < 0.05). However, there was no significant difference in the foreskin angle between the phimosis group and the obesity concealed penis group (Figure 5, P > 0.05). The average of penis-scrotum angle of patients in the phimosis group, congenital concealed penis group and obesity concealed penis group was 6.98° (ranging from 0° to 90°), 118.65° (ranging from 100° to 155°) and 85.59° (ranging from 80° to 100°), respectively (Table 2). The penis-scrotum angle of patients in the congenital concealed penis group was significantly larger than that in the phimosis group and obesity concealed penis group (Figure 6, P < 0.05). In addition, the penis-scrotum angle of patients in the obesity concealed penis group was significantly larger than that in the phimosis group (P < 0.05). Regarding the annular wrinkles on the foreskin surface, the numbers of annular wrinkles of foreskin in the phimosis group, congenital concealed penis group and obesity concealed penis group were 0.26 ± 0.08, 0.32 ± 0.07, and 2.68 ± 0.52, respectively (Table 3). The number of annular wrinkles in the obesity concealed penis group was significantly more than that in the congenital concealed penis group and the phimosis group (Figure 7, P < 0.05).
| Group | Mean | Range |
|---|---|---|
| Phimosis | 10.05° | 0° to 20° |
| Congenital concealed penis | 74.34° | 30° to 155° |
| Obesity concealed penis | 8.86° | 0° to 20° |
| Group | Mean | Range |
|---|---|---|
| Phimosis | 6.98° | 0° To 90° |
| Congenital concealed penis | 118.65° | 100° To 155° |
| Obesity concealed penis | 85.59° | 80° To 100° |
| Group | Mean ± SD |
|---|---|
| Phimosis | 0.26 ± 0.08 |
| Congenital concealed penis | 0.32 ± 0.07 |
| Obesity concealed penis | 2.68 ± 0.52 |
5. Discussion
In clinical practice, experienced physicians can diagnose the type of abnormal penis and provide corresponding treatment through empirical observation. For inexperienced physicians, however, misjudgment may result in unnecessary surgery (obesity concealed penis) or delayed reconstruction of the concealed penis. Thus, in this study, we proposed a simple and auxiliary measurement method to assist in the diagnosis of phimosis, congenital concealed penis and obesity concealed penis in children. The results of this study showed that children with congenital concealed penis had greater foreskin angle (about 74.34°) and penis-scrotum angle (about 118.65°), while children with obesity concealed penis had moderately large penis-scrotum angle (about 85.59°) and higher number of annular wrinkles of foreskin surface (about 2.68). In contrast, children with normal phimosis had the lowest foreskin angle (about 10.05°), penis-scrotum angle (about 6.98°), and number of annular wrinkles (about 0.26). Thus, the auxiliary evaluation system can help clinicians identify the type of concealed penis clinically and provide a basis for subsequent treatment.
The design of this study is based on the beak-like (or pagoda-shaped) or earthworm-like appearance of the concealed penis. Clinically, congenital concealed penis and obesity concealed penis were the most common cause of penile surgery in children. Congenital concealed penis was formed due to inadequate proximal attachments of dysgenetic dartos and appropriate or excessive attachment to the dorsal cavernosum (20, 21). Dartos dysplasia and abnormal fixations hinder the exposure of the penis. During the development of the penis, these constraints gradually extrapolate to form a typical “beak-like” or “pagoda-like” appearance, which leads to abnormal foreskin angle and penis-scrotum angle. On the other hand, excessive fat in a boy who is obese may also contribute to the appearance of obesity concealed penis. Due to the accumulation of fat in children, the penis body is relatively retracted, causing the wrinkled outer skin to look like earthworms. The clinical manifestations are that the penis body is not easy to touch from outside the foreskin, and the annular folds on the surface of the foreskin are obviously deepened and increased. In view of this phenomenon, we added an annular wrinkles index to explore the differential diagnostic assistance of different causes of concealed penis. The final results of this study confirmed that these three indicators can effectively distinguish congenital concealed penis, phimosis and obesity concealed penis in children.
A micropenis is characterized by the smaller penis than normal, which is easily diagnosed by clinician or personnel. If the length of the extended penis is less than 2.5 standard deviations from the normal mean, it can be considered as a micropenis. However, the length of concealed penis is normal, so in addition to the clinical characteristics for judgment, development of other measurement methods are needed. Chin et al also developed an auxiliary way to quantify the severity of buried penis by determining the length of the penile skin (S) and the exact length of penile shaft (P) (4). They demonstrated that only patients with S/P ratio < 70% are considered to be suitable for preputial unfurling. Although it is not mentioned whether S/P ratio can be used as a distinction between congenital concealed penis and obesity concealed penis in children, Chin et al. suggested that diet control or liposuction would be a better way for patient with concealed penis due to obesity. In addition, the S/P ratio method was applied for patients ranging from 2 months to 33 years old. However, our auxiliary measuring method was currently suitable for children below 13 years old, not suitable for teenagers and adults. We believe that the measured angles of the children will change during the development of the penis. It’s worthwhile to conduct more in-depth studies in the future to explore whether these two strategies can be used in combination, and whether our auxiliary methods can be applied to patients of different ages.
There is still considerable controversy about whether children with concealed penis should undergo surgery immediately, especially for concealed penis caused by obesity. Surgical intervention as early as possible can indeed prevent children from having the negative impact on sexual-psychological development due to concealed penis (22, 23). In addition, it can reduce the development of aesthetic concern, balanitis, urinary tract infections, erectile dysfunction, and difficult hygiene. However, many pediatric urologists believe that children with concealed penis due to obesity may temporarily not need surgery. After successful weight loss of obese children, penile growth may accelerate and return to normal in the middle or late childhood. When choosing the appropriate surgical technique for children with concealed penis due to obesity, circumcision or preputial unfurling should not be applied (4). It may cause preputial shortness or absence, which seriously affect penile development.
It should be emphasized that although patients with obesity concealed penis are often associated with obesity, they are not all overweight children. In addition, some children may have two or more different causes of concealed penis or severe forms of concealed penis (22, 24, 25), which may be reflected in the complex values of the foreskin angle, penis-scrotum angle, and the number of annular wrinkles. These measured values in children with multiple syndromes will be significantly higher than that in children with phimosis and between children with congenital concealed penis and obesity concealed penis. In this situation, we suggest that the final clinical treatment decision should be made through stricter examinations or discussions with other more experienced physicians.
5.1. Conclusion
The auxiliary evaluation method combines the foreskin angle, penis-scrotum angle, and numbers of annular wrinkles of foreskin surface to help clinicians in providing a new basis for the diagnostic assistance of concealed penis. For phimosis, the measured values are foreskin angle < 30°, penis-scrotum angle < 80°, and the numbers of annular wrinkles of foreskin surface < 2. For congenital concealed penis, it is foreskin angle > 30°, penis-scrotum angle > 100°, and the numbers of annular wrinkles of foreskin surface < 2. As for obesity concealed penis, it is foreskin angle < 30°, penis-scrotum angle 80° - 100°, and the numbers of annular wrinkles of foreskin surface > 2.