1. Background
Proper sleep pattern is considered as an important effective factor on physical and mental development of adolescents and children (1-4). So, the trend of insufficient and poor quality sleep among adolescents is a public health concern which assessed its relationship with several mental problems such as depression, anxiety, social isolation and attention deficit hyperactivity disorders (ADHD) (5-8) and physical disorders included in hypertension, hyperglycemia and obesity (9) in adolescents.
Depression is the second most common cause of mortality among adolescents because it can lead to suicide (10-12). In other words, sleep disturbance is considered among the top 10 warning signs of suicide in adolescence (13). So, these two important issues can highlight potential importance of assessment of relationship between sleep and depression in this critical period of growing up from childhood into adulthood when social interactions become more complex.
Modifying deteriorated sleep may be protective factor in prevention of mental problems including depression in adolescence (4, 14).
Findings from studies on relationship between sleep and psychological functions in adolescents have shown that adolescents and their parents should be educated about poor sleep and the effects of sleepiness on psychological problems and they must be awarded about some symptoms such as anxiety, depression, and somatic complaints and guidance about monitoring sleepiness (15).
Neurobiological studies declare that sleep deprivation may reduce inhibition of the amygdala area and can affect emotional processing and progression of anxiety, depression and social isolation, gradually (16, 17).
Beside the biological mechanisms, cultural factors such as co-sleeping, bedtime rituals, the sleeping environment and napping, are also important determinants of sleep behaviors in adolescents and influence both the type and frequency of sleep problems (18).
Previous studies have shown that sleep might be a modifiable risk factor in prevention of several mental health problems in adolescence (19, 20).
2. Objectives
Therefore, this study was designed to asses sleep pattern and its relationship with depression. It might be helpful for designing next strong cohort studies for evaluating a causal association between sleep pattern and depression in order to apply helpful information for well-being and physical and mental development interventional programs in adolescents health promotion as an important age group in the future by policy makers.
3. Methods
In 2019 April to August we arranged a cross-sectional survey in 3 levels of high schools (10th, 11th and 12th level) in Hamedan province located in North West part of Iran. Students in consenting schools were in randomly multiple cluster selected classes. Of the 700 students from 20 classes eligible to participate, 567 completed the questionnaire, for a response rate of 82 %. Missing values were removed from calculations and statistical analysis. All 10th, 11th and 12th level high school students studying in Hamadan in 2019 were included and lack of willingness and written consent of containedn the study was considered as exclusion criteria.
We applied a self-reported questionnaire consisting4 parts. The First part of questionnaire contained demographic questions. In the second part we applied PSQI, a standard self-reported valid and reliable (α: 0.83) questionnaire for recording sleep quality (21). All questions could be answered by a 3-level scale (never, sometimes (2 or 3 times in a week), often (more than 3 times in a week)). A standard instruction was used for determining the score of sleep quality in different subscales and severity of sleep disorder.
Beck Depression Inventory questionnaire as a valid and reliable questionnaire was used in the third part for measuring depression. The internal consistency was demonstrated to be 0.9 and the retest reliability ranged from 0.73 to 0.96 (22), educational status was defined based on semester average score: ≥ 17 was considered fine, 14 - 16 moderate and < 14 poor.
Considering the magnitude of the study subject and trust to collaborate honestly in answering the questions, at first, nature and purpose of the questionnaire were explained to students and anonymity was also emphasized. Because of student’s age being under 18, completing the questionnaire needed to obtain informed consent from the parents in addition to informed consent from themselves. Based on the last ethical committee, at the top of every questionnaire a short notice was brought which suggested filling it consulting their parents at home and returning without answer if they didn’t wish to complete it. In the next day all questionnaires were collected in a box which was placed at the middle of the class. They were assured that their personal information would remain wholly confidential. The study was started after approval from institute’s ethical committee (ID: IR.UMSHA.REC.1397.978).
The data were analyzed descriptively and analytically by SPSS 21. The frequency and percentage of responses to each question were calculated. According to the scale of the questionnaire, the total score of each individual was obtained. The normality of data distribution was checked. In order to assess relationship between sleep disorder severity and students’ characteristics, Chi square test was used. Pearson correlation was considered for testing the correlation between sleep disorder and depression score and finally, in order to identify predicting factors for depression in students, logistic regression analysis was used. Variables included sex, educational situation and sleep disturbance, which had a meaningful relationship with depression in simple regression, were entered into the model and after checking the model’s goodness of fit by Hosmer and Lemeshow test, predicting factors were determined. The significance level in all tests was 0.05.
4. Results
This study investigated 576 students in 10th to 12th grade of 1 and 2 educational areas in Hamden province. The mean age of the students was 16.53 ± 0.69years (Min - Max: 15 - 19), of whom290 (50.3%) were girls. 112 (19.4%) students were studying in humanities, 319 (55.4%) in experimental field and rest of them in mathematics. Only 5.8 % (33) were without problem in sleep efficiency. Details about subscales of sleep disorder index are shown in Table 1.
| Sleep Disorder Subscale | Without Problem, No. (%) | Moderate Problem, No. (%) | Serious Problem, No. (%) | Very Serious Problem, No. (%) |
|---|---|---|---|---|
| Mental quality of sleep | 176 (30.5) | 144 (25) | 236 (41) | 20 (3.5) |
| Delay in falling asleep | 156 (27.1) | 233 (40.5) | 160 (27.8) | 27 (4.7) |
| Real time sleep | 259 (45) | 162 (28.1) | 93 (16.1) | 62 (10.8) |
| Sleep efficiency | 33 (5.8) | 30 (5.2) | 108 (18.8) | 405 (70.2) |
| Need to Use of hypnotics(drugs) as a problem | 497 (86.3) | 34 (5.9) | 15 (2.6) | 30 (5.2) |
| Daily dysfunction | 130 (22.6) | 279 (48.4) | 131 (22.7) | 36 (6.2) |
| Sleep disorder | 5 (0.9) | 287 (49.8) | 239 (41.5) | 45 (7.8) |
| Usual bedtime | 21 - 23 PM | 23 and Up To 24 | 24 and Up To 1 AM | 1 AM and After |
| No. (%) | 33 (5.7) | 132 (22.9) | 197 (34.2) | 201 (34.8) |
| Sleep latency | 0 - 15 min | 15 - 30 min | 30 - 60 min | > 60 min |
| No. (%) | 358 (63.4) | 169 (29.3) | 31 (5.3) | 7 (1.2) |
| Sleep duration | 7h and more | 6 - 7h | 5 - 6h | < 5h |
| No. (%) | 243 (42.1) | 173 (30) | 92 (15.9) | 60 (10.4) |
Based on the results, 497 (86.3%) participants didn’t report any use of hypnotics but 5.9%, 2.6% and 5.2% of them used it one time, two times and three or more times in a week, respectively.
Results for association between sleep disorder severity and students characteristics showed that 12.9% of the boys and only 2.8% of the girls had severe problem of sleep disorder (P < 0.001). In students with good educational status (Semester grade point average ≥ 17) 56.6% hadn’t any sleep disorder or they showed mild problems whereas 43.9% of students with moderate educational status and 40.7% of poor educational status showed moderate problems of sleep disorder (P < 0.05). So, in girls and students with proper educational status, sleep disorders were less than others. However, there wasn’t any relationship between sleep disorder severity and field of study (P = 0.157). Details are shown in Table 2.
| Students’ Characteristics | Sleep Disorder, No. (%) | P Value | ||
|---|---|---|---|---|
| Without Problem or Mild | Moderate Problem | Severe Problem | ||
| Sex | < 0.001 | |||
| Male | 124 (43.4) | 125 (43.7) | 37 (12.9) | |
| Female | 168 (57.9) | 114 (39.3) | 8 (2.8) | |
| Educational status (Semester average score) | 0.029 | |||
| 17 or more (good) | 180 (56.5) | 115 (36.1) | 24 (7.5) | |
| 14 - 17 (moderate) | 101 (43.9) | 108 (47) | 21 (9.1) | |
| < 14 (poor) | 11 (40.7) | 16 (59.3) | 0 (0) | |
| Field of study | 0.157 | |||
| Humanities | 66 (58.9) | 36 (32.1) | 10 (8.9) | |
| Experimental field | 159 (49.8) | 133 (41.7) | 27 (8.5) | |
| Mathematics | 67 (46.2) | 70 (48.3) | 8 (5.5) | |
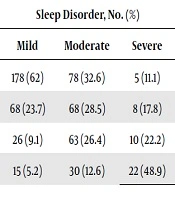
It was notable that among all students only 5 persons (0.9%) were considered normal in terms of mood and without any problem in sleep. So, rest of them endured some degree of depression or sleep disturbance and sleep disorder was significantly higher in severely depressed students (P < 0.001) (Table 3).
| Depression Severity | Sleep Disorder, No. (%) | P Value | ||
|---|---|---|---|---|
| Mild | Moderate | Severe | ||
| Without depression, No. (%) = 226 (46.2) | 178 (62) | 78 (32.6) | 5 (11.1) | < 0.001 |
| Mild depression, No. (%) = 144 (25) | 68 (23.7) | 68 (28.5) | 8 (17.8) | |
| Moderate depression, No. (%) = 99 (17.2) | 26 (9.1) | 63 (26.4) | 10 (22.2) | |
| Severe depression, No. (%) = 67 (11.6) | 15 (5.2) | 30 (12.6) | 22 (48.9) | |
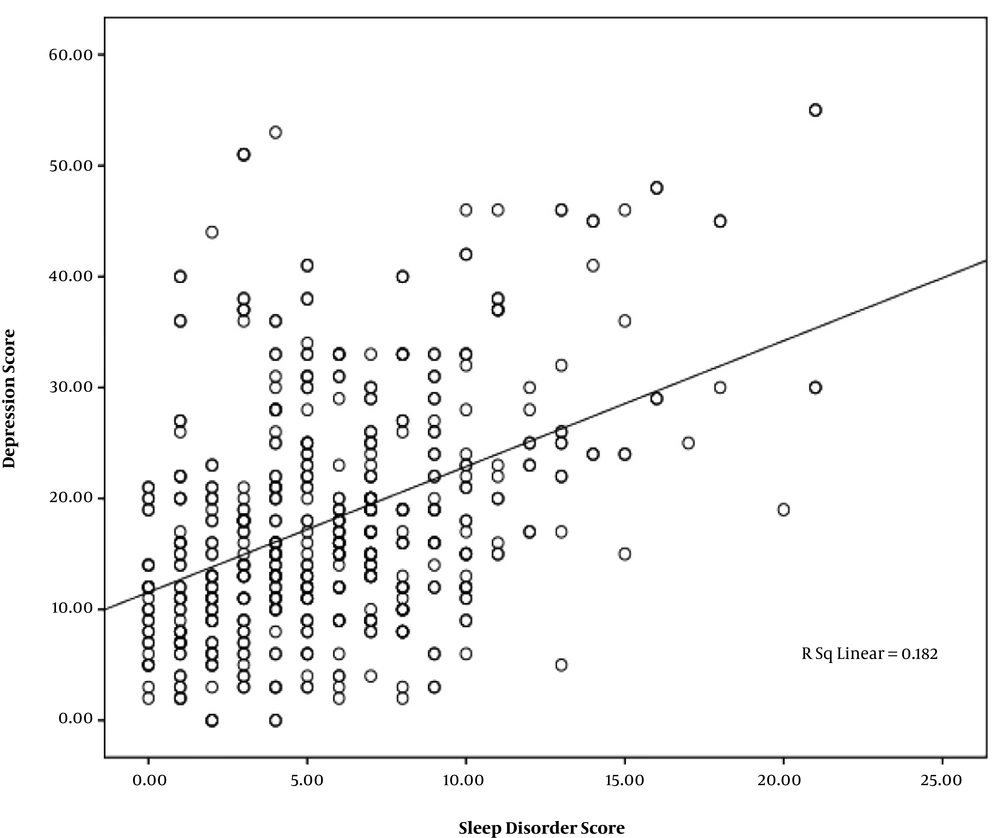
Additionally, there was a statically significant correlation between sleep disorder and depression score (Pearson correlation: r = 0.42; P < 0.001) which is shown in Figure 1.
In logistic regression analysis for detecting depression’s predicting factors, being boy and having severe problem in sleep pattern of the students were considered as statistically related variables to depression (Table 4).
| Variables | OR | Lower | Upper | P Value |
|---|---|---|---|---|
| Sex | ||||
| Male | 1.5 | 1.04 | 2.3 | 0.03 |
| Female | Referent | |||
| Sleep disorder | ||||
| Normal | Referent | |||
| Moderate | 1.7 | 0.7 | 4.2 | 0.2 |
| Severe | 18 | 5.1 | 63 | < 0.001 |
aHosmer and Lemeshow test: Chi square (6) = 3.6, P value = 0.7; A total of 68.6% of subjects were correctly classified
5. Discussion
Considering the importance of sleep disorder and its effect on mental and physical health in adolescents, this study which was designed on almost 600 Iranian adolescents to asses sleep pattern and its relationship with depression. The study revealed that nearly 70% of the adolescents had problems in mental quality of sleep, delay in falling asleep and daily dysfunction. In 10%, sleep duration was less than 5 hours and in 69% usual bedtime was after midnight (24 o’clock).
Poor sleep quality has been reported in different studies from nearly half of the students (2, 23, 24) to more than 80% in other studies (25). In our findings less than half of the students (42%) had normal sleep duration (≥ 7 h) based on recommended need for adolescents (26) which was less than other findings in similar previous studies (24, 27, 28).
It seems that these poor sleep quality and quantity indicators contribute to a huge stress for passing a contest examination for entering the university (the so-called Concours) especially in 10th to 12th high school students in Iran. The manner of setting and running this exam is associated with high stress imposed on students which is worth that educational officials and managers think about changing the method of students’ evaluation for entering the university, in order to provide healthy sleep and mental health in adolescents.
Poor sleep can increase some physically problems such as blood pressure and type 2 diabetes risk in youth (9) beside psychological complications including depression, anxiety, ADHD and even suicide (5, 6, 17, 29).
The present study revealed that severe sleep problems in boys were more conspicuous than in girls and more than half of students with good educational status didn’t have sleep problem. However, there wasn’t any relationship between sleep disorder severity and field of study. In a systematic review, female gender, depressed mood, and physical illness were considered as risks for future sleep disturbances (30). The other point that was assessed in this project was amount of using electronic devices and screens which was higher in boys in comparison with girls and using those devices showed statically significant relationship with sleep problems, as well. It might be considered as a reason for having more sleep problems in boys than in girls. Details about using electronic devices and screens will be brought in a forthcoming article.
Several psychosocial factors may affect sleep pattern and are related to the delay in bedtime and reducing the sleep duration in adolescents (31). Our findings showed statically significant correlation between sleep disorder and depression score. Association between poor sleep quality and depressive symptoms has been observed in some former studies (5, 7, 17, 29).
Several pathways have been recommended for chains of relationship between poorer sleep quality and higher depressive symptoms (32, 33). Additionally, it has been explained that elevated anxiety is related to in appropriate concentrations of serotonin and dopamine in the brain (34), and those neurotransmitters have been related with sleep quality and decreased REM sleep time (35)and depressive symptoms (36).
This study revealed that nearly 70% of Iranian students had problems in mental quality of sleep, more than half of them had normal sleep duration and almost half of them had some degrees of depression symptoms. Being boy and having severe problem in sleep pattern were considered as statistically related variables for predicting depression. Of course, this was a cross -sectional study, so that we couldn’t get evidential results indicating that defect in sleep pattern can cause depression, cohort studies are needed for detecting causality. However, adolescent health providers should consider how these difficulties may potentially worsen each other. So, adolescents with sleep problems should be screened for comorbid mental problems, particularly depression or even suicide and self-harm behavior. These information might be applied for well-being and physical and mental development interventional programs in adolescents’ health promotion as an important age group in the future by policy makers.
5.1. Limitations
Our study has limitations which need to be considered in the future researches. Firstly, this is a cross-sectional study, so we cannot demonstrate causality in our interpretation; secondly, our sample was limited to adolescents in a particular population (10th to 12th high school students), so, results may not be generalized to all adolescents; thirdly, some more accurate results would be found if one-week sleep diary of the participants had been detected; fourthly the percentage for sleep problems underestimated (13.7% in the worst situation) suggestive of hypnotics use, these cases were not separated in our analysis. It is recommended that other psychological problems such as stress, anxiety, suicide, etc. beside interventional programs for reducing the sleep problems be assessed in the future research and in adolescents health care packages.
5.2. Conclusion
Problems in mental quality of sleep were notable in Iranian adolescents and almost half of them had some degree of depression symptoms. Being boy and having severe problem in sleep pattern were predictors for depression. These findings might be applied to interventional programs for well-being and physical and mental development of adolescents, as well as parents’ educational programs for adolescents’ health promotion.