1. Background
The main goals of anesthesia for pediatric outpatient surgery are rapid emergence, short recovery with low postoperative side effects, and rapid discharge (1). Inhalation anesthesia has been the basis of pediatric anesthesia for more than 150 years due to its efficacy, reliability, safety, stability, ease of delivery, and not having end-organ consequences (2). The majority of pediatric anesthetists worldwide are considering it as the gold standard (3). Meanwhile, with the advances in understanding the pharmacological properties and availability of fast-acting drugs, total intravenous anesthesia (TIVA) has become an appealing option in general anesthesia in children (4-6). Therefore, utilization of TIVA compared to volatile anesthesia is still a topic of debate in successful anesthesia management.
2. Objectives
The current study aimed to compare inhalation anesthesia with sevoflurane and total intravenous anesthesia (TIVA) with propofol infusion on the quality of recovery. Secondary measures included postoperative pain, postoperative nausea and vomiting, hemodynamic status, and duration of post-anesthesia care unit (PACU) stay.
3. Methods
The study was conducted from March 2019 to August 2019 at Tabriz Pediatric Hospital. 80 cases aged 2 - 10 years who were scheduled to undergoing herniotomy, orchiopexy, frenulectomy, and sigmoidoscopy surgery were included. Exclusion criteria included having a known allergy to any of the drugs involved in the study, being on an anticonvulsant, having purulent nasal discharge, fever, and history of malignant hyperthermia, cardiopulmonary disease, or other organic dysfunction. Patients were allowed to take solid food until 8 hours, milk products until 6 hours, and clear liquids until 3 hours before the surgery. The participating patients were randomly assigned to one of the two groups of TIVA with propofol (T) or sevoflurane (S) anesthesia using a computer-generated random number table. Routine investigations were performed in the operation room. Non-invasive monitors, such as electrocardiogram, blood pressure, oxygen saturation, and bispectral index (BIS) were attached for recording baseline parameters. To have an adequate depth of anesthesia, the BIS value was regulated between 40 and 60. The TIVA group with propofol (T) anesthesia induced with midazolam 0.03 - 0.05 mg/kg, fentanyl 1mcg/kg, propofol 3 - 5 mg/kg, 0.1 mg/kg lidocaine, and an appropriate size of laryngeal mask airway (LMA) was implanted, and the anesthesia continued with propofol infusion 100 to 250 μg/kg/min and remifantanil 0.1 mcg/kg. The concentration of remifentanil was modified in accordance with the BIS. The sevoflurane (S) group received general anesthesia induced with midazolam 0.03 - 0.05 mg/kg, fentanyl 1mcg/kg, O2/sevoflurane 8 vol%, maintenance with 2 - 3vol%. The concentration of sevoflurane was modified in accordance with the BIS, heart rate, and blood pressure. After successful extubation, children were transferred to the PACU. Demographic characteristics, awakening quality in recovery, agitation, and other complications such as pain, nausea, vomiting, and hemodynamic status were documented by an experienced nurse. Postoperative pain was equal in the two groups and was measured 15 minutes after surgery using the Wong-Baker Faces Pain Rating Scale and pain relief was provided by rectal acetaminophen. Collected data were evaluated using statistical-descriptive methods (i.e., mean, standard deviation, frequency, and percentage). The independent-samples t-test was used to compare quantitative data. The non-normal distribution of data was assessed by the Kolmogorov-Smirnov test and Chi-Square test. Data were analyzed by SPSS version 20. A P-Value of < 0.05 was considered as statistically significant.
4. Results
Of 95 children to be evaluated, 15 were excluded. The remaining 80 patients were randomly allocated to the two defined groups. 40 children were planned to receive sevoflurane, and 40 children were planned to receive propofol and remifentanil. The characteristics of patients are presented in Table 1. Patients in the two groups were not significantly different in terms of gender, American Society of Anesthesiologists (ASA) class, and body weight. Anesthesia and surgery time were similar in both groups (Table 1). There were significant differences concerning the eye-opening time (14 and 22 minutes) and the time of staying in recovery (25 and 35 minutes), respectively, between the sevoflurane and TIVA groups (P < 0.001) (Table 2).
| (T) Group, (n = 40) | (S) Group, (n = 40) | P-Value | |
|---|---|---|---|
| Age (y) | 6 ± 1 | 5 ± 2 | 0.537 |
| Gender (M/F) | 30/10 | 30/10 | 1.00 |
| Weight (kg) | 18.2 ± 4 | 15.6 ± 5 | 0.077 |
| ASA (I/II) | 40/0 | 37/3 | 0.98 |
| Duration of anesthesia (min) | 48 ± 10 | 46 ± 9 | 0.329 |
| Duration of surgery (min) | 36 ± 8 | 34 ± 9 | 0.209 |
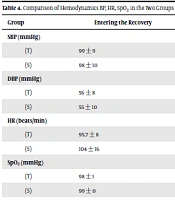
The incidence of postoperative agitation was higher in the sevoflurane group (62%) than the TIVA group (5%) (P < 0.001), and 30 and 17.5% of the patients had postoperative nausea and vomiting in TIVA and sevoflurane groups, respectively (Table 3). In this study, the highest percentage of pain was found in the sevoflurane group, 52.5% of the children were anesthetized with sevoflurane experienced pain compared to 25.0% of the children who were anesthetized with TIVA (Table 3). Investigating hemodynamic variables (Table 4) revealed no difference in systolic pressure, diastolic pressure, and arterial oxygen saturation during the recovery between the two groups. But there was a significant decrease in the heart rate of the patients in the T group (P < 0.001).
| Adverse events | Group (T), (n = 40) | Group (S), (n = 40) | P-Value |
|---|---|---|---|
| Agitation (% within) | 2/40 (5.0) | 25/40 (62.5) | < 0.001a |
| Nausea or vomiting (% within) | 12/40 (30.0) | 7/40 (17.5) | 1.00 |
| Pain % (Score 4 - 8) | 25.0% | 52.5% | 0.05 |
aP < 0.05 versus Group (T) and Group (S).
| Group | Entering the Recovery | 5 Min | 10 Min | 20 Min | Before Discharge | P-Value |
|---|---|---|---|---|---|---|
| SBP (mmHg) | 0.132 | |||||
| (T) | 99 ± 9 | 100 ± 9 | 102 ± 11 | 105 ± 9 | 107 ± 10 | |
| (S) | 98 ± 10 | 102 ± 12 | 103 ± 12 | 100 ± 12 | 108 ± 12 | |
| DBP (mmHg) | 0.366 | |||||
| (T) | 56 ± 8 | 57 ± 8 | 59 ± 24 | 62 ± 9 | 63 ± 9 | |
| (S) | 55 ± 10 | 60 ± 13 | 62 ± 18 | 61 ± 9 | 59 ± 8 | |
| HR (beats/min) | < 0.01b | |||||
| (T) | 95.7 ± 8 | 97 ± 6 | 98 ± 7 | 100 ± 7 | 104 ± 7 | |
| (S) | 104 ± 16 | 105 ± 11 | 104 ± 7 | 104 ± 10 | 109 ± 9 | |
| SpO2 (mmHg) | 0.832 | |||||
| (T) | 98 ± 1 | 98 ± 1 | 99 ± 1 | 98 ± 0 | 98 ± 1 | |
| (S) | 99 ± 0 | 98 ± 1 | 98 ± 1 | 98 ± 1 | 99 ± 0 |
aValues are expressed as mean ± SD.
bP < 0.05 versus Group (T) and Group (S).
5. Discussion
Inhalation anesthesia using the sevoflurane and TIVA with propofol are two techniques that are widely used to maintain anesthesia in pediatric patients undergoing general anesthesia for outpatient surgery. However, discussions about the best anesthesia technique for children still continue among anesthetists. The results of this study showed significant differences in eye-opening time (14 and 22 minutes) and the time of staying in the recovery room (25 and 35 minutes), respectively, between sevoflurane and TIVA groups (P < 0.001). Time to eye-opening and recovery stay was significantly shorter in the sevoflurane group than the TIVA. McFarlan et al. (1999) argued that recovery after brief anesthesia with TIVA may be as fast as when using inhalation anesthesia. Besides, recovery after prolonged anesthesia with TIVA is likely to be much protracted than after inhalation anesthesia (7). These findings aren’t in line with our study. Also, Steur et al showed that prolongation in the duration of stay in the PACU in propofol recipients is due to its oversedation, resulting in slower discharge, which is not conducive to outpatient surgery centers (8). In this study, postoperative pain was measured by the Wong-Baker Faces Pain Rating Scale. Patients receiving sevoflurane had a higher percentage of postoperative pain than patients receiving TIVA. Many studies have suggested that propofol-based anesthesia reduces postoperative pain (9-11). Hasani et al. (2013) reported that 24.3% of children anesthetized with sevoflurane experienced pain, compared to 4.5% of children anesthetized with propofol (6). Chandler et al. (2013) also found higher pain scores after administration of sevoflurane, compared to propofol, in children aged between 2 and 6 years who underwent strabismus surgery and concluded that TIVA can reduce the pain scores (9). In the current study, postoperative nausea and vomiting were higher in the TIVA group but were not significantly different. Some studies have reported a higher incidence of nausea and vomiting after sevoflurane anesthesia compared to propofol anesthesia (8, 9, 12). The studies conducted by Picard et al. (2000) investigated the quality of recovery after administration of sevoflurane anesthesia, compared to propofol anesthesia for tonsillectomy in children and did not find any difference concerning the postoperative nausea and vomiting (PONV) between the two groups (1), which is consistent with the findings of the current study. Studies have also shown that propofol may have anti-inflammatory activities, even at very low doses, and is mainly effective in preventing vomiting early after the operation (13-15). Pieters et al. (2010) reported an incidence of 5.4% for the PONV among those who received propofol anesthesia compared to sevoflurane anesthesia (36.8%). Only 1 (out of 200) patients included in this study received anti-nausea in the PACU (10). The study also showed that agitation was more common in children who received sevoflurane anesthesia than in children who underwent TIVA anesthesia. Naito et al. (16) compared agitation after anesthesia with sevoflurane and halothane in children and explained the high incidence of agitation and fidget in children anesthetized with sevoflurane. Also, in one study, the most common causes of agitation are reported, including hypoxemia (decreased tissue oxygen), pain, anxiety, hypoglycemia, hyponatremia (decreased blood sodium), and residual drug effects (17). Another study has considered postoperative agitation as an abnormal and scary behavior (18). Postoperative agitation is commonly performing for preschool children after receiving inhalation anesthetic agents such as sevoflurane (19), desflurane (20), and isoflurane (21, 22). In the present study, hemodynamic parameters were evaluated, and no difference in systolic pressure, diastolic pressure, and arterial oxygen saturation was observed, but heart rate was significantly decreased in the T group (P = 0.01). Previous studies have reported decreased HR in the TIVA group (23, 24) and it has been argued that this is partly due to the stronger inhibition of the neuroendocrine stress response by the TIVA (25). Studies have also shown that sevoflurane has a more outstanding parasympatholytic effect than TIVA (26, 27).
5.1. Conclusion
Inhalation anesthesia with sevoflurane led to more rapid recovery from anesthesia, and TIVA with propofol injection reduced post-operative pain and agitation compared to patients receiving sevoflurane. Therefore, TIVA with propofol infusion is probably an effective technique to maintain general anesthesia in pediatric outpatient surgery and to increase parental satisfaction, and to reduce the workload of recovery room staff.