1. Background
One of the critical criteria for discharging preterm infants from the neonatal intensive care unit (NICU) is an achievement of full oral feeding (1). Oral feeding is a complicated procedure, which needs coordinating sucking, swallowing, and breathing. In preterm infants, the lack of coordination sucking, swallowing, and breathing, the immaturity of their neurological, cardio-respiratory, and gastrointestinal functions leads to delayed oral feeding and prolonged tube feeding (2, 3). Therefore, the preterm infants must reach maturity for success in oral feeding procedure. Furthermore, they need to be cared for by an expert caregiver to help the infants attain a delightful experience of feeding with the most intake and the least stress (4, 5). Preterm infant’s problems in the transition from tube to full oral feeding often result in delayed discharge from hospital. Moreover, increased length of stay in the hospital has adverse effects, such as increased health care costs and also stress on the mother, infant, and family. Ultimately these problems may cause reduced parent-infant interaction (6, 7).
Different interventions have been developed for full oral feeding achievement, including Fucile oral-motor intervention protocol (8), non-nutritive sucking approach (9), and chin support approaches (10), which emphasize only sensory-motor stimulation. Another intervention is Supporting Oral Feeding in Fragile Infants (SOFFI) approach with a goal for the attainment of oral feeding with bottle feeding (11, 12). The scheduled feeding approach is another standard method that is clinician-centered and based on an infant’s weight and gestational age (GA). In this model of care, successful feeding is defined as infant feeding only based on the determined volume by a clinician at a specific time, without attention to the overall state of the infant (13). Another approach used in NICUs in some countries that seems more comprehensive than other approaches and involves all domains of feeding is “cue-based feeding.” In the cue-based feeding protocol, the infant’s behavioral cues are feeding readiness determinant. Moreover, successful feeding is primarily based on the quality of the feeding rather than the quantity. In this approach, successful feeding occurs when it is safe, functional, nurturing, individual, and appropriate for each infant’s level of development (14, 15).
Although some studies have reported that infants fed with cue-based feeding approach have achieved full oral feeding earlier and the length of hospitalization has been shorter than the scheduled feeding approach (1, 4, 15-19), none of the studies have assessed results by a comprehensive feeding assessment scale. A meta-analysis has demonstrated that these findings should be analysed tentatively due to methodological weaknesses in the included trials (19). Moreover, another research illustrated that scant researches were performed to support the use of cue-based feeding (18). In the present study, comprehensive evaluation tools, including Preterm Infant Oral Feeding Readiness Assessment Scale (PIOFRAS) and Early Feeding Skill (EFS) scale have been used to measure the results of the research precisely
Thus, it would be helpful to intervene with consistent evidence that provides useful clinical guidelines for speech-language pathologists, parents, nurses, and physicians to lead to the progress of oral feeding, decrease the length of hospitalization and reduce costs to the family and government. Despite the importance of these issues, there has been no research on the effect of cue-based feeding on preterm infants concerning feeding culture in intensive care units of Iran.
2. Objectives
The aim of the present research is the investigation of the effectiveness of cue-based feeding in comparison with scheduled feeding in preterm infants using feeding assessment scales in the NICU.
3. Methods
3.1. Study Design and Setting
This study was a randomized, clinical trial study designed to investigate the effectiveness of cue-based feeding in preterm infants ≤ 34 gestational age (GA) who had been hospitalized in the Neonatal Intensive Care Unit of Dr. Shariati Hospital, Tehran University of Medical Sciences between Dec. 2017 and Feb. 2018. Inclusion criteria consisted of infants who lacked the ability of oral feeding, neurological, gastrointestinal disorders, significant congenital anomalies. In addition, the Apgar score was 3 or more in the first minute and 5 or more in the first five minutes, and infants who recieved respiratory support with low set-up on continuous positive airway pressure (CAPA) (PEEP ≤ 6 and FiO2 ≤ 30%). Exclusion criteria included the following: some conditions such as family’s unwillingness to participate in the study, infant’s death or transition to another hospital, infant’s discharge before the end of the intervention, and a sudden change affecting neonates’ nutritional status, like cerebral hemorrhage or intestinal problems.
The sample size was calculated using Altman Nomogram and considering type I error of α = 0.05, power = 0.8, and the standard difference 1.2 (20, 21). Thus, the sample size determinded 40 infants (20 infants in each group). Due to attrition of three infants (2 infants were discharged before the end of the intervention in the cue-based feeding group and one infant was excluded from the scheduled group feeding owing to changing hospital), cue-based feeding group and scheduled group feeding consisted of 18 and 19 infants, respectively. Preterm infants were selected for each group by the block randomization method (22). In this method, two groups (Scheduled Feeding and Cue-based Feeding) were in equal sample sizes. Ten blocks were determined, and the block size was 4, and in all blocks, the numbers of infants of two groups were similar (each group consisted of 2 infants in a block).
3.1.1. Outcome Measures
Infant characteristics that included GA (day), gender, weight (grams per day), milk volume, duration of full oral feeding achievement, duration of hospitalization, postmenstrual age (PMA) of first oral feeding day, PMA of full oral feeding day, and PMA of the day of discharge were documented in a questionnaire.
The assessment of the infant’s oral feeding readiness, with the Preterm Infant Oral Feeding Readiness Assessment Scale (PIOFRAS), was performed 15 minutes before the estimated time of the first oral feeding. The assessed aspects consisted of the state of behavioral organization, oral posture, oral reflexes, nonnutritive sucking, and the corrected age of preterm infants. Each of the items on this scale was scored in the range of 0 to 2. Infant’s oral skill performance is considered as the sum of the scores obtained of whole items considered, which ranged from 0 to 36. Validity and reliability of this scale were confirmed in 2007, 2013, and the inter-rater and intra-rater reliability of the Persian version of PIOFRAS was good (Intraclass Correlation Coefficients greater than 0.75 (23-25).
Early feeding skills measure was carried out through the Early Feeding Skill (EFS) scale. It is a 28-item scale that measures feeding skills in three parts, including before feeding (oral feeding readiness assessment), during feeding (ability of maintaining engagement in feeding, ability of oral-motor skills organization, ability of swallowing coordination, and ability of physiological stability maintenance), and after feeding (oral feeding recovery assessment). Subscales of the assessment scale indicate areas of strength, areas of some clinical concern, and areas of major clinical concern. The EFS scale was developed by neonatal nurses and feeding experts and supports content validity. It is reported that the inter-rater reliability of EFS is 0.85 and intra-rater reliability was 0.81 in 2018 (26, 27). Face validity, content validity, structural validity, and internal consistency of the Persian version of EFS are confirmed (26-28).
3.2. Interventions
All subjects - preterm infants - were randomly divided, based on criteria for inclusion, into two intervention groups: cue-based feeding and scheduled feeding protocol. This research consists of 4 evaluation stages: before treatment, first oral feeding day, full oral feeding day, and day of discharge from hospital. A speech and language pathologist in every stage assessed infants by PIOFRAS and EFS
3.2.1. Cue-based Feeding Protocol
Initially, preterm infants were evaluated 15 minutes before feeding by PIOFRAS. If they received a score of more than 30, they would be prepared for oral feeding, and then EFS was used to get the infant’s profile of early feeding skills. When infants did not receive mechanical ventilation, and they could stand full enteral feeding, physicians ordered an assessment of infants’ readiness for oral feeding. During the day, speech and language pathologist reviewed infants’ scores on the Oral Feeding Readiness Scale (OFRS), which had five options that included preterm infants’ oral feeding cues (infant state, rooting behavior, muscle tone, and physiological instability). Feeding readiness was in the range of 1 to 5. One score was indicator of drowsy or alert state, rooting behavior, and the right tone. The score five meant the infant's physiological condition was not stable, and the infant did not have readiness for feeding. Infants were offered oral feedings when their readiness scores were 1 or 2 on the OFRS, and then SLP continuously was evaluating the quality of preterm infants’ oral feeding on the Oral Feeding Quality Scale, which considered infant's sucking, coordination between sucking, swallowing, and breathing, and duration of feeding. The scale consisted of five items that ranged between 1 to 5. The score 1 and 2 demonstrated oral feeding quality was satisfactory and infant was able to feed all milk volume by bottle or breast. The score 5 meant infants were not capable of oral feeding. Oral feeding was stopped if the infant demonstrated distress cues, such as change of heart rate, respiratory rate, and oxygen saturation levels, and uncoordinated suck–swallow–breathe pattern (1, 29, 30). Each oral feeding lasted up to and no more than 30 minutes. The remaining volume of milk was given to the infant by gavage. Infants kept the cue-based feeding up until they orally reached the prescribed volume in each feeding. However, the infant who received a score of less than 30 in PIOFRAS, that infant was not ready for oral feeding. According to the infant’s oral skills, interventions such as oral non-nutritive sucking and skin to skin contact were done before tube feeding (29, 31).
3.2.2. Scheduled Feeding Approach
Initially, preterm infants were evaluated by PIOFRAS for entering the scheduled feeding group. If they had received a score of less than 30, they were enlisted in the scheduled feeding group, and then infants were fed based on a scheduled time (every 3 hours) regardless of infant’s status from the day of inclusion to research to the day of discharge. Whenever the neonatologist determined to start time of oral feeding regarding infant's gestational age and weight, a speech therapist assessed infants’ oral feeding skills by PIOFRAS. The infants who had received a score of more or less than 30, EFS was used to get the infants’ profile of early feeding skills (EFS). After first oral feeding, infants were fed every 3 hours, same before first oral feeding of preterms. If infants had slept, they were awakened to be fed. In this group, successful feeding was measured by volume consumed regardless of infant behaviors (13, 19). When neonatologist determined the day of the full oral feeding and the day of discharge, the speech therapist evaluated again infants’ oral and feeding skills by PIOFRAS and EFS.
3.3. Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 23. To test homogeneity of gender and type of milk was used Chi-Square test, and Shapiro–Wilk test to normalize the distribution of variables. Independent t-test was used for all variables to analyze differences between two groups, with the exception of PMA, and for milk volume the Mann Whitney test was used. Moreover, Bootstrap method was utilized to report confidence intervals of all variables. A P-value of less than 0.05 was considered statistically significant.
4. Results
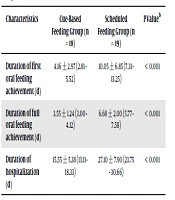
The demographic and clinical characteristics of infants are illustrated in Table 1. The sample consisted of 37 preterm infants, 18 infants in the cue-based feeding group, and 19 infants in the scheduled feeding group. In the total sample, GA at birth ranged from 29 to 34 weeks, and 17 of infants were girls, and 20 infants were boys. Table 2 shows a significant difference in the duration of first oral feeding achievement, duration of full oral feeding achievement, and duration of hospitalization between two groups (P < 0.001). The cue-based feeding group achieved full oral feeding on average 3.13 days sooner (3.55 ± 1.24 vs 6.68 ± 2.00) and infants were discharged on average 11.55 days earlier (15.55 ± 5.38 vs 27.10 ± 7.90). There was no significant difference in GA between the cue-based feeding group and the scheduled feeding group (P = 0.80). The difference of PMA in first oral feeding (P < 0.001), full oral feeding (P < 0.001), and the day of discharge (P < 0.001) between the cue-based feeding group and the scheduled feeding approach group was statistically significant (Table 3). The difference in weight between the two groups was not significant in each stage of assessment (P > 0.05) (Table 3). In addition, Table 3 shows a significant difference in milk volume only at the first oral feeding stage (P = 0.04). There was no significant difference between the two groups before intervention (P = 0.09), first oral feeding (P = 0.91), and full oral feeding (P = 0.41) regarding PIOFRAS. However, there was a significant difference in the day of discharge (P = 0.03). The mean score of PIOFRAS on the day of discharge in the cue-based feeding group was higher than that in the scheduled feeding group (Table 4). Differences in some dimensions of EFS were statistically significant, including Ability to Maintain Engagement in Feeding (AMEF) (P = 0.01) and Oral Feeding Recovery Assessment (OFRS) dimensions (P = 0.03) in the full oral feeding, and Ability to Coordinate Swallowing (ACS) dimension in the first oral feeding (P = 0.04) (Table 5).
| Characteristics | Cue-Based Feeding Group (n = 18) | Scheduled Feeding Group (n = 19) | P Value |
|---|---|---|---|
| Male, No. (%) | 11 (61.1) | 9 (47.4) | > 0.99b |
| Gestational age (d) | 222.94 ± 10.77 (218.23 - 228.09) | 223.84 ± 10.90 (218.92 - 228.63) | 0.80c |
| Birth weight (gr) | 1657.77 ± 363.59 (1502.69 - 1849.80) | 1601.31 ± 289.01 (1471.03 - 1733.30) | 0.60c |
| Apgar score 1 min | 5.77 ± 2.10 (4.73 - 6.72) | 5.47 ± 2.3 (4.57 - 6.38) | 0.65c |
| Apgar score 5 min | 8.16 ± 0.98 (7.68 - 8.58) | 8.10 ± 1.10 (7.61 - 8.57) | 0.85c |
| Milk, No. (%) | 0.56b | ||
| Breast | 3 (16.7) | 3 (15.8) | |
| Formula | 2 (11.1) | 5 (26.3) | |
| Breast and formula | 13 (72.2) | 11 (57.9) |
aValues are expressed as mean ± SD (CI 95 % [lower-upper]) unless otherwise indicated.
b Fisher's Exact Test.
cIndependent t-Test.
| Characteristics | Cue-Based Feeding Group (n = 18) | Scheduled Feeding Group (n = 19) | P Valueb |
|---|---|---|---|
| Duration of first oral feeding achievement (d) | 4.16 ± 2.97 (2.81 - 5.52) | 10.05 ± 6.85 (7.31 - 13.25) | < 0.001 |
| Duration of full oral feeding achievement (d) | 3.55 ± 1.24 (3.00 - 4.12) | 6.68 ± 2.00 (5.77 - 7.58) | < 0.001 |
| Duration of hospitalization (d) | 15.55 ± 5.38 (13.11 - 18.33) | 27.10 ± 7.90 (23.75 - 30.66) | < 0.001 |
aValues are expressed as mean ± SD (CI 95 % [lower-upper]).
bIndependent t-Test
| Characteristics | Cue-Based Feeding Group (n = 18) | Scheduled Feeding Group (n = 19) | P Value |
|---|---|---|---|
| PMA at first oral feeding (d) | 229.94 ± 10.06 (225.68 - 234.57) | 240.05 ± 11.30 (235.00 - 244.56) | < 0.001 b |
| PMA at full oral feeding (d) | 233.55 ± 9.33 (229.68 - 237.82) | 246.78 ± 10.86 (241.80 - 251.25) | < 0.001 b |
| PMA at discharge (d) | 237.77 ± 9.93 (233.50 - 242.23) | 251.84 ± 11.83 (246.37 - 256.80) | < 0.001 b |
| Milk volume of first oral feeding | 12.05 ± 5.81 (9.29 - 14.47) | 15.84 ± 5.87 (13.18 - 18.42) | 0.04 b |
| Milk volume of full oral feeding | 21.27 ± 5.82 (18.76 - 24.09) | 25.10 ± 5.79 (22.64 - 27.77) | 0.06 b |
| Milk volume at discharge | 28.05 ± 5.18 (25.90 - 30.58) | 30.26 ± 4.85 (28.25 - 32.64) | 0.27 b |
| Weight at first oral feeding (gr) | 1611.11 ± 351.30 (1463.35 - 1788.12) | 1654.68 ± 273.27 (1528.13 - 1773.52) | 0.67c |
| Weight at full oral feeding (gr) | 1696.11 ± 308.94 (1565.21 - 1852.10) | 1743.15 ± 274.30 (1622.61 - 1863.51) | 0.62c |
| Weight at discharge (gr) | 1757.22 ± 280.20 (1646.36- 1894.66) | 1840.00 ± 322.09 (1692.78 - 1978.26) | 0.40c |
Abbreviation: PMA, post menstrual age.
aValues are expressed as mean ± SD (CI 95 % [lower-upper])
bMann-Whitney Test.
cIndependent T-Test.
| Characteristics | Cue-Based Feeding Group (n = 18) | Scheduled Feeding Group (n = 19) | P Valueb |
|---|---|---|---|
| Before intervention | 18.55 ± 5.00 (16.14 - 20.83) | 15.68 ± 5.12 (13.45 - 18.05) | 0.09 |
| First oral feeding | 30.61 ± 0.91 (30.21 - 31.04) | 30.57 ± 0.83 (30.23 - 31.00) | 0.91 |
| Full oral feeding | 31.77 ± 1.00 (31.30 - 32.21) | 31.52 ± 0.84 (31.16 - 31.90) | 0.41 |
| Discharge day | 32.61 ± 1.14 (32.08 - 33.14) | 31.90 ± 0.87 (31.50 - 32.27) | 0.03 |
Abbreviation: PIOFRAS, preterm infant oral feeding readiness assessment scale.
aValues are expressed as mean ± SD (CI 95 % [lower-upper]).
bIndependent t-Test
| First Oral Feeding | Full Oral Feeding | Discharge Day | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Dimensions of EFS | Cue-Based Feeding (n = 18) | Scheduled Feeding (n = 19) | P- Valueb | Cue- Based Feeding (n = 18) | Scheduled Feeding Group (n = 19) | P- Value | Cue-Based Feeding Group (n = 18) | Scheduled Feeding Group (n = 19) | P- Value |
| OFRA | 2.17 ± 0.32 (2.01 - 2.25) | 2.11 ± 0.45 (1.91 - 2.33) | 0.96 | 2.67 ± 0.34 (2.51 - 2.82) | 2.57 ± 0.36 (2.41 - 2.73) | 0.43 | 2.89 ± 0.25 (2.75 - 2.98) | 2.79 ± 0.27 (2.67 - 2.91) | 0.27 |
| AMEF | 2.25 ± 0.42 (2.05 - 2.43) | 2.25 ± 0.31 (2.11 - 2.39) | 1.00 | 2.72 ± 0.25 (2.61 - 2.82) | 2.46 ± 0.33 (2.31 - 2.61) | 0.01 | 2.91 ± 0.17 (2. 83 - 2.98) | 2.84 ± 0.19 (2. 75 - 2.92) | 0.21 |
| AOOMF | 2.13 ± 0.32 (2.00 - 2.30) | 2.14 ± 0.39 (1.97 - 2.31) | 0.96 | 2.72 ± 0.28 (2. 58 - 2.84) | 2.68 ± 0.28 (2. 54 - 2.80) | 0.68 | 2.94 ± 0.16 (2. 86 - 3.00) | 2.82 ± 0.23 (2. 72 - 2.92) | 0.09 |
| ACS | 2.85 ± 0.17 (2.76 - 2.92) | 2.60 ± 0.47 (2.38 - 2.78) | 0.04 | 2.95 ± 0.09 (2.90 - 2.99) | 2.79 ± 0.41 (2.57 - 2.96) | 0.12 | 2.97 ± 0.06 (2. 94 - 3.00) | 2.92 ± 0.23 (2.81 - 3.00) | 0.34 |
| AMPS | 2.40 ± 0.35 (2.24 - 2.57) | 2.1 ± 0.41 (2.00 - 2.38) | 0.09 | 2.80 ± 0.14 (2.73 - 2.86) | 2.62 ± 0.43 (2. 41 - 2.80) | 0.10 | 2.95 ± 0.09 (2.90 - 2.99) | 2.87 ± 0.24 (2.74 - 2.96) | 0.19 |
| OFRS | 2.30 ± 0.64 (2.02 - 2.59) | 2.07 ± 0.50 (1.87 - 2.32) | 0.24 | 3 ± 0.00 (3.00 - 3.00) | 2.65 ± 0.44 (2.46 - 2.84) | 0.03 | 3 ± 0.00 (3.00- 3.00) | 2.94 ± 0.15 (2.86 - 3.00) | 0.16 |
Abbreviation: EFS, early feeding skill; OFRA, oral feeding readiness assessment; AMEF, ability to maintain engagement in feeding; AOOMF, ability to organize oral-motor function; ACS, ability to coordinate swallowing; AMPS, ability to maintain physiologic stability; OFRS, oral feeding recovery assessment.
aValues are expressed as mean ± SD (CI 95 % [lower-upper]).
bIndependent t-test
5. Discussion
In the present study, the infants in the cue-based feeding group started the first oral feeding with lower PMA than the scheduled approach group. The duration of full oral feeding achievement was shorter in the cue-based feeding group. Moreover, the length of hospital stay was shorter in the cue-based feeding group than that in the scheduled group.
The results of this study demonstrated that the infants of the cue-based feeding group started oral feeding on average 4 days sooner. Davidson et al and Chrupcala et al found no significant difference between groups for the initiation of oral feeding (1, 32); This finding may be due to the difference in the criteria for initiation of oral feeding. For instance, Davidson et al revealed that oral feeding was initiated only based on Oral Feeding Readiness Scale. However, in the present study, in addition to Oral Feeding Readiness Scale, we evaluated infants by PIOFRAS. Furthermore, the difference in PMA may be one of the reasons for differences in duration of hospitalization. The mean of PMA in the first oral feeding in the study by Davidson and colleagues was about 34 - 36 weeks. However, in our study, it was about 32 - 34 weeks.
Furthermore, in the current study, the infants in the cue-based feeding group achieved full oral feeding on average 3.13 days sooner, which is useful in reducing the consequences of gavage feeding. Kansas et al and McCain et al reported the achievement of full oral feeding after 5 days (33, 34) and Kirk et al stated after 6 days (21). Also, the results of McCain et al, Colling et al, Davidson et al, Gelfer et al and Morag et al demonstrated that the difference in the number of days is related to differences in the methodology (1, 4, 13, 31, 35).
More importantly, infants in the cue-based feeding group in the present study were discharged from the hospital on average 11.55 days earlier, and the duration of hospitalization was shorter than scheduled feeding. The earlier discharge has a significant effect on reducing the financial burden on the family, hospital, and government. Another benefit of early discharge is the reduction of anxiety and stress of the mother, the infant, and the family. Consequently, this early discharge will lead to more interaction between the infant and parents. These findings were consistent with previous reports (1, 13, 15, 31, 33, 35). The studies by Gelfer et al and McCain et al showed no statistically significant difference between the two groups, but clinically the cue-based feeding group was discharged earlier (4, 34). These findings indicate that the decision to discharge the infants depends on many factors, and the achievement of full oral feeding is only one of those factors. Another factor is the need for supplemental oxygen in premature infants. In the study by McCain et al (2012), some preterm infants needed oxygen despite achieving full oral feeding (34).
It is important that despite the use of comprehensive evaluation tools to measure the results accurately in the present research, the score of PIOFRAS only on the day of discharge in the cue-based feeding group was more than that of the scheduled feeding group. This difference demonstrates that the cue-based feeding approach affects the last stage of intervention. Furthermore, the score of EFS in each dimension was inconsistent in each stage, and most of the differences were observed between two groups in the full oral feeding stage. However, the feeding stages and discharge process of cue-based group were more rapid than the scheduled feeding group on average, and this impact of the cue-based feeding is essential in terms of clinical effectiveness. Inconsistency in the scores of EFS may be due to lack of assessment of infants in a specific condition, for example, an identical state of alertness (deep sleep, light sleep, drowsiness, quiet alert). After all, infants in different states of alertness showed different functions.
Results of the present research showed lower weight in cue-based feeding group that was inconsistent with results of the studies by Colling et al (1982), McCain et al (2001), Pucket et al (2008), and Davidson et al(2013)(1, 13, 15, 31). One of the main reasons for the higher weight of infants in the scheduled feeding group is that these infants achieved a given volume through gavage that was based on a specific program, regardless of their demand, and without making a great effort for feeding. Another possible reason is that the earlier discharge of infants in the cue-based feeding group can reduce the chance of weight gain while they are in the NICU.
One of the limitations of this study was that the infant’s behavioral patterns differed at each feeding and at the time of assessment, which likely affected the evaluation results.
In conclusion, the present study demonstrated that the cue-based feeding approach compared with the scheduled feeding approach in preterm infants without significant medical problems is an effective and safe approach that results in the earlier achievement of oral feeding, and less hospitalization time.
Finally, we suggest further research in the effectiveness of cue-based feeding examined by measurement tools that evaluate infants in a specific condition. We also recommend that parents’ satisfaction with the cue-based feeding approach be examined.