1. Background
The first clinical symptoms of patients with the new SARS-COV was reported in December 2019. Initially, the number of cases was low, but it rapidly spread out. By the end of January 2020, more than 10,000 cases infected with SARS-COV were reported from across China. At February 19 the number of infections had risen to 74,280 in China, and about 2009 deaths were reported in 24 countries outside of China (1).
The number of definitive and confirmed cases reached 80,935 in China, and 37,371 in other countries, the number of deaths caused by the COVID-19 has risen to 3,162 in China and 1,130 in other countries, as the World Health Organization reported on 11 March 2020 (2). Following the global spread of Covid-19, the World Health Organization declared, as a 6th public health emergency of international concern (3). At 7 May 2020 confirmed cases had risen to 3672238 and 254045 deaths (4). To control the Covid-19 outbreak efficiently, screening and identifying children for Covid-19, and early isolation, and managing the affected subjects is mandatory. Although PCR tests are suggested as standard tools for Covid-19 diagnosis, they are a time-consuming process, may have accessibility problems and highly probable false-negative results. It is recommended to syndicate all findings obtained from clinical characteristics, a history of contact, chest CT scan, and blood cell count with the NAT/PCR test as the standard diagnostic protocol in children (5-7). In this study, we investigated the results of screening of 474761 children under 19 years of age and identified epidemiological features of suspect cases in East Azerbaijan province, Iran.
1.1. Clinical Symptoms
Various health organizations around the world have reported different incubation periods for Covid-19 disease. Incubation times between 2-10 days (4), between 10-14 days (3), and between 2-14 days (8) have been reported. Covid-19 starts replicating in the respiratory system. A large amount of the virus replicates in the upper respiratory tract during an introductory period in infected persons, leading to the virus's spread to infect other hosts. It can lead to lesions in the lower respiratory tract in cells prone to destruction (9).
Approximately 81% of Covid-19 patients show mild symptoms and recover at home. In 14% of cases, severe symptoms including pneumonia and shortness of breath occur. In 5% of cases, the patient's condition goes to deterioration, leading to respiratory failure, infectious shock, and failure in other organs. Infection with covid-19 at primary stages is related with nonspecific and general symptoms such as fatigue, nausea, fever, body aches, and dry cough. Patients may have symptoms of nausea and diarrhea shortly before the fever. A small number of patients may also have headaches with hematemesis and may even be relatively asymptomatic (10). To date, there is no strong evidence of intrauterine transmission (3). Table 1 shows the epidemiological characteristics of Covid-19 according to previous researches.
| Component | Description | Source |
|---|---|---|
| The incubation period | WHO: 2-10 days (8) - China National Health Commission between 10-14 days (3) - CDC: 2-14 day (11). | (3, 8, 9) |
| Fatality rates | According to studies by Wang et al., the mortality rate for Quaid-19 disease is 2.84 percent, and according to meta-analyzes, the rate is 6.5 percent. | (11-13) |
| Transmission rate | The transmission rate in Yang et al. was 2.2 per case, and in the study of Wu et al., the transmission rate was 3.8 per patient. However, this rate does not include asymptomatic people. | (14, 15) |
| RO | According to a study by Liu et al., the RO rate in Covid-19 is between 1.4 and 6.49. On average, 3.8. | (16) |
Epidemiological Characteristics of COVID-19
2. Objectives
To assess the extent of the disease in the pediatric population in our region, we conducted a clinical pediatric screening for Covid-19 and evaluated factors that affected its manifestation in children.
3. Methods
This is a retrospective screening study of 474,761 children and teenagers under 19 years of age in two phases conducted in the province of East Azerbaijan, Iran. The screening lasted 35 days, between March 5, and April 8, 2020, when Covid-19 was in the full outbreak. The screening subjects were residents in the region under the medical supervision of Tabriz University of Medical Sciences. The initial screening was performed by investigating the clinical symptoms or those being in close contact with confirmed cases in their family. The suspected cases were referred to the hospital for further evaluation. In step 2 of screening, the cases were categorized in confirmed or probable groups (17).
Suspicion was based on one of the following criteria:
1. Having symptoms such as dry cough, chills with or without fever that could not be attributed to another etiological factor.
2. Having a history of contact with a confirmed case of Covid-19 during the last 2 weeks in a patient with respiratory symptoms (with any severity) or fever.
3. Decreased arterial blood oxygen saturation below 3% (Normal level 95–100) despite oxygen inhalation or below 90% in normal condition, respiratory distress syndrome, seizures or decreased level of consciousness, inability to eat and talk, shock.
4. High CRP, lymphadenopathy, thrombocytopenia, abnormal LDH level.
Probable cases were defined as having one of the following criteria:
1. Radiological manifestations include one- or two-way multi-lobule infiltration, ground glass appearance in CT scan of the lungs.
2. Inconclusive result: The unknown result of the PCR test.
Confirmed case: A person diagnosed with a positive PCR test as Covid-19 (7).
Data were analyzed with descriptive statistics and chi-square tests in SPSS 28.
4. Results
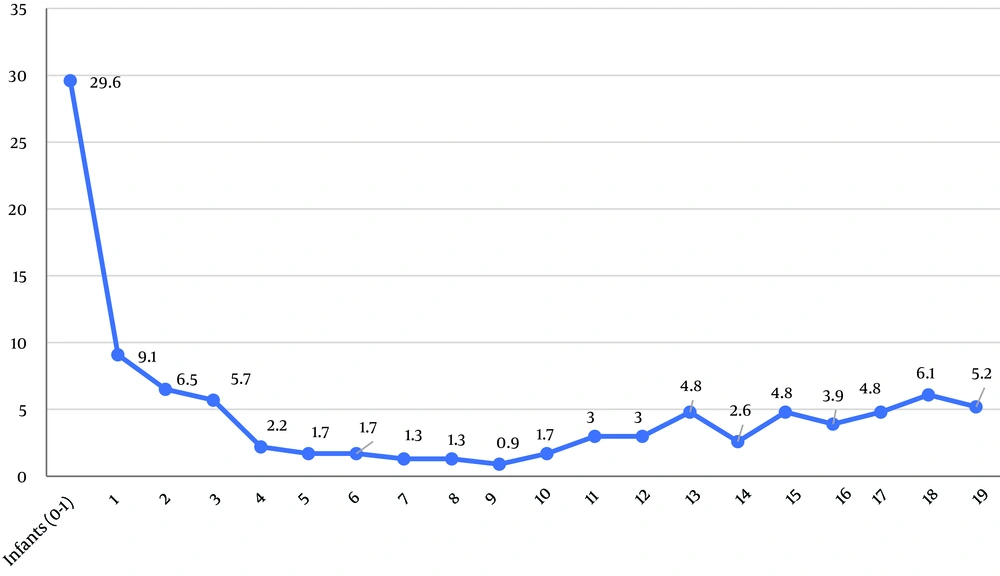
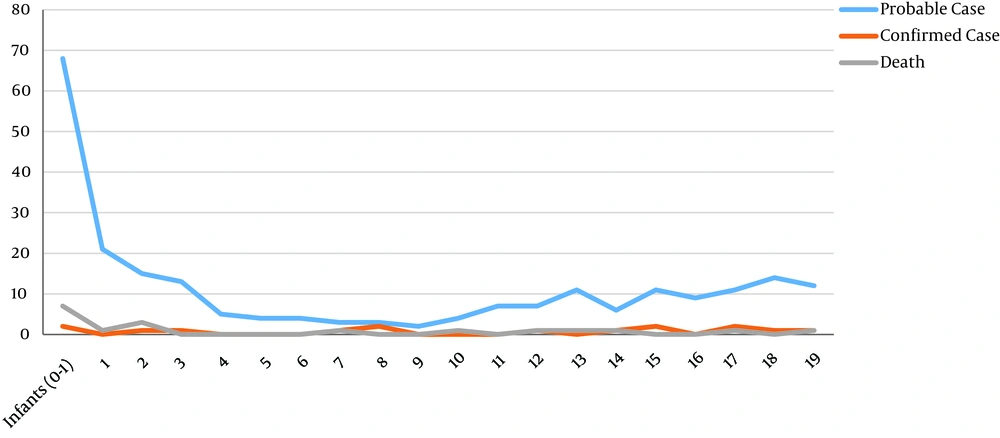
Between all the cases in the first screening, 680 children were considered as suspect cases, which were referred for the second screening, and in the second screening, 230 probable cases were referred to the hospital for further investigation. Among these, 105 were girls (45.7%) and 125 boys (54.3%). The most suspected cases were infants (Figure 1) and then 1-3 year olds, due to the high rate of pneumonia at this age. The graph of suspected cases has a gentle slope in 3-10 year olds, and increases in 11-year olds; probable cases followed the same trend (Figure 2).
All of the probable cases had pneumonia and symptoms of shortness of breath and cough. Fever over 38˚C (56.7%), hypotension (17.4%), hemoptysis (16.1%), sore throat (11.6%), and difficult breathing (6.7%) were other symptoms of the disease; 26% of the patients had a history of chronic disease (mainly pulmonary and cardiac) (Table 2). Of probable cases, 39 (17.0%) were hospitalized, and 18 (7.8%) cases died (Table 3), 137 cases received ambulatory treatment.
According to Table 4, there was a statistical relationship between the probable cases and the disease symptoms (P < 0.05). However, only 15 (6.5%) cases had a positive PCR test. As shown in Table 5, there was no relationship between clinical signs and test results (P > 0.05). There was a statistical relationship between age and probable cases (P < 0.05) and between the positive test result and the hemoptysis test (P < 0.05) (Table 6). However, there was no relationship between other symptoms and test results (P > 0.05). Table 7 shows a statistically significant relationship between death and having underlying disease (P < 0.05). However, as Table 8 shows, there was no relationship between death and clinical symptoms (P > 0.05).
| Frequency | Percent | |
|---|---|---|
| History of previous illness | 60 | 26.8 |
| Pneumonia | 218 | 97.3 |
| Fever above 38°C | 127 | 56.7 |
| Sore throat | 26 | 11.6 |
| Cough | 224 | 100.0 |
| Shortness of breath | 224 | 100.0 |
| Difficult breathing | 15 | 6.7 |
| Hemoptysis | 36 | 16.1 |
| Hypotension | 39 | 17.4 |
Clinical Signs of Probable Cases
| Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|
| Hospitalized | 39 | 17.0 | 17.0 | 17.0 |
| Hospital discharge | 173 | 75.2 | 75.2 | 92.2 |
| Death | 18 | 7.8 | 7.8 | 100.0 |
| Total | 230 | 100.0 | 100.0 |
Patients' Outcome
| Value | df | Asymptotic Significance (2-sided) | |
|---|---|---|---|
| Pearson Chi-Square | 62.203 | 38 | 0.008 |
| Likelihood Ratio | 59.345 | 38 | 0.015 |
| Linear-by-Linear Association | 8.329 | 1 | 0.004 |
| Number of Valid Cases | 230 |
The Relationship Between Clinical Signs of Probable Cases
| Value | df | Asymptotic Significance (2-sided) | |
|---|---|---|---|
| Pearson Chi-Square | 1.766a | 2 | 0.414 |
| Likelihood Ratio | 1.507 | 2 | 0.471 |
| Linear-by-Linear Association | .047 | 1 | 0.828 |
| Number of Valid Cases | 224 |
The Relationship Between the Test Result and Clinical Signs
| Value | df | Asymptotic Significance (2-sided) | Exact Sig. (2-sided) | Exact Sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson Chi-Square | 7.943 | 1 | 0.005 | ||
| Continuity Correction | 5.966 | 1 | 0.015 | ||
| Likelihood Ratio | 6.132 | 1 | 0.013 | ||
| Fisher's Exact Test | 0.013 | 0.013 | |||
| Linear-by-Linear Association | 7.908 | 1 | 0.005 | ||
| Number of Valid Cases | 224 |
The Relationship Between the Confirmed Case and Hemoptysis
| Value | df | Asymptotic Significance (2-sided) | Exact Sig. (2-sided) | Exact Sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson Chi-Square | 15.874 | 1 | .000 | ||
| Continuity Correction | 13.740 | 1 | 0.000 | ||
| Likelihood Ratio | 13.756 | 1 | 0.000 | ||
| Fisher's Exact Test | 0.000 | 0.000 | |||
| Linear-by-Linear Association | 15.803 | 1 | 0.000 | ||
| Number of Valid Cases | 224 |
The Relationship Between Death and Having the Underlying Disease
| Value | df | Asymptotic Significance (2-sided) | Exact Sig. (2-sided) | Exact Sig. (1-sided) | |
|---|---|---|---|---|---|
| Pearson Chi-Square | 0.155 | 1 | 0.693 | ||
| Continuity Correction | 0.021 | 1 | 0.884 | ||
| Likelihood Ratio | 0.157 | 1 | 0.692 | ||
| Fisher's Exact Test | 0.806 | 0.446 | |||
| Linear-by-Linear Association | 0.155 | 1 | 0.694 | ||
| Number of Valid Cases | 224 |
The Relationship Between Death and Clinical Signs
5. Discussion
This investigation aimed to analyze the first Covid-19 screening study among 474,761 children and adolescents under 19 years old in Iran. In accordance with previous studies (18, 19), compared to adults, the Covid-19 disease in children was less severe, and the mortality rate was lower.
The initial screening was performed by investigating the clinical manifestations in children or those children being in contact with confirmed cases in the family. The results of this study showed that boys were slightly more affected than girls (54.3% vs. 45.7%), which are similar to the three recent epidemiological studies (18-20).
The most suspected cases in our study were infants (Figure 1), followed by 1, 2, 18, 3, 19-year-olds. This result is similar to the Dong et al study (20). However, children of all ages can be infected (21). According to SJ Seyedi et al Covid-19 among children and infants is associated with mild respiratory or nonspecific asymptomatic infection symptoms; in neonates and infants, it may present with fever, dry cough, nasal discharge, distress, fatigue and sore throat (7).
In our patients, approximately all of the cases (97.3%) had pneumonia and the most common symptoms were shortness of breath, cough, and fever over 38°C, hypotension, Hemoptysis, sore throat, and difficult breathing respectively, 26% of patients had a chronic disease (Table 1).
Huang et al found that 98% of COVID-19 patients had a fever, in 78% above 38°C. They reported that 76% of patients had a cough, 44% had fatigue and muscle aches, and 55% had dyspnea. A small number of patients had sputum expectoration (28%), headache (8%), Hemoptysis (5%), and diarrhea (3%) (22).
A study in China found that only 43.8% of patients had a fever and 15.7% had severe pneumonia (19). Their typical symptoms included fever and acute respiratory infections, sore throat, cough, sneezing, fatigue, and myalgia. In the Wuhan Children's hospital, the most common symptoms were cough (48.5%), pharyngeal erythema (46.2%), and fever of at least 37.5°C (41.5%) (23).
In Dong et al study, 28.7% of children demonstrated tachypnea and tachycardia (42.1%) on hospital admission (23). In our study, 39 were hospitalized (17%), 173 (75%) received ambulatory treatment, and 18 (7.8%) died.
In our study, only 15 (6.5%) had a positive PCR test. The relationship between age and possible cases and between the positive test result and the hemoptysis test was statistically significant (P < 0.05). There was no statistical significance between other symptoms and test results (P > 0.05). There was a statistically significant relationship between death and previous medical history (P < 0.05).
In 2143 pediatric patients in Dong et al study, the disease was confirmed by a combination of exposure history and clinical manifestations. Of these, 34.1% had the laboratory-confirmed disease, while in the remainder, the disease was clinically suspected (23). Dong et al. found that more than 90% of children diagnosed with clinically diagnosed Covid-19 or laboratory-verified had an asymptomatic, mild, or moderate disease. From the rest, 5.2% had severe disease and 0.6% had a critical disease (23). In the US study, 1.6%-2.5% of children needed hospital admission with no child needing intensive care (24). Moreover, in Wuhan Children's Hospital, 1.8% of children required intensive care; also, all of those had underlying disease (25).
In this study, the death rate was 7.8%, but none of them had a positive test result. On March 18, 2020, Italian data reported that only 1.2% of Italian cases with COVID-19 were children, with no deaths. Indeed, no deaths had been reported below the age of 30 years in Italy (26). In Lee et al study, the overall mortality rate from severe respiratory distress syndrome (SARS) ranged from 7% to 17% and people with basic medical conditions and people over the age of 65 had a mortality rate of more than 50 percent, but no deaths were reported under the age of 24 (27). In our study, a significant percentage (36.4%) of suspect cases had an underlying disease and the frequency of underlying disease was significantly related to death and congenital pulmonary and cardiovascular disease was the most prevalent.
Pneumonia is the most common cause of death in children (28); of the factors influencing children's mortality in this study could be underlying diseases and pneumonia. The highest age range for pneumonia is under one year, and more than half of mild respiratory infections occur in children under one year old. In other studies, congenital heart disease and bronchopulmonary disease were more severe with acute respiratory illness, especially RSV (29, 30).
5.1. Conclusion
Parainfluenza viruses are a major cause of respiratory illness in children. They multiply in the upper respiratory tract and cause a range of mild respiratory illnesses up to snoring and pneumonia. Most children usually experience these viral infections in the first years of life. Immunity from the disease is not protective and re-infection occurs throughout life (31).
The virus is spreading worldwide and the infection is more common in children (4, 20, 32). Children infected with COVID-19 are chiefly asymptomatic carriers, which means they have a high potential to transmit and spread the disease in societies (7). The symptomatic pediatric cases have mainly pneumonia and shortness of breath, cough, fever over 38°C, hemoptysis, and sore throat. It is recommended to hospitalize children with shortness of breath, cough, pneumonia, fever over 38°C, and underlying disease.
5.2. Limitations
This study also has some limitations. We suggest that some suspected cases might be caused by other respiratory infections, for example, RSV. We did not have information on children’s exposure history, and thus, the incubation period was not examined in this study.