1. Background
Pediatric airway poses a separate set of risks and manipulation methods as compared to adult airway due to the anatomical as well as physiological differences between them. These include a relatively large occiput and tongue, more cephalad larynx, narrowed epiglottis, and anteriorly placed vocal cords (1).
Over the past decade, methods to improve airway visualization have been developed, among which is the advent of video laryngoscopy. Two of the most commonly used video laryngoscopies are GlideScope® (Verathon Medical) and C-MAC® (Karl Storz). As compared to direct laryngoscopy, C-MAC® has been shown to significantly enhance glottic view and improve Cormack-Lehane score in pediatric patients with normal airway, while GlideScope® further enhances view in difficult airway patients (2, 3). Direct laryngoscopy requires alignment of the pharyngeal, laryngeal, and tracheal axes, with displacement of the tongue, which can often be difficult in pediatric patients due to anatomical differences. The usage of a video laryngoscope can negate these difficulties as insertion requires minimal head manipulation, no tongue displacement and provides high-resolution images of the laryngeal inlet and glottic (4). Comparison between these two devices, in terms of success rate in adults, has shown no superiority over the others (5).
A bulk of literature compares GlideScope® and C-MAC® video laryngoscopy with conventional laryngoscopy. A study by Redel et al. found that GlideScope® laryngoscopy is comparable to Macintosh laryngoscopy in patients age 10 years or less with normal airway (6). Even in neonates and infants, GlideScope® laryngoscopy is able to demonstrate better a glottic view as compared to direct laryngoscopy (7). Vlatten et al. (8) found that Karl Storz-DCI video laryngoscope improved glottic view in children with normal airway anatomy, but longer time to intubation. A study comparing usage of GlideScope® and Karl Storz DCI® in a pediatric manikin showed no difference in tracheal intubation time and satisfaction score between the two methods (9). In the adult population, a retrospective study by Mosier et al. (5) compared the use of C-MAC® and GlideScope® in the emergency department and found both methods had similar rates of successful intubations. The usage of C-MAC® in adult patients in ICU settings has also improved laryngeal imaging and improved the intubating success rate on the first attempt in patients with predictors for difficult intubation.
2. Objectives
This study aimed to compare intubation time between these common video laryngoscopes specifically in pediatric patients, as well as to determine glottic view and satisfaction score using these devices among anesthetists.
3. Methods
3.1. Study Setting and Participants
The patients were recruited from December 2018 till November 2019 in operation theatres of a tertiary teaching hospital. Sixty-five American Society of Anesthesiologists status I or II patients aged 3 - 12 years old requiring elective operation were recruited to the study. Obese patients with a body mass index (BMI) of higher than 30 kgm2, patients with features of difficult airway, risks of pulmonary aspiration, or any history of difficult intubation were excluded from this study.
3.2. Study Design
This prospective, randomized study adheres to CONSORT guidelines and was approved by the Local Ethics Board Committee (code: FF2019004) on 12 September 2018 and registered under Clinicaltrials.gov (code: NCT04145089). The parents of the patients were counseled, and written informed consent was obtained during premedication round. The patients were fasted for at least 6 hours prior to their surgery. They were randomly assigned to groups 1 and 2 with 1:1 allocation ratio by means of computer-generated list of random numbers by primary investigator on the day of surgery. Group 1 patients were intubated with C-MAC® video laryngoscopy, while group 2 patients were intubated using GlideScope® video laryngoscopy. Group allocation was sealed in an envelope, and the envelope were clip together with General Anesthesia Assessment form. The laryngoscopist would open the envelope prior to induction. Performance blinding was not possible in this study.
Before induction of anesthesia, monitoring with pulse oximetry, blood pressure, and electrocardiogram were attached to the patient as per standard protocol. The patient was induced with sevoflurane 8% with 100% oxygen at 8L/min and was put supine with head resting on pediatric size silicone doughnut. Intravenous cannulation was obtained, and IV fentanyl 2 mcg/kg and IV atracurium 0.5 mg/kg were administered. Intubation was done after 180 sec of administration of IV atracurium with the study assigned device. The size of endotracheal tube chosen depended on patient’s age and weight. All laryngoscopists had performed intubation using both C-MAC® and GlideScope® at least 20 times formerly. Intubations were performed in a standing position, using a tracheal tube reinforced by either a stylet shaped similarly to the blade of C-MAC®, or GlideRite stylet for GlideScope®.
The duration of time for tracheal intubation was recorded by the primary investigator using a CASIO HS-3V-1R Sports Track Field Digital Stopwatch. It was defined as the time from insertion of the laryngoscope blade into the mouth (between the teeth) until the presence of capnography wave on the monitor. Time of intubation during the first attempt was recorded as T1. There was a maximum of two attempts. When the Cormack Lehane view was 3 or 4, additional airway adjunct was used with or without external laryngeal maneuver and readjustment of head position to optimize visualization. During each intubation attempt, whenever any complications such as lip trauma, dental trauma, or episodes of desaturation were less than 95%, it was recorded and managed accordingly. If the first intubation attempt failed, the attempt was terminated, and the next attempt would only be initiated after mask ventilation. The timing was reset and recorded as T2.
When despite two attempts and the tracheal intubation was still unsuccessful, the airway was managed according to local hospital difficult airway protocol to the discretion of the anesthetist providing care for the patient and are considered dropout. In the end, the total time of intubation (TTI) and Cormack-Lehane grade were documented. TTI is defined as total time required for intubation for the first successful attempt. After intubation, the ease of intubation and anesthetist satisfaction with the respective device was recorded using a simple questionnaire using a 5-point Likert scale, ranging from very dissatisfied to very satisfied. Anesthetists were also asked whether they would like to use the device next time.
The primary endpoint of this study was time taken for endotracheal intubations. The intubation time was defined as the time from insertion of the laryngoscope blade into the mouth (between the teeth) until the presence of capnography wave on the monitor. Secondary outcomes were the number of attempts, additional maneuvers required for intubation, and complications such as dental and lip trauma and desaturations. Anesthetic satisfaction scale was also assessed.
3.3. Sample Size Calculation
The sample size was calculated based on our main objective, which was to compare intubation time between these two devices. Based on Kim et al. (10), where there was a significant difference in regard to the mean time for tracheal intubation between Glidescope®. Therefore, by using Snedecor and Cochran’s formula and the mean difference of 12.2, 32 patients per group were recruited with 10% of dropout rate, power of 80%, and an α-value of 0.05.
3.4. Statistical Analysis
The data were analyzed using the SPSS (Statistical Package for The Social Sciences) version 20 software. Chi-square test or Fisher exact test was used to calculate significant differences for categorical variables in demographic data, satisfaction score, and requirement for external laryngeal manipulation between the two groups. Independent t-test was used to determine significant differences for continuous variables such as age and weight. As the primary outcome (total time to intubate in both groups) was not normally distributed, the data were analyzed using Mann Whitney U-test. A P-value of less than 0.05 was considered statistically significant.
4. Results
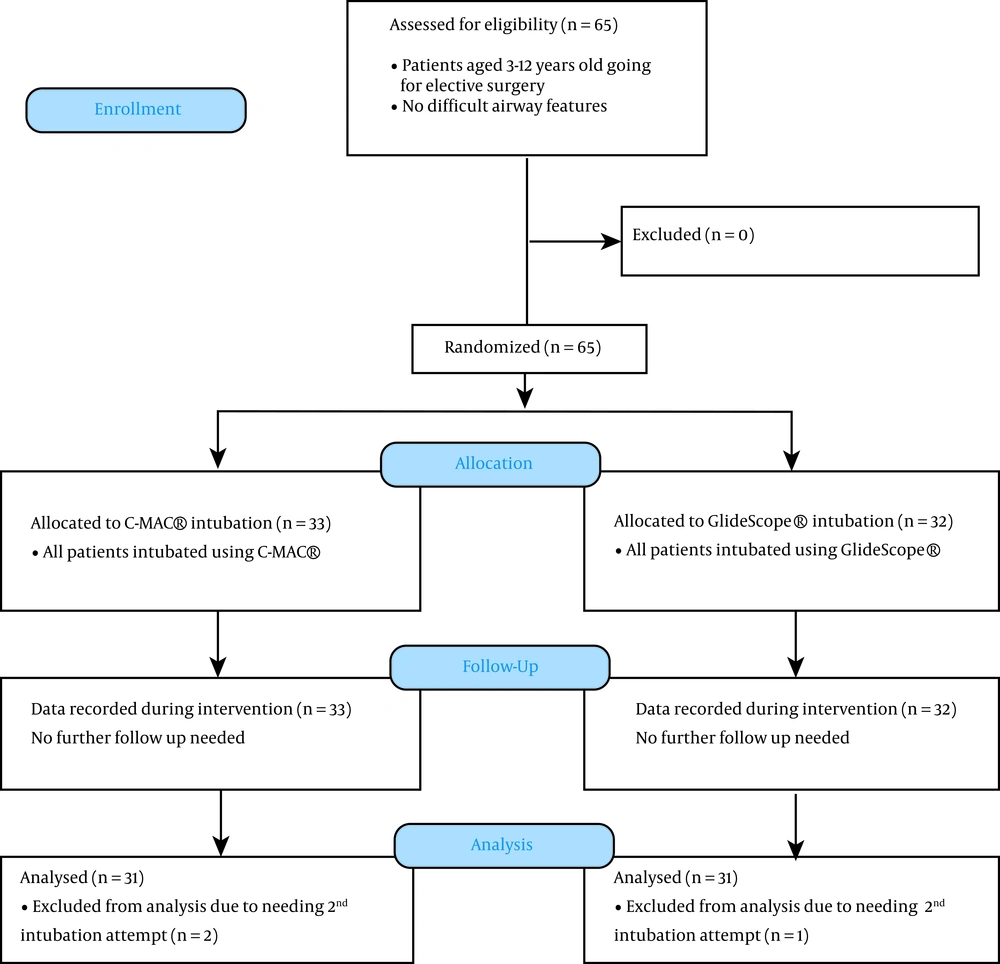
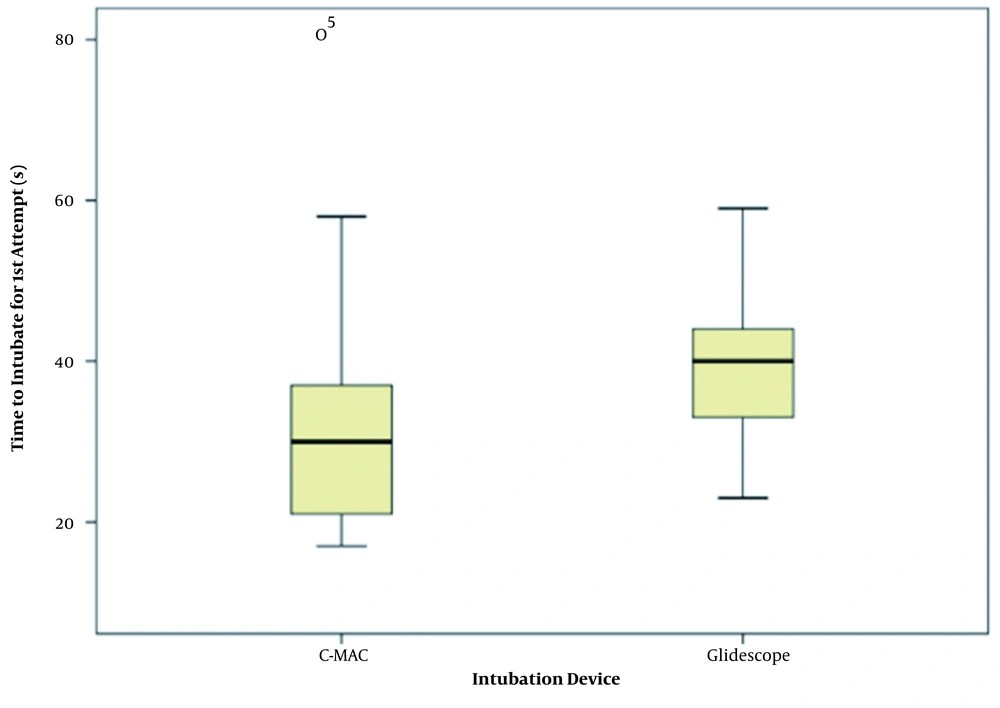
A total of sixty-five patients were recruited into the study. There were no dropouts. A description of enrolment is summarized in Figure 1. The demographic data of the patients in both groups and total time of intubation are shown in Table 1. There were no significant differences in the demographic data between the two groups. The median for total time to intubate for C-MAC® was 30 seconds, and 40 seconds for GlideScope® The difference was statistically significant (p = 0.001). Figure 2 shows a Box plot for time to first successful intubation between C-MAC® and GlideScope®.
| Group 1 (N = 33) | Group 2 (N = 32) | P-Value | |
|---|---|---|---|
| Age, y | 6.06 ± 2.03 | 6.81 ± 2.86 | 0.229 |
| Gender | 0.718 | ||
| Male | 19 (57.6) | 17 (53.1) | |
| Female | 14 (42.4) | 15 (46.9) | |
| Race | 0.355 | ||
| Malay | 29 (87.9) | 29 (90.6) | |
| Chinese | 4 (12.1) | 1 (3.1) | |
| Indian | 0 (0) | 1 (3.1) | |
| Others | 0 (0) | 1 (3.1) | |
| ASA | 0.699 | ||
| I | 28 (84.8) | 26 (81.3) | |
| II | 5 (15.2) | 6 (18.8) | |
| Body weight, kg | 17.05 ± 3.94 | 20.13 ± 8.14 | 0.056 |
| Total time to intubate, sec | 30 (21 - 38) | 40 (33 - 45) | 0.001 |
| External laryngeal manipulation | 3 (9.1) | 2(6.3) | 1.000 |
Demographic Data and Time to First Successful Intubation and Additional Maneuver in Both Groups
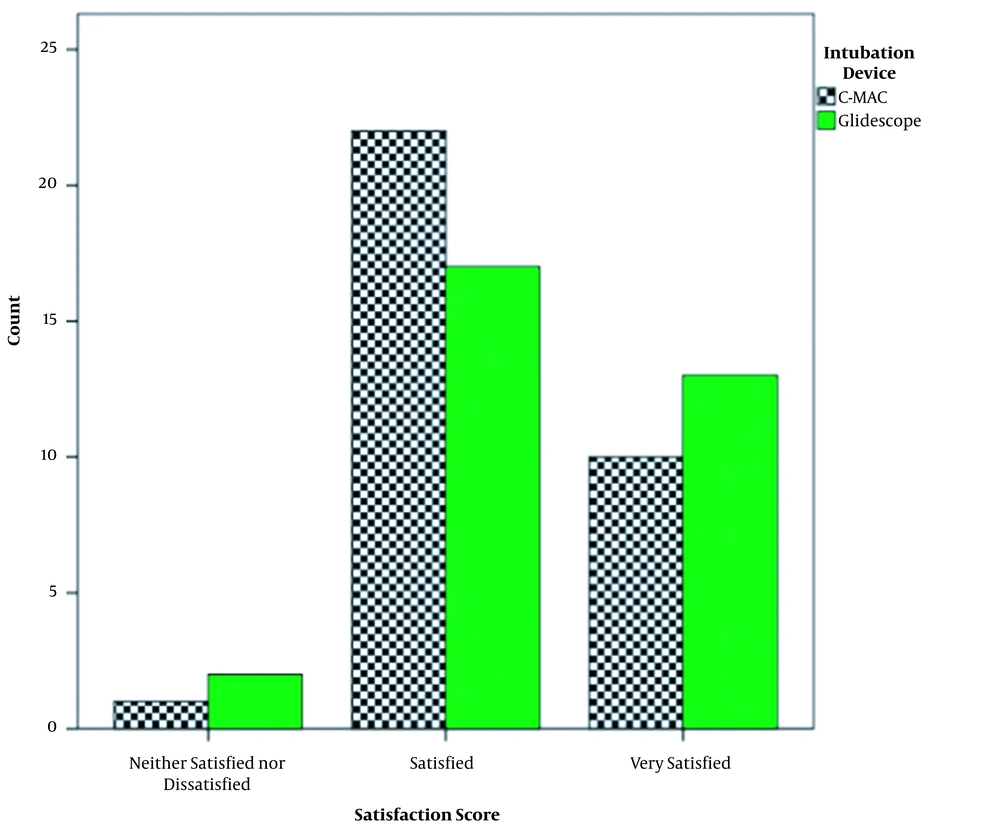
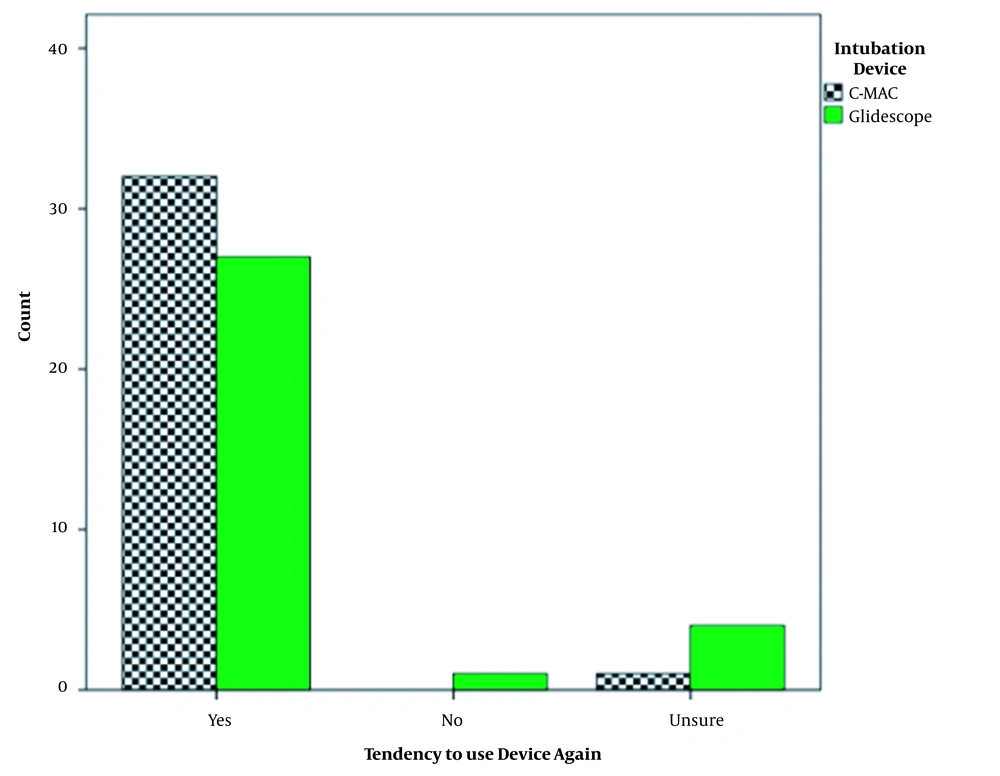
All patients had a Cormack Lehane 1 view on both devices. None of the patients required any additional airway adjunct. There were no intubation-related complications recorded, such as desaturation, dental, or lip trauma. Operator’s satisfaction score and their decision to reuse the device in next pediatrics intubation were comparable between both groups, as shown in Figures 3 and 4.
5. Discussion
Tracheal intubation using video laryngoscope has increasingly become more relevant in the management of the airway during COVID-19 pandemic. Its usage has been recommended to reduce the proximity of the laryngoscopist to the patient’s airway, especially in COVID-19 patients (11). To date, there were no prospective studies comparing GlideScope® and C-MAC® video laryngoscope in the pediatric population. The primary finding of this study showed a statistically significant longer time to intubate in the GlideScope® group as compared to C-MAC® group (40 sec vs 30 sec, P = 0.001). This is in contrast with Hurford and White’s finding (9), who found that there is no difference in intubation time between GlideScope® and Karl Storz DCI using Miller blade in infant manikin. However, in a study comparing three video laryngoscopes in difficult intubation adult manikin, GlideScope® has been shown to have prolonged intubation time as compared to C-MAC® (12).
First pass success rate for GlideScope® is slightly higher than C-MAC® (96.8% vs 93.9%), but the difference is not statistically significant. This is similar to findings in Mosier et al. (5), who compared C-MAC® Vs. GlideScope® in adult patients (96% Vs. 97%). On the contrary, there is higher first-pass success in C-MAC® compared to GlideScope® intubation in pediatric patients aged < 18 years in the emergency department (13). Despite the longer time to intubate in the GlideScope® group, there was no difference in terms of additional maneuvers required to improve intubation, such as external laryngeal manipulation, and no additional airway adjunct was required. In addition, although statistically significant, the time difference between these two devices is merely 10 seconds, which in author’s opinion does not translate into clinical significance. There were no adverse events associated with both video laryngoscopes in this study. A meta-analysis in 2014 that compared numerous video laryngoscope (among them is GlideScope®) data with direct laryngoscope showed similar rates of intubation-associated complications such as desaturation and lip, or oral trauma (14). Both devices achieved excellent glottic view (100% Cormack Lehane 1 view) with comparable satisfaction scores by the operators. This is consistent with Healy et al. (12), who found that both devices are comparable in terms of glottic view in simulated difficult adult manikin intubation. However, it must be noted better Cormack Lehane view in video laryngoscope does not always translate into easier tracheal intubation as the angle of view is increased due to lens position near the tip of the blade (15). In our study, the Cormack Lehane view is still used as a comparative tool to assess glottic view between these two devices as there is no standard scoring available yet specific to video laryngoscopes.
There are numerous reasons that may contribute to longer time to intubate in GlideScope® group. Familiarity with C-MAC® is greater as the curved blades are similar to the Macintosh blades in terms of size and shape. To optimize intubation, a ‘rocking action’ is recommended in GlideScope® intubation in contrast to the usual ‘lifting’ maneuver used in conventional Macintosh or C-MAC® blade (16). There were two blade sizes of GlideScope® used in this study, including LoPro S2 and LoPro S3. They boast the signature hyperangulated blade and low profile design to improve maneuverability and workspace. The new LoPro blade size 2.5, which is recommended for 10 kg to 28 kg was not available during the time of study, and this may influence the ease of laryngoscope in our selected age group’s weight (mean weight 17 - 20 kg).
The principal limitation in using GlideScope® is not in getting a good glottic view but the skill to manipulate the endotracheal tube through the vocal cords (17). Specific techniques will facilitate the passage of tube during intubation, such as usage of Gliderite stylet and the withdrawal of stylet by 3 cm upon entering the glottic to avoid hitting the tracheal wall. Both methods were used in this study. Insertion of GlideScope® blade also requires a more careful approach due to the hyper angulated shape to avoid injuring the palate. More time was also needed to remove the Gliderite stylet as compared to the usual stylet due to its J-shape. Another factor that may contribute to the difference in intubation time is the length of capnography tube used during the surgery, as the endpoint of intubation is the detection of capnography wave. In shared airway surgeries such as in maxillofacial or ear, nose, and throat surgery, the side stream capnography tube used is longer, and this may end up with longer transit time and a delay in capnography wave detection (18).
The laryngoscopists for this study were anesthetists with experiences in both C-MAC® and GlideScope® intubation. However, their clinical experiences range from senior pediatrics anesthetists to junior anesthetists. This may influence the time taken to intubate using both devices. Despite that, in a study comparing experienced and inexperienced users using these devices in pediatric manikin, GlideScope® has also been shown to exhibit longer intubation time compared to C-MAC® and direct laryngoscope in both users (17).
There were several limitations to this study. It is not possible to blind the operators prior to induction of anesthesia. Intubations were done by multiple operators, and each operator has his/her own personal speed and preferences in intubating patients. As GlideScope® has a different blade design compared to the conventional Macintosh blade, it requires a slightly different set of skill to optimize the speed of intubation. This study did not extrapolate and compare the time between the two devices and its significance on the efficiency of operation theatre’s time utilization and its turnover. This could have been additional useful information for the overall operational flow to the hospital system.
5.1. Conclusions
The time taken to intubate using GlideScope® is significantly longer compared to C-MAC® in pediatric patients with a normal airway. However, their first pass success rate is comparable, and both are not associated with any increase in the incidence of airway-related complications. Anesthetist satisfaction scores were also comparable.