1. Background
Advances in neonatal and prenatal medicine in addition to the use of modern equipments has improved the survival of premature and malnourished babies during recent years (1). Prolonged hospitalizations in the Neonatal Intensive Care Unit (NICU) for low birth weight (BW) infants and critically ill patients necessitates long-term administration of hypertonic fluids and salts, total parenteral nutrition (TPN), and various antibiotics emphasizes the importance of the need for achieving safe peripheral blood vessels and more effective using of these vessels (1-4).
On the other hand, concerns with surgical embedding of the central veins to establish a central venous line (CVL) include the use of anesthesia, embedding needed time, and elevated cost (3, 5). Today, peripherally inserted central catheters (PICC) are less invasive, provide safe venous access with minimal manipulation and decreased complications, and allow for the possibility of long-term maintenance of the catheters. There is increased parental satisfaction due to the decreased vein thrombosis and reduced infant pain and anxiety, which is essential according to the Newborn Individualized Developmental Care and Assessment program (NIDCAP) protocols (3, 6, 7).
Installation of a PICC requires training for placement, care, monitoring of possible complications, and awareness of malpositioning (6, 7). Complications of PICC include cardiac arrhythmias, accumulation of fluid in the pericardium with cardiac tamponade, an atrial rupture with cardiac tamponade, intravenous (IV) catheter rupture and subsequent catheter embolism, clot formation, diffuse or localized infection, nerve damage, air embolism, ruptured catheterization due to severe injection pressure, extravasation and leakage, bleeding, and rupture of the arteries (2, 8).
The PICC catheter end position assessment is traditionally performed by a standard chest radiography, which sometimes requires a second radiograph in a different position (e.g., right lateral position) to reduce improper placement of PICC relative to the mediastinal structures (9). However, evidence has shown that the use of ultrasound for monitoring the PICC placement can significantly increase the overall success rate of the procedure and minimize the risk of thrombosis and X-ray exposure (10, 11).
2. Objectives
We designed this study by taking into consideration the importance of evaluating the PICC catheter end position and the difficulty of PICC examination by ultrasound due to the small size of the catheter. The purpose of this study was to assess the ability of ultrasound and conventional radiography to ascertain the location of the PICC placement in hospitalized infants, and determine the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of both methods.
3. Methods
3.1. Study Design and Inclusion Criteria
This prospective descriptive-analytical (evaluation of methods) study was performed in the NICU of Tehran Children’s Medical Center (tertiary level), Iran from July, 2019 to December, 2019. The Ethics Committee of Tehran University of Medical Sciences and the Neonatal Health Research Center, Research Institute for children’s Health, Shahid Beheshti University of Medical Sciences approved this study following the necessary coordination with NICU personnel, the trained nursing team, the person in charge of the PICC, radiology department, and pediatric heart service. From July 6, 2019 to December 5, 2019, there were 90 infants who, according to the neonatal subspecialty opinion and the department protocol, met the criteria for PICC placement for long-term or moderate IV drug therapy or antibiotic therapy (more than six days), IV feeding, difficult access to blood vessels, or very low BW (< 1500 g) (2). The infants were enrolled in the study after their parents received an explanation of the study protocol and signed the informed consent.
3.2. Sample Size
According to Telang et al. (12), real-time ultrasonography (RTUS) has a sensitivity of 94% to detect the correct placement of the PICC catheter. The frequency of correct placement was reported to be 88%. We calculated a study sample size of 89 infants by using the formula for estimating sample size in a cross-sectional study and by taking into consideration 95% sensitivity and 5% error.
3.3. Data Collection
Infant demographic characteristics of gestational age, neonatal weight, and PICC embedded age, and information such as catheter embedding location, underlying disease, and catheter embedding indication were recorded in a researcher-developed questionnaire. The nurses who assisted with PICC insertion recorded the following information in the questionnaire: specifications of the applied processor, catheter type (silicone), size (1 and 2 francs), location of the implant, implant date, and dressing date.
Measurement of the amount of PICC catheter insertion: (A) Insertion from the upper limb: The tip of the catheter was placed in the superior vena cava (SVC). Measurement was done from the entrance place to the limb or the space between the third rib for installation in the upper limb, while the arm is at a 90-degree angle; (B) insertion from the lower limb: The catheter tip was placed in the IVC above the lumbar vertebra 4 or 5 or the iliac crest and below the right atrium (RA). Measurement was done from the entry point to the xiphoid appendage for implantation at the lower end. The optimal position of the PICC catheter end is considered in the case of implantation of the upper limb inside the SVC or at the junction of SVC and RA, and in cases of implantation of the lower limb at the junction of IVC and RA. The atrium is also considered acceptable if it does not move through the atrial wall or through the tricuspid or coronary sinus.
The PICC was sterilized and implanted by a fixed catheter implantation team consisting of NICU nurses and head nurses who were trained in implantation, care, removal and complications of PICC (PICC nurse) with the participation of neonatal flow. Catheter insertion is performed in completely sterile conditions. The catheters were disposable in a sterile package and immediately after the catheter implantation, a chest anteroposterior (AP) or abdominal radiography was performed using the same imaging device for all study patients. The results were reported and recorded by a radiologist. An ultrasound was performed as soon as possible at each infant’s bedside with a portable unit device (Contron Medical; Imagic Agile, Mehrkam Tajhiz, Iran). A single radiologist with the cooperation of a pediatric cardiologist conducted the ultrasound. Both the radiologist and pediatric cardiologist were blinded to the patient’s radiography report. In cases where the ultrasound images indicated that the end of the catheter was located in the vessels close to the heart or inside the heart, an echocardiogram was performed for a more accurate examination at the earliest possible time and within the first 24 h after implantation.
3.4. Exclusion Criteria
Contraindications to PICC implantation in the infants included perfusion disorders in the limbs, susceptibility of venous thrombosis in those with coagulation disorders, dermatitis, or local hematoma that prevented access to the peripheral veins, anatomical abnormalities that would interfere with proper placement (e.g., Erb’s palsy), and sepsis that was confirmed by a positive blood culture prior to antibiotic therapy (2).
3.5. Statistical Analysis
Confidential data were entered into SPSS software V.21 and subjected to descriptive and analytical analyses. Descriptive statistics were considered as the absolute and relative frequency for qualitative variables, and mean variables and standard deviation (SD) for quantitative variables. A comparison of qualitative variables between the two groups was performed with the chi-square test. Sensitivity, specificity, PPV, and NPV of the ultrasound were calculated and compared to radiography as the gold standard.
The correlation between the ultrasound and radiography results based on variables such as sex and age was assessed using the Pearson correlation test. The consistency of these results was evaluated by calculating the Kappa coefficient. A P value < 0.05 was considered to be statistically significant.
4. Results
In the present study, a total of 90 infants were examined, of which 45 infants were girls (50%) and 45 were boys (50%). The demographic characteristics of infants are summarized in Table 1.
| Variables | Values |
|---|---|
| Qualitative Variables | |
| Sex | |
| Male | 45 (50) |
| Female | 45 (50) |
| Underlying diseases | |
| Gastrointestinal | 33 (36.7) |
| Craniofacial anomalies | 2 (2.2) |
| Orthopedic | 1 (1.1) |
| Nephrologic | 1 (1.1) |
| Uorologic | 3 (3.3) |
| Dermatologic | 1 (1.1) |
| Birth trauma | 1 (1.1) |
| Respiratory | 15 (16.7) |
| Neurosurgery | 1 (1.1) |
| Neurologic | 10 (11.1) |
| Infectious | 9 (10) |
| Cardiac | 5 (5.6) |
| Limb gangrene | 1 (1.1) |
| Metabolic | 7 (7.8) |
| Indication of insertion | |
| TPNA | 48 (53.3) |
| IVB therapy | 6 (6.7) |
| Anti-convulsant therapy IV | 13 (14.4) |
| Antibiotic therapy IV | 13 (14.4) |
| Low weight | 8 (8.9) |
| Low Blood sugar | 1 (1.1) |
| Anticoagulant therapy IV | 1 (1.1) |
| Location of insertion | |
| Right upper limb | 27 (30) |
| Left upper limb | 15 (16.7) |
| Right lower limb | 10 (11.1) |
| Left lower limb | 11(12.2) |
| Left temporal | 12 (13.3) |
| Right temporal | 9 (10) |
| Right auricular | 3 (3.3) |
| Ultrasound report | |
| Right place | 71 (78.9) |
| Midline | 16 (17.8) |
| Malposition | 3 (3.3) |
| Quantitative Variables | |
| Chronological age, wk | 26.71 ± 25.6 |
| Gestational age, wk | 35.58 ± 3.29 |
| Weight, g | 2576.94 ± 725.27 |
Demographic Characteristics of Studied Infantsa
Radiography results indicated correct PICC placement in 73 infants (81.1%), which was confirmed by sonography in 71 infants (78.9%). Sonography results indicated inappropriate placement in 19 infants (21.1%), whereas radiography showed that 17 infants (18.9%) had inappropriate placement of the PICC. Ultrasound had a sensitivity of 100%, specificity of 89.5%, PPV of 97.3% and NPV of 100% (P = 0.0001, correlation = 0.933, Kappa = 0.931). The end of the tip in one infant was identified to be inside the right atrium on radiography and located behind the tricuspid valve on the ultrasound. In another infant, radiography showed correct placement of the tip inside the inferior vena cava (IVC), whereas ultrasound showed that the tip had entered the left atrium from right atrium through the patent foramen ovale (PFO).
Correlation of ultrasound results with radiography, as the gold standard, was 97.8%. This correlation was examined in smaller subgroups of different variables and it was determined that the correlation of the two tests was not related to sex, gestational age, chronological age, PICC location, need for surgery, and catheterization indication. In general, no significant correlation existed between the consistencies of these methods with the underlying variables.
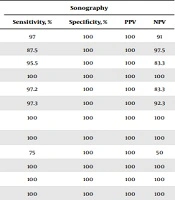
A comparison of both tests based on the catheter placement (correct, incorrect, midline) showed that the results matched (P = 0.0001, correlation = 0.900, kappa = 0.932). Table 2 compares the results of the catheter placement in both tests based on the variables and the sensitivity, specificity, PPV, and NPV of the ultrasound for each variable.
| Variable | No. of Correct Place Radio | No. of Correct Place USb | No. of Incorrect Place Radio | No. of Incorrect Place US | Correlation Two Tests | P Value | Sonography | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity, % | Specificity, % | PPV | NPV | |||||||
| Male | 35 | 34 | 10 | 10 | 0.940 | 0.0001 | 97 | 100 | 100 | 91 |
| Female | 38 | 37 | 7 | 7 | 0.923 | 0.0001 | 87.5 | 100 | 100 | 97.5 |
| Preterm | 44 | 42 | 10 | 10 | 0.892 | 0.0001 | 95.5 | 100 | 100 | 83.3 |
| Term | 29 | 29 | 7 | 7 | 1.000 | < 0.0001 | 100 | 100 | 100 | 100 |
| BW a < 2500 g | 36 | 35 | 5 | 5 | 0.900 | 0.0001 | 97.2 | 100 | 100 | 83.3 |
| BW > 2500 g | 37 | 36 | 12 | 12 | 0.948 | 0.0001 | 97.3 | 100 | 100 | 92.3 |
| Right upper limbs | 22 | 22 | 5 | 5 | 1.000 | < 0.0001 | 100 | 100 | 100 | 100 |
| Left upper limbs | 13 | 13 | 2 | 2 | 1.000 | < 0.0001 | 100 | 100 | 100 | 100 |
| Right lower limbs | 8 | 6 | 2 | 2 | 0.612 | 0.053 | 75 | 100 | 100 | 50 |
| Left lower limbs | 9 | 9 | 2 | 2 | 1.000 | < 0.0001 | 100 | 100 | 100 | 100 |
| Right temporal | 6 | 6 | 3 | 3 | 1.000 | 0.003 | 100 | 100 | 100 | 100 |
| Left temporal | 10 | 10 | 2 | 2 | 1.000 | < 0.0001 | 100 | 100 | 100 | 100 |
The Comparison of the Results of the Catheter Placement in the Radiography and Ultrasound Based on Different Variables and the Sensitivity, Specificity, PPV, and NPV Positive of the Ultrasounda
In general, no significant correlation existed between the consistency of these methods with the underlying variables including gender, gestational age, chronological age, catheter embedding location, embedding indication, underlying disease, and need for surgery. The ultrasound had good sensitivity, specificity, PPV, and NPV.
5. Discussion
In the present study we examined 90 infants, 45 (50%) females and 45 (50%) males. The results of the ultrasound compared to radiography as the gold standard for evaluation of the PICC tip had a sensitivity of 100% and specificity of 89.5%. The ultrasound, with a PPV of 97.3% and NPV of 100%, showed good diagnostic capabilities. In line with these results, a similar study conducted by Telang et al. (12) estimated the sensitivity (96.55%), specificity (100%), PPV (100%), and NPV (75%) of RTUS.
In 2006, Lanza et al. (13) conducted a study in Italy on neonates that had an average age of 31.7 days. They reported that the B-mode and Doppler ultrasounds had an 84.6% sensitivity and 100% specificity. The reported NPV value was 97.9% and PPV was 100%. They reported a correlation between ultrasound and chest radiography of 98.1%, which was relatively consistent with the results of our study.
Another study evaluated the catheter pathway by ultrasound in 61 umbilical cord catheters in 60 infants and compared the results with radiography. They reported a sensitivity of 96.4% and specificity of 93.9% for ultrasound, and a sensitivity of 92.8% and specificity of 78.8% for radiography. Ultrasound had a sensitivity of 93.3% and specificity of 95.6% for determining the position of the tip of the catheter, whereas radiography had a sensitivity of 66.7% and specificity of 63% (P < 0.001). Radiographic dysfunction increased in determining the position of the tip of the umbilical cord catheter with increased birth weight (P < 0.005). Their results showed that radiography was reliable in determining the path of the umbilical cord catheter (central or otherwise), but the ultrasound method had a higher priority in determining the position of the tip of the umbilical cord catheter compared to radiography (14). These findings were in line with their study results.
In the present study, 81.1% of the PICC placements were identified as appropriate by radiography and 78.9% were confirmed by ultrasound. On the other hand, radiography detected 17 (18.8%) cases of inappropriate placement, whereas ultrasound detected 19 (21.1%) cases of inappropriate placement. The findings indicated that ultrasound was more accurate than radiography in determining the PICC placement. These findings were similar to the results of a study by Karber et al. (15).
Ultrasound assessments after catheter implantation have been shown to identify the depth of the catheter placement points in the heart and portal system. However, radiography has not been able to do this properly (16, 17). Results of previous studies have indicated that ultrasound can minimize the potential side effects of improper catheter placement and reduce the need for radiography reassessment (18, 19), which was confirmed in the present study.
The practical and beneficial role of sonography during catheter implantation as a guide in neonatal intensive care has been investigated, and it appears that ultrasound examination can be performed even on premature infants (20, 21).
In our study, the consistency between the results of radiographic and ultrasound was independent of the underlying variables of sex, gestational age, chronological age, catheter embedding location, embedding indication, underlying disease, and need for surgery. Similar studies have also reported that the results of the two tests are independent of the underlying variables (11, 12, 22, 23).
Ultrasound sensitivity in the present evaluation was 100%, with a specificity of 89.5%, PPV of 97.3%, and NPV of 100%. Saul et al reported both the sensitivity and specificity of ultrasound as 100% (24).
At present, radiography is mentioned as the standard gold method in diagnosing the end of PICC catheter in books and articles, and this method is used routinely in most centers. However, the disadvantages of radiography include the following: exposure of the baby to radiation; in case of malposition and correction, need for re-graphing and re-imposition of radiation; sometimes AP and LAT imaging is needed to determine the location of the catheter; creating a static image that requires a proper position on the baby’s torso and limbs is difficult in practice; risks of cumulative radiation dose in patients, staff and other patients present at the NICU due to its bedside. It is now inclined to gradually replace chest radiographs with repeated radiographs in the diagnosis of neonatal respiratory diseases (1). In this regard, in order to see the end of the catheter, small portable ultrasound devices have been considered for this purpose in the present study.
Advantages of the present study included the larger sample size compared to most of the similar studies. The study conducted by Tauzin et al. (19) evaluated a series of 109 cases, which was more than that in the current study. Also, our study was performed on 1 and 2 French silicone PICC catheters, which are difficult to visualize with sonography because of their small size. Most studies examined umbilical artery catheters (UAC) and umbilical venous catheters (UVC), which are larger than the PICC (25-32). In addition, there were no observed side effects in the 90 studied infants. However, we conducted this study on one population over a limited period of time and in one center, which was a limitation of this study. Future studies that enroll more patients and in several centers are recommended.
5.1. Conclusions
This study showed that the ultrasound had good PPV and NPV in determining the location of the tip of the PICC catheter. Ultrasound appears to be a suitable bedside tool for identifying PICC placement and can prevent babies from exposure to additional X-rays. However, multi-center studies with larger sample sizes need to be conducted.