1. Background
The World Health Organization (WHO) declared coronavirus outbreak a global pandemic on 11th March 2020 (1). The first children's coronavirus cases were reported in Wuhan, the epicenter of COVID-19, showing mild respiratory symptoms and fever with positive SARS-CoV-2 RNA in nasopharyngeal/throat swabs (2, 3). However, the first report from United Kingdom (UK) introduced shared clinical manifestations of the new syndrome with other critical syndromes, such as toxic shock syndrome (TSS), atypical Kawasaki disease (KD), Kawasaki disease shock syndrome (KDSS), and secondary hemophagocytic lymphohistiocytosis (HLH) with antibody SARS-CoV-2 positive (4). This was followed by reports from Italy (5) and Switzerland (6). Thus, on 14th May, the United States Centers for Disease Control and Prevention (CDC) named multisystem inflammatory syndrome in children (MIS-C) on these manifestations of SARS-CoV-2 in children (7).
Children have been associated with the early phase of the virus replication with positive SARS-CoV-2 RNA of nasopharyngeal involvement with mild symptoms and delayed phase of inflammation and immune dysregulation with seropositive SARS-CoV-2 due to MIS-C (4, 5, 8-10).
In Iran, especially at the second peak, several patients and consultations with KD and/or MIS-C, according to CDC criteria, were referred to our hospital. Hence, this kind of approach to patients with MIS-C in the Tehran Children’s Medical Center, (affiliated to Tehran University of Medical Sciences) is confirmed and advised by pediatric rheumatologists, pediatric infectious disease specialists, and pediatric cardiologists. According to this experience, we have some research and report on a different aspect of MIS-C recently (11, 12).
2. Kawasaki Disease and Kawasaki-Like Diseases
Kawasaki disease (KD) is an inflammatory disease that damages mucous membranes (eyes, lips and oral mucosa), skin (rashes), lymph nodes, and medium-sized vessels (vasculitis, specially coronary arteries) (13). Nowadays, similar clinical manifestations of KD and MIS-C have attracted the attention of clinicians to a higher prevalence of Asian vasculitis.
The seasonal incidence of viral infection and Kawasaki disease suggests the viral trigger factor of the immune system to be involved in KD.
The seasonal incidence of viral infection and KD led to the speculation that viral infection may be a trigger factor of the immune system in KD (14). The association of SARS-COV1 and KD was described (15). However, this theory has not been accepted by subsequent studies. A 30-fold increased incidence of KD after the COVID-19 pandemic compared to the same period in the last five years in the Italian literature may confirm the triggering role of SARS-CoV-2 in KD patients with higher affinity than SARS-CoV1 (5). Thus, the first complete KD with positive SARS-CoV-2 RNA-PCR was reported with a significant response to intravenous immunoglobulin (IVIg) treatment without MIS-C presentations (16).
Kawasaki disease shock syndrome (KDSS) is one of the severe manifestations of KD (1% - 5%) with decreased ejection fraction (EF), thrombocytopenia, anemia, and increased inflammatory laboratory data (ESR, CRP). KDSS patients were older, with more coronary involvement and IVIg resistance (17).
In the acute phase of KD as a hyper-inflammatory condition, the levels of cytokines, such as TNF, IL6, IL1β, IL17, and GCS-F are increased. In IVIg- resistant KD patients, IL6 and IL10 levels are higher with more coronary involvement than IVIg-responsive KD patients (18) Thus, increased levels of IL6, IL10, and interferon-gamma (IFN‐γ) were reported in IVIG-resistant KDSS patients (17). Hence, MIS-C patients may be resistant to IVIg treatment.
IVIg is prepared from the serum of 1000 - 15000 blood donors. IVIg targets both innate and adaptive immune systems. The endocytosis of macrophages and dendritic cells is inhibited by blocking the activation of the immune complex. Thus, it would be helpful in the early phase of the inflammatory cascade. In contrast, due to high concentrations and increased plasma viscosity should be dealt with the volume overload and thrombotic events, especially in cardiogenic shock (CS) and hyper-coagulative states, such as KDSS and MIS-C (19).
To the best of our knowledge, there are two aspects of COVID-19 KD in childhood nowadays:
First, at a younger age (less than five years old), the results of the SARS-CoV-2 PCR-RNA become more positive than antibody test in patients with complete or incomplete KD (according to AHA criteria) and this group is responder to IVIg treatment (IVIg-responsive patients).
Second, at an older age (older than five years), patients with incomplete KD criteria or Kawasaki-like disease resembling KDSS exhibit higher coronary and valvular involvement. In this group, antibodies become more positive than SARS-CoV-2 PCR-RNA and do not respond to IVIg treatment (non-IVIg-responsive patients) (8, 9).
3. Cytokine Storm and MISC
Macrophage activation syndrome (MAS) or secondary hemophagocytic lymphohistiocytosis (HLH) is a cytokine storm phenomenon arising from malignancies, rheumatic disorders, or viral infections. The dysregulation of NK cells and cytolytic CD8 T cells (CTL) lead to inherited or acquired antigen-presenting activation and INF-y. TNFα secretion, on the other hand, causes the recruitment of other inflammatory cells, such as neutrophils and lymphocytes, leading to increased secretion of cytokines and activation of macrophages, along with the production of pro-inflammatory cytokines, TNF-α, IL-6, IL-1, IL-18, and hemostatic tissue factor (TF). The activated macrophages exhibit HLH and hyperferritinemia. This cycle continues until a cytokine storm occurs ultimately (20).
The same pathway may be taken in a cytokine storm, or MIS-C phenomenon of SARS-CoV-2 as a secondary HLH triggered by a viral infection with antibody-mediated stimulation (21, 22). Secondary HLH, like the primary HLH, may occur with a fundamental role of a genetic disorder (23). Therefore, it may be a response to the question why the first MIS-C reports were from European children of specific races as opposed to Asian children with higher susceptibility to KD and the source of SARS-CoV-2 from this population.
MAS is a life-threatening condition, which requires prompt evaluation and treatment. Due to the highly increased cytokines, the antagonists of key cytokines, such as anti-IL1, anti-IL6, and INF, were administered and evaluated in the treatment of the cytokine storm phenomena (24). Although there is no consensus and evidence on efficacy of pulsed intravenous methylprednisolone (IVMP), rapid resolution of hypercoagulable state and critical response to MAS with suppression of activated macrophages lead to administration of IV pulses of methylprednisolone in one to three doses (25-27). Indeed, the economic state and availability of medicine in the immediate therapeutic intervention should be noticed.
In the recent pandemic state, corticosteroids in patients with MIS-C are prescribed and yield good results (8, 9, 11, 12, 28), Therefore, the majority of MIS-C patients are SARS-CoV-2 PCR-RNA negative accompanied by SARS-CoV-2 antibody positive with delayed presentation, leading to conducting clinical trials to suppress the inflammatory response process rather than virus suppression.
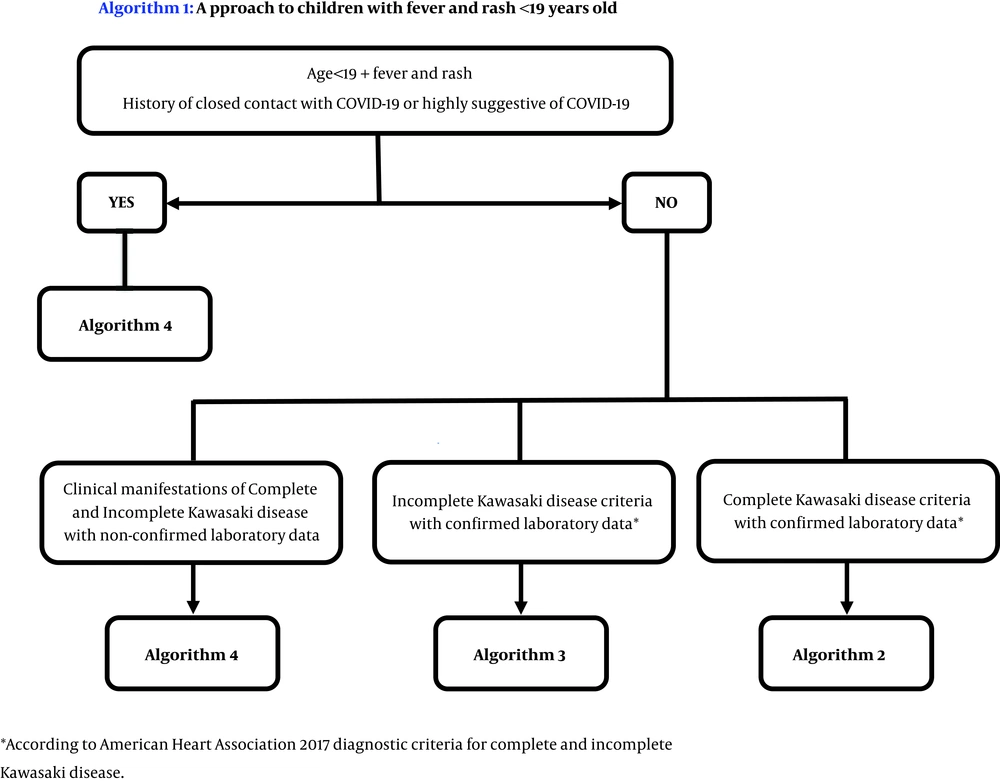
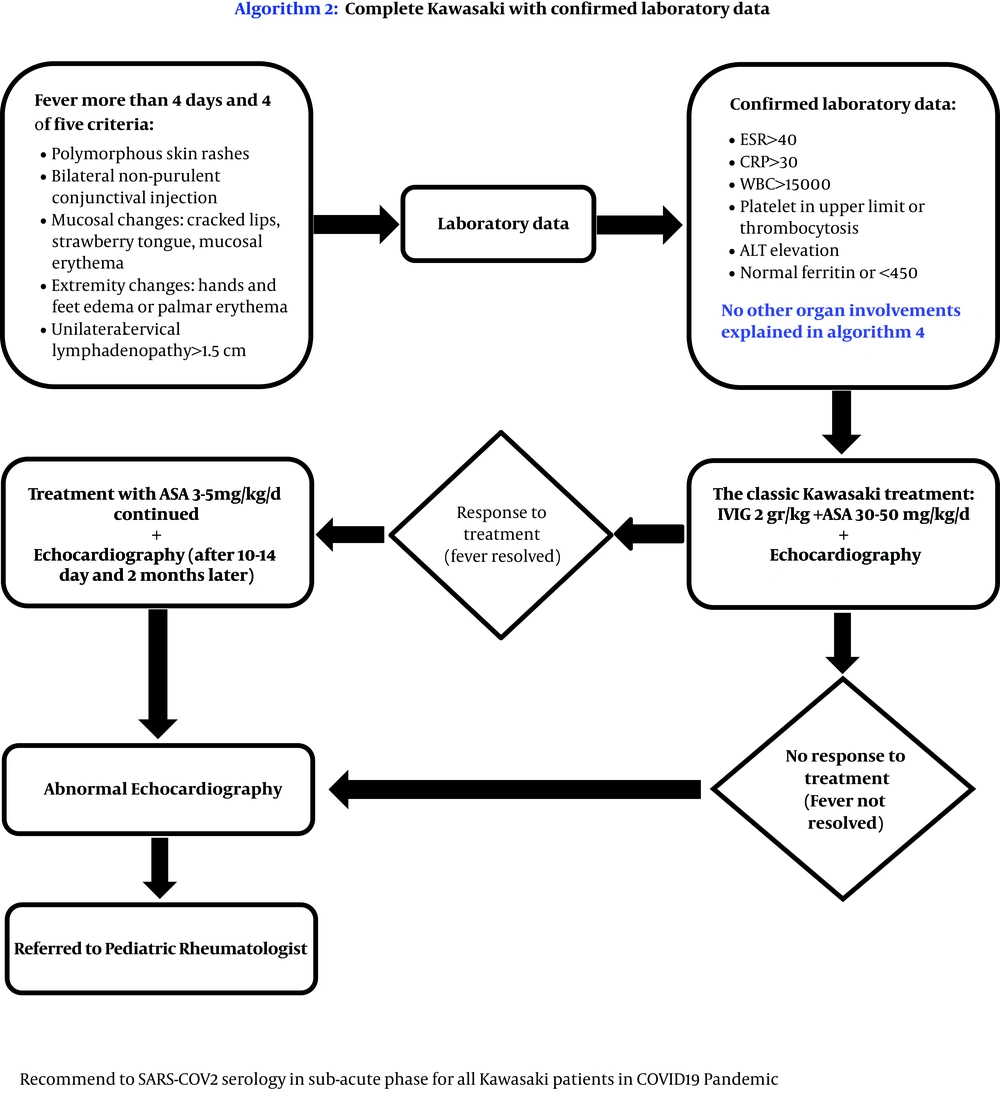
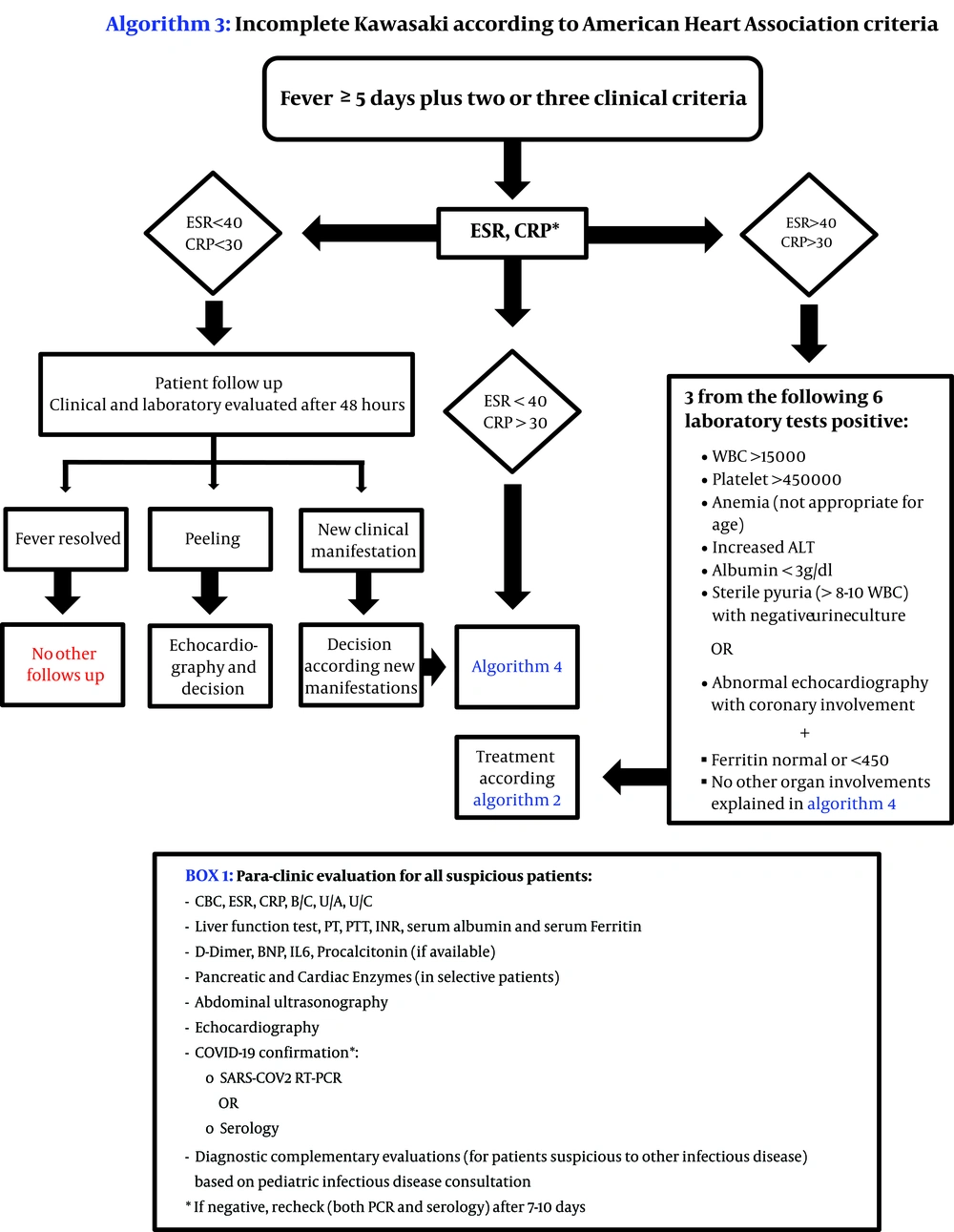
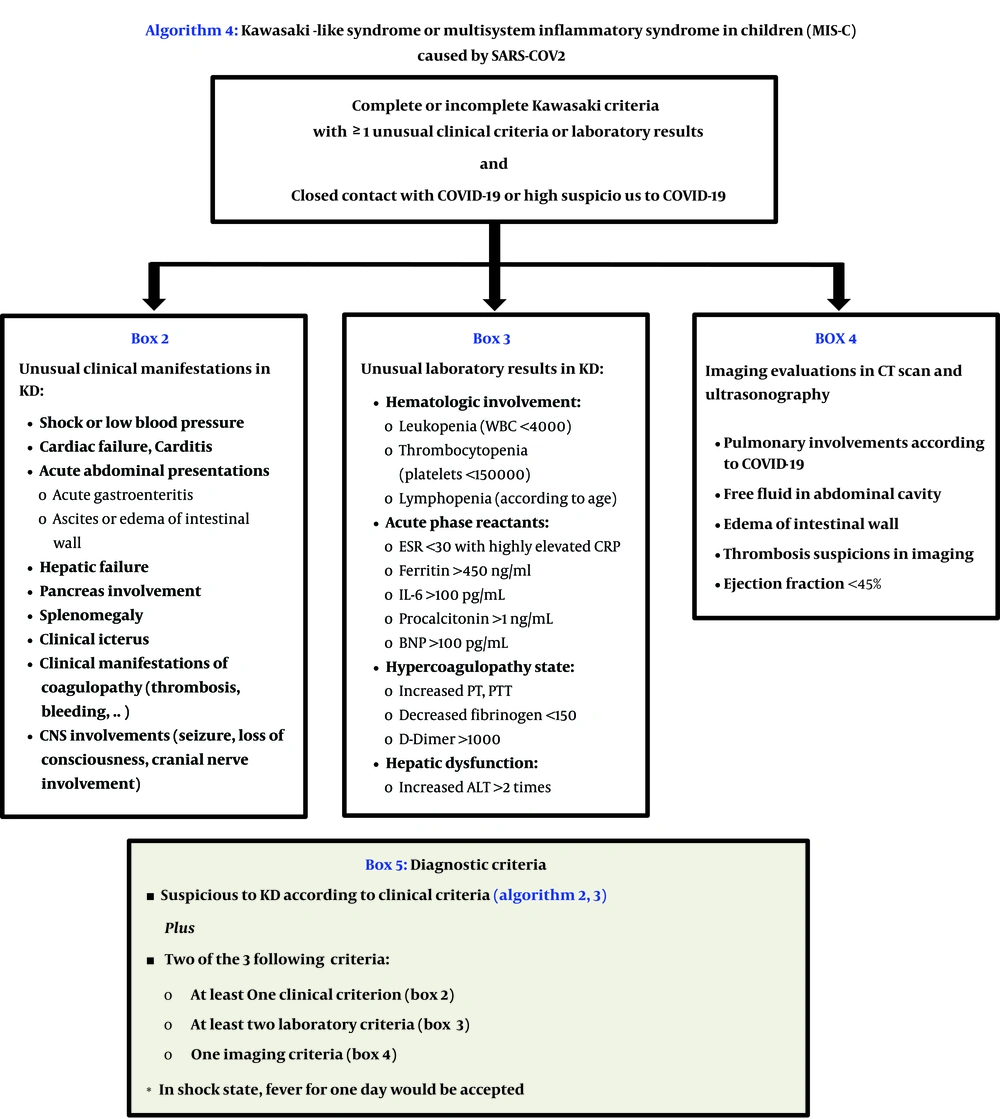
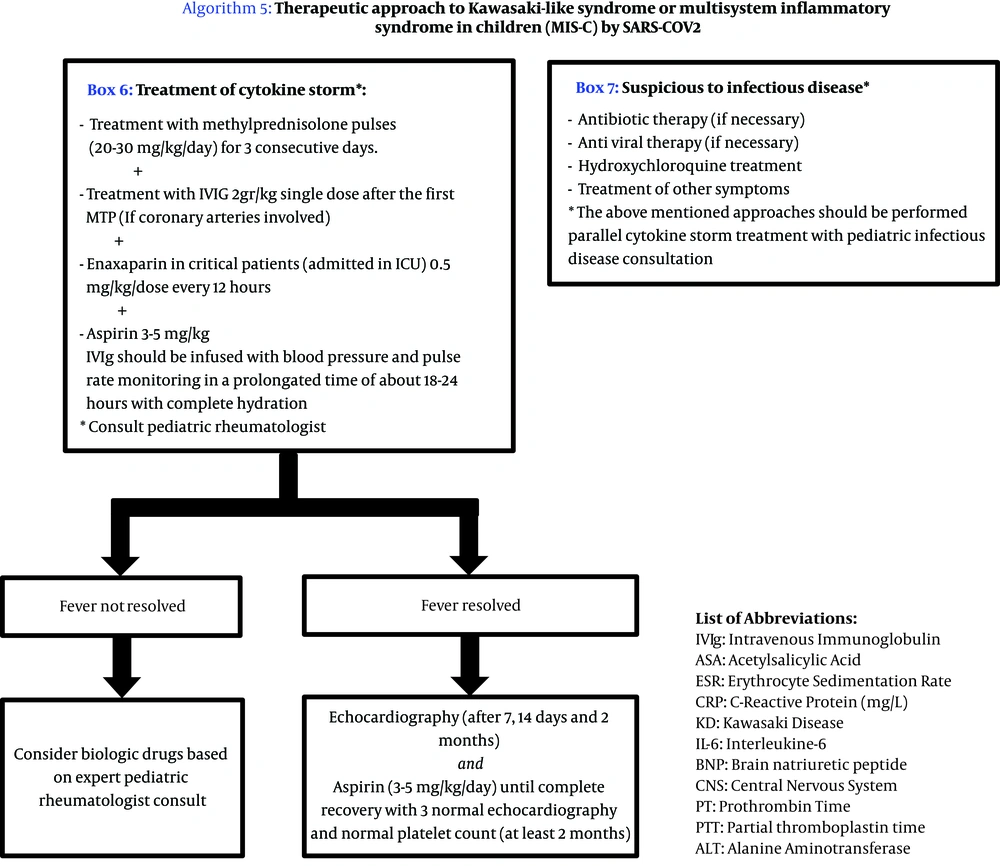
Tehran Children’s Medical Center, Pediatrics Center of Excellence in Iran as a tertiary pediatric referral center has been encountered with more than 50 MIS-C cases during 3 months. So, all relative departments including rheumatology, infectious disease, intensive care, cardiology and emergency departments were involved in designing an algorithmic approach for diagnosis and treatment of children suspicious to MIS-C and Kawasaki like disease following COVID-19. This approach is presented in this report. Based on this approach we diagnosed all patients as soon as possible and treated all suspected children without any mortality or morbidity (Figures 1-5).
Approach to Kawasaki-like syndromes in pandemic COVID-19: The Tehran Children’s Medical Center Protocol (algorithm 1); designed by Pediatric Rheumatology Department confirmed by Pediatric Infectious Diseases, Pediatric Intensive Care, Pediatric Cardiology, and Pediatric Emergency Departments.
Approach to Kawasaki-like syndromes in pandemic COVID-19: The Tehran Children’s Medical Center Protocol (algorithm 2); designed by Pediatric Rheumatology Department confirmed by Pediatric Infectious Diseases, Pediatric Intensive Care, Pediatric Cardiology, and Pediatric Emergency Departments.
Approach to Kawasaki-like syndromes in pandemic COVID-19: The Tehran Children’s Medical Center Protocol (algorithm 3); designed by Pediatric Rheumatology Department confirmed by Pediatric Infectious Diseases, Pediatric Intensive Care, Pediatric Cardiology, and Pediatric Emergency Departments.
Approach to Kawasaki-like syndromes in pandemic COVID-19: The Tehran Children’s Medical Center Protocol (algorithm 4); designed by Pediatric Rheumatology Department confirmed by Pediatric Infectious Diseases, Pediatric Intensive Care, Pediatric Cardiology, and Pediatric Emergency Departments.
Approach to Kawasaki-like syndromes in pandemic COVID-19: The Tehran Children’s Medical Center Protocol (algorithm 5); designed by Pediatric Rheumatology Department confirmed by Pediatric Infectious Diseases, Pediatric Intensive Care, Pediatric Cardiology, and Pediatric Emergency Departments.