Dear Editor,
The relation of Henoch-Schonlein purpura (HSP) vasculitis with Acute rheumatic fever was defined by Gairdner firstly in 1948 (1). Both HSP and rheumatic fever can affect the joints and heart in a different way. In HSP artritis is usually non migratory and heart involvement is usually appear as myocarditis. In rheumatic fever artritis is usually migratory and heart involvement is manifest as valvulitis. Rheumatic fever may rarely develop during HSP. The role of group A beta-haemolytic streptococcus (GABHS) in the pathogenesis of rheumatic fever is well established. The presence of rheumatic fever, GABHS may sometimes have a pathogenic role in HSP (2). We present here a child admitted to our clinic as acute rheumatic carditis, who developed HSP vasculitis thereafter.
A 12- year-old male presented to our clinic with initially right ankle,followed by left knee and left ankle, pain, sensitivity, redness. His complaints had started 4 days ago. We learned that he had an upper respiratory infection 15 days ago and used antibiotic. At the time of admission axillary body temperature was 36.7°C; blood pressure was 90/60 mmHg. Erythema marginatum-like eruptions appeared on his body and upper extremities, which regressed within 1 hour during follow-up (Figure 1).
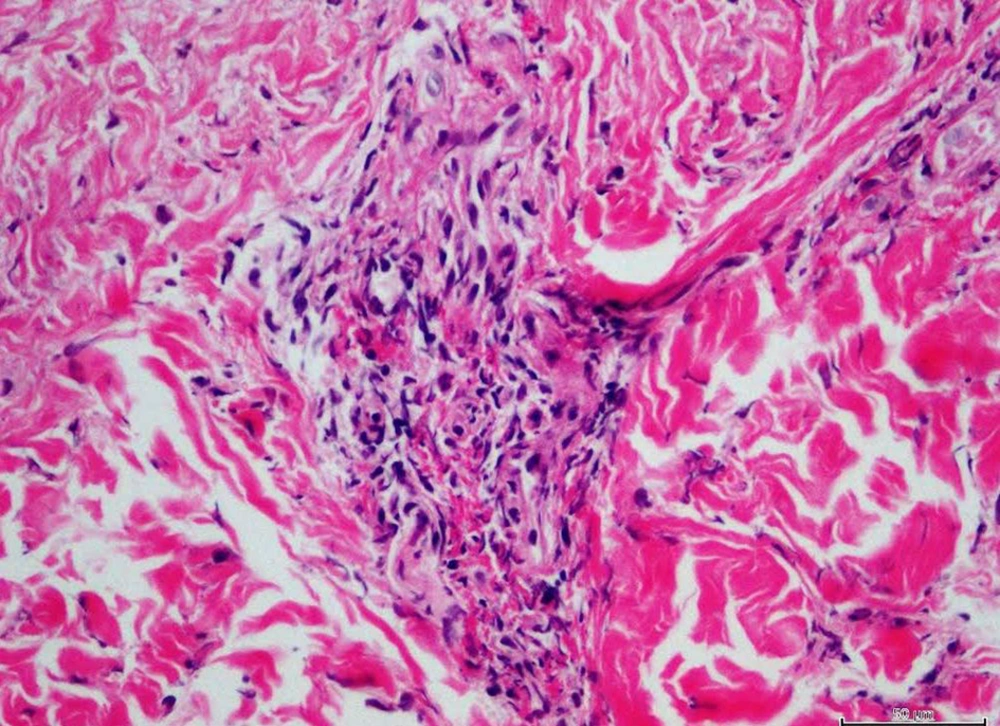
A cardiac auscultation revealed a grade 2/6 systolic murmur over the mitral region. He had hyperemia and swelled on the left knee and right leg, a pronounced diameter difference between the two ankles. Laboratory investigation showed hemoglobin 11.2 g/dL, WBC count 7.6 × 109/L, platelet count 283 × 109/L, C-reactive protein was elevated 79.9 mg/dL, erythrocyte sedimentation rate was elevated, 80 mm/hour. Antistreptolysin (ASO) titer was 180 Todd Units on admission. ASO was elevated 320 Todd Units during follow-up. The throat culture was negative. Antinuclear antibody was absent, rheumatoid factor was negative. Electrocardiography revealed a PR interval of 0.20 seconds. Echocardiographic findings revealed minimal mitral, aortic, and tricuspid valve failure. The patient was diagnosed with ARF carditis, and treatment was started with 2 mg/kg/day prednisolone. Benzathine penicillin made intramuscular. During the second day of hospitalization patient developed purpuric rush on his lower ekstremities. Purpuric rush, did not become pale with pressure. The skin biopsy revealed leucocytoclastic vasculitis (Henoch-Schönlein purpura) (Figure 2).
His serum immune globulin A (IgA) level was elevated 324 mg/dL. Therefore, the steroid treatment was continued. During follow-up the signs and symptoms of vasculitis and carditis regressed.
Our patient had migratory artritis. According to the Jones criteria, our case had three major diagnostic symptoms of rheumatic fever; arthritis, carditis, and erythema marginatum; therefore, a diagnosis of acute rheumatic fever was made. ASO, which is a supporting parameter of diasease, was also high in our case. Ocal et al. (3) reported a case of HSP with rheumatic carditis with history of streptococcal infection 4 weeks ago. Our patient had history of upper respiratory infection before 2 weeks ago. Our case’s throat culture was negative for GABHS, but he used antibiotic. Elevated ASO titers suggested a recent streptococcus infection.
Immunologic mechanism underlying HSP and rheumatic fever are quite different. Celluler immune mechanism mediated by T lymphocytes to streptococcal M-proteins cause destruction cardiac tissues (4). In these patients elevated IgA levels and immune complexes have been described (5).
In previous reports during to HSP, developed acute rheumatic carditis thereafter (1, 3, 6). He is different from previous cases. In literature, the interval from onset of HSP to appearance of rheumatic fever was declared as 10 days to 12 weeks (2, 3, 6). Literatures are limited of HSP and acute rheumatic fever co-occurrence without time interval between these two diseases (6, 7). We presented this case due to that rheumatic fever appeared first, after 2 days purpuric rash occurred. Because of these two reasons our case is different from previous reports. We think that GABHS infections may trigger HSP as acute rheumatic fever.