Fulltext
Hyperbilirubinemia is a common and in most cases benign clinical condition in neonates. Phototherapy is used for management of neonatal hyperbilirubinemia[1]. Phototherapy may lead to complications including skin rash, diarrhea, hyperthermia, chills, dehydration, DNA damage to lymphocytes, retinal degeneration, bronze baby syndrome especially in cholestatic jaundice and PDA opening in LBWs and Hypocalcemia[2].
A cross sectional study was performed on 147 icteric neonates managed with phototherapy in Bahrami Hospital in Tehran from 2008 to 2009. Phototherapy was provided with four blue light fluorescent lamps (Phillips) placed at 20 cm distance from newborns. Neonates with any underlying disease or risk factors of hypocalcemia were excluded. Serum calcium and bilirubins were measured on arrival and 48 hours after phototherapy. We considered hypocalcemia as a total serum calcium of <8 mg/dl. Demographic data, bilirubin and calcium levels were recorded and analyzed by ANOVA, Banferroni and Chi-square tests. P value <0.05 was considered as significant. The study was approved by Ethics Committee of Tehran University of Medical Sciences. A written informed consent was taken from one of the parents prior to enrollment after explaining the study.
The study was done on 147 term infants (73 females, 74 males). The mean±SD chronological age and time of jaundice appearance was 6±3 days and 3±2days respectively. The mean±SD weight was 3182±430 gram and mean±SD serum bilirubin level was 20.1±3.3 mg/dl in admission.
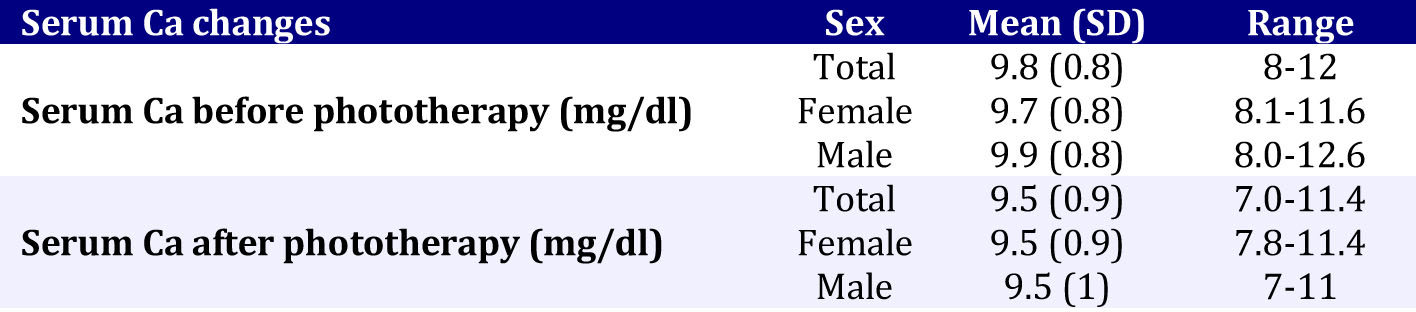
The mean±SD serum calcium level in admission and 48 hours after phototherapy were 9.8±0.8 and 9.5±0.9 mg/dl respectively (Table 1). Eighty-three (56%) babies had decrease in serum calcium level. Only ten (7%) newborns (4.2% females, 10.4% males) developed hypocalcemia after 48 hours of phototherapy. There was a significant difference between serum calcium level before and after phototherapy (P=0.03).
Romagnoli[3] was the first to suggest the association of hypocalcaemia and phototherapy in preterms. Hakinson[4] and Hunter[5] hypothesized that phototherapy inhibits pineal secretion of melatonin which blocks the effect of cortisol on bone calcium. So cortisol increases bone uptake of calcium and induces hypocalcaemia. Kim[6] suggested decreased secretion of parathormone as the cause of hypocalcemia. In Hooman’s study the urinary calcium excretion was significantly higher in phototherapy group[7].
Yadav[8] observed that 66% of term and 80% of preterms developed hypocalcemia after phototherapy. The prevalence of hypocalcemia in Jain’s study[9] was 30% in full term neonates and in Ehsanipoor’s 15%[10]. In our study 83 (56%) newborns had decline in serum calcium level, and only 7% had hypocalcaemia like Karamifar’s study (8.7%)[11]. In Jain’s study the frequency of hypocalcemia was higher in patients with high level of serum bilirubin.
In Eghbalian’s study, one of hypocalcemic newborns had apnea[12]. In Yadav’s study 80% of hypocalcemic term neonates became symptomatic, the most common sign was jitteriness[8]. In Karamifar’s study, none of the
Table 1: Serum calcium before and after phototherapy
patients developed symptoms similar to our findings[11].
In conclusion it is suggested that calcium level be assessed in newborns treated with phototherapy for 48 hrs or more and managed accordingly. It seems that prevalence of phototherapy associated hypocalcemia is not so high and we recommend further and larger studies for estimation of this prevalence rate.