Voriconazole is a triazole antifungal medication with expanded antifungal activity including Aspergillus spp. (1, 2). Therapeutic drug monitoring (TDM) is necessary for all pediatric patients receiving voriconazole due to various reasons including pharmacokinetic variability and CYP2C19 gene polymorphisms (1-3). Steady-state trough blood concentration should be monitored with target level of 1 - 5.5 mcg/mL (2 - 5.5 mcg/mL preferably) (1, 2). The time to obtain the initial blood sample is after four to seven days of treatment. When a loading dose is given, it can be taken on the third day of treatment (not earlier than immediately before the fifth dose) (1-3). This time period also encompasses the switch from oral to intravenous voriconazole (4). Repeated TDM is mandatory when adjusting the dosage, a change in clinical condition or route of administration, poor response, adverse drug reaction, and drug-drug or drug-food interactions (1, 3).
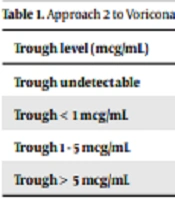
However, limited guidelines are available on how to adjust voriconazole dose based on therapeutic trough levels in pediatrics (1). Here, we provide five approaches to adjust the dose based on trough levels grounded on a literature review, including three children approaches and two adult approaches to provide a comparison and guide to TDM. The first approach is the one provided in the voriconazole pediatric monograph in UpToDate (5). Regarding intravenous voriconazole dose, the adjustment in the pediatric monograph in UpToDate for inadequate response increments of 1 mg/kg/dose has been mentioned for children ≥ 2 years and adolescents < 15 years weighting < 50 kg, as well as children ≥ 12 years and adolescents < 15 years weighting ≥ 50 kg and adolescents ≥ 15 years (regardless of weight). For patients unable to tolerate treatment, 1 mg/kg/dose reduction has been proposed in the above-mentioned age and weight groups (5). For oral voriconazole, different adjustments have been mentioned according to the age and weight of the patient (5). The second approach was provided by John et al. Table 1 illustrates the approach suggested by John et al. (1). The third approach, which is shown in Table 2, is the one utilized by Kang et al. in children (6). The fourth approach illuminates one provided by the Chinese Pharmacological Society in adults (3). In this approach, with trough level < 0.5 mcg/ml or poor clinical response, the maintenance dosage should be increased by 50%, followed by repeat TDM. If the trough level is within 5 - 10 mcg/mL without grade 2 adverse drug reactions (ADR), the maintenance dose should be decreased by 20% with a repeat TDM. If the trough level is > 10 mcg/mL or grade 2 ADR presents, the dose should be skipped once, with the maintenance dose reduced by 50% with a repeat TDM. Approach 5 describes an adult approach suggested by John et al. (1). In this approach, with trough levels of 0.0 - 0.5 mcg/mL, the dose should be increased by 50%; with levels of 0.5 - 1 mcg/mL, the dose should be increased by 25% and the trough level should be checked again on day 5 of new regimen; with ≥ 1 to 6 levels, no change is needed if the patient is responding; with > 6 levels if the patient is asymptomatic, the dose should be decreased by 25%; with > 6 levels if there exist drug-related toxicities, one dose should be held and subsequent doses decreased by 50%. In the latter situation, if toxicity is not reversed, an alternative antifungal agent should be considered. Perreault et al. have also provided a voriconazole dose modification guideline in adults, which is not mentioned in this editorial (7).
| Trough level (mcg/mL) | Approach |
|---|---|
| Trough undetectable | Increase dose by 2 mg/kg |
| Trough < 1 mcg/mL | Increase dose by 1 mg/kg |
| Trough 1 - 5 mcg/mL | Continue current dose |
| Trough > 5 mcg/mL | Decrease dose by 1 mg/kg |
| Trough level (mcg/mL) | Approach |
|---|---|
| Below therapeutic range | Dosage increase by 20% |
| Slightly above 5.5 mcg/mL | Dosage decrease by 20% without skipping a dose |
| Extremely above therapeutic range | Skip the dose (or more depending on the decision of the clinician) and then decrease the following dosage by 20% |
The main difference in pediatrics and adults seems to be the more cautious dose adjustment of 1 - 2 mg/kg/dose in pediatrics compared to 20 - 50% dose adjustment in adults, which may be due to different pharmacokinetics in these age groups (1, 4). To be better compared, it should be noted that 1 - 2 mg/kg dose decrement during voriconazole dose adjustment in children means approximately 10 - 20% dose reduction, while, in adult patients, 20 - 50% dose reduction is recommended.
The clinical pharmacist and the pediatrician should incorporate all these approaches according to the patient’s clinical status and adjust the dose according to clinical judgment, as well as the mentioned guides. It should be noted that there is no guideline to specify dose adjustment of voriconazole in neonates. The approach to dose adjustment may be extrapolated from children, but needs to be confirmed in trials. It is noteworthy that the upper range of doses to achieve a therapeutic level in infants < 2 years and neonates is higher than that in older children and adolescents (5, 8).
Adverse effects of voriconazole include hepatotoxicity, transient vision changes, neurotoxicity, skin rash, and QT prolongation (1, 2). Hepatotoxicity and neurotoxicity, in particular, are associated with higher plasma concentrations of voriconazole (1, 2). It has been suggested that patients who are ultra-rapid or rapid metabolizers of CYP2C19 may benefit from an alternative antifungal agent (1) rather than voriconazole dose adjustment based on serum levels. This issue needs further studies to clarify the best therapeutic approach.
In conclusion, there are various methods for voriconazole dose adjustment in children. The treating team should integrate the clinical status of the patient with these methods and provide the best plan for the child. Further studies underscoring this issue in children and neonates and illuminating the best approach are required.