1. Background
Medication adherence is defined as “the extent to which a person’s behavior-taking medication, following a diet, and/or executing lifestyle changes corresponds with agreed recommendations from a health care provider” (1). Medication adherence is a dynamic and complex behavioral process and intensely affects the individual, social, and environmental factors (2). Non-adherence is associated with higher rates of morbidity and mortality and increased health care costs. Therefore, improving medication adherence is critical in the management of chronic diseases (3).
During the past decades, liver diseases have been increasing globally. Based on the global burden of disease, it has been shown that almost 5400 deaths due to cirrhosis and other chronic liver diseases occurred in Iran in 2017 (4). The major causes of liver diseases in Iranian children are biliary atresia, cryptogenic cirrhosis, autoimmune cirrhosis, and familial intrahepatic cholestasis (5). Chronic liver diseases can lead to ascites, infection, hepatorenal syndrome, hepatic encephalopathy, upper gastrointestinal bleeding, and carcinoma (6, 7).
Liver transplantation is a vital intervention for patients with liver failure. It increases the patients’ survival rate at 1, 5, and 10 years to 85%, 77%, and 71%, respectively, according to a multi-centric report in Iran (8). Pre-operational behaviors can affect both operation success and graft rejection during the following years. Medication non-adherence before liver transplantation is not unusual, happening in about 70% of patients, and is one of the major causes of preventable graft rejection (9).
Given that medication adherence is modifiable and has a significant role in transplantation success, it is crucial to recognize the predictors of non-adherence in patients (9). Medication adherence patterns differ among the age groups. Adolescents have lower rates of adherence to their medications than both younger children and adults. Moreover, non-adherence has been proved to correlate with lower socioeconomic status (10, 11). The number of medications, their rate of administration, side effects, and duration of therapy, which leads to a continually changing regimen in these patients, can all affect the rate of medication adherence (12, 13)
2. Objectives
Medication non-adherence is one of the most significant risk factors in transplant care; therefore, we investigated medication non-adherence and its determinants in children and adolescents who suffered from chronic liver diseases in the Shiraz transplant center.
3. Methods
3.1. Study Setting and Population
We conducted this cross-sectional study in Shiraz, Iran, from August 2018 to the end of August 2019. A total of 160 children selected through convenience sampling from the outpatient clinic with complete medical records and good cooperation were enrolled in this study. The patients were entered into the study after they were provided with an explanation about the survey, and they answered the questions willingly. The inclusion criteria were at least six months of diagnosis of chronic liver disease and taking the drug(s), the age of less than 20 years, and patients or their families ability to commute to the clinic. Because medication adherence was the core of the study, the patients who did not complete the 8-Item Morisky Medication Adherence Scale (MMAS-8) or their physician had stopped prescribing medicine were excluded.
Face-to-face interviews based on a data collection form and MMAS-8 were conducted. The data collection form included questions on demographic data, family income, insurance status, living status, and the history of using medications. The MMAS is a tool that evaluates medication adherence among patients with chronic disease. The MMAS contains 8 self-reported items with seven yes/no questions and one question scored on a 5-point Likert scale. The scores from completed questionnaires are categorized into “High” (score =8), “Medium” (score 6 to < 8), and “Low” (score < 6) adherence groups. The validity and reliability of the Persian version of MMAS-8 have been assessed (9, 14).
The study protocol was approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1398.144).
Data were presented as mean ± SD and number (percentage), for continuous and categorical variables, respectively. The chi-square test and analysis of variance (ANOVA) were used to test statistical differences between the three groups. The multiple logistic regression was used to find the influencing factors on adherence. All analyses were done using R Statistical Software v-3.5.1.
4. Results
A total of 160 children completed the questionnaires. Their age range was 1.33 - 20 years, with a mean age of 11.2 ± 4.4 years. The mean age at diagnosis was 6.6 ± 5.4 years (range 0 - 19 years). Also, 84 participants (52.5%) were female. The mean number of siblings was 1.82 ± 1.7. Among the children, 69 (43.7%) cases had elementary education. The majority of patients (142, 89.31%) reported living with both parents. Among all parents, only 10 cases (6.3%) were illiterate, 27 cases (17%) had elementary education, and 38 cases (23.9%) had secondary or high school education. More than half of the parents had a diploma (49, 30.82%) or university degrees (35, 22.01%). About a quarter of parents (34, 21.7%) were unemployed. A large number of patients had insurance coverage (152, 96.2%). Regarding the residence status, 100 (62.8%) patients reported living in urban areas. Most of the families (110, 70.9%) had monthly income below15,000,000 Rials (Table 1).
| Variable a | Adherence Level | P-Value | |||
|---|---|---|---|---|---|
| Total (N = 160) | High, N = 56 (35) | Medium, N = 38 (24) | Low, N = 66 (41) | ||
| Age (y) | 11.22 ± 4.42 | 10.58 ± 4.41 | 10.75 ± 3.93 | 12.06 ± 4.62 | 0.137 a |
| Age at diagnosis (y) | 6.61 ± 5.36 | 6.26 ± 5.50 | 5.91 ± 5.37 | 7.35 ± 5.22 | 0.215 b |
| Gender | 0.733 c | ||||
| Female | 84 (52.5) | 29 (51.79) | 22 (57.9) | 33 (50) | |
| Male | 76 (47.5) | 27 (48.21) | 16 (42.1) | 33 (50) | |
| No. of siblings | 1.82 ± 1.7 | 1.83 ± 1.89 | 1.6 ± 1.07 | 1.95± 1.83 | 0.770 b |
| Patients’ education level | 0.249 c | ||||
| Illiterate | 29 (18.35) | 14 (25.45) | 6 (15.79) | 9 (13.85) | |
| Elementary | 69 (43.67) | 26 (47.27) | 20 (52.63) | 23 (35.38) | |
| Middle school | 32 (20.25) | 8 (14.55) | 6 (15.79) | 18 (27.69) | |
| High school | 15 (9.50) | 5 (9.09) | 3 (7.89) | 7 (10.77) | |
| Diploma | 13 (8.23) | 2 (3.64) | 3 (7.89) | 8 (12.31) | |
| Living status | 0.109 c | ||||
| Living With both Parents | 142 (89.31) | 46(83.64) | 37 (97.37) | 59 (89.4) | |
| Living With one parent / other family members | 17 (10.69) | 9 (16.36) | 1 (2.63) | 7 (10.6) | |
| Parents’ job status | 0.340 c | ||||
| Both or One are employed | 123 (78.34) | 42 (75) | 33 (86.84) | 48 (76.19) | |
| Both are unemployed | 34 (21.66) | 14 (25) | 5 (13.16) | 15 (23.81) | |
| Parents’ education level | 0.048 c | ||||
| Illiterate | 10 (6.29) | 6 (10.72) | 0 (0) | 4 (6.16) | |
| Elementary | 27 (16.98) | 9 (16.07) | 5 (13.16) | 13 (20) | |
| Middle school / High school | 38 (23.90) | 19 (33.93) | 6 (15.79) | 13 (20) | |
| Diploma | 49 (30.82) | 11 (19.64) | 14 (36.84) | 24 (36.92) | |
| Higher education | 35 (22.01) | 11 (19.64) | 13 (34.21) | 11 (16.92) | |
| Insurance | 0.237 d | ||||
| Yes | 152 (96.20) | 50 (92.59) | 37 (97.37) | 65 (98.48) | |
| No | 6 (3.80) | 4 (7.41) | 1 (2.63) | 1 (1.52) | |
| Residency | 0.327 c | ||||
| Urban | 100 (65.79) | 31 (59.62) | 27 (75) | 42 (65.62) | |
| Rural | 52 (34.21) | 21 (40.38) | 9 (25) | 22 (34.38) | |
| Housing | 0.021 c | ||||
| Personal house (property) | 107 (66.88) | 42 (75) | 29 (76.32) | 36 (54.55) | |
| Personal house (leased) /Other | 53 (33.12) | 14 (25) | 9 (23.68) | 30 (45.45) | |
| Family monthly income | < 0.001 c | ||||
| ≤ 15000000 rials | 110 (70.97) | 42 (77.78) | 17 (45.95) | 51 (79.69) | |
| > 15000000 rials | 45 (29.03) | 12 (22.22) | 20 (54.05) | 13 (20.31) | |
| Traveling time to the center (min) | 444.82± 536.69 | 573.43± 554.93 | 270.83± 270.58 | 447.26± 610.52 | 0.020 b |
| Liver disease Causes | 0.057 d | ||||
| Non-viral hepatitis | 20 (15.62) | 4 (8.33) | 2 (6.90) | 14 (27.45) | |
| Biliary tract diseases/ hepatic vascular disease | 19 (14.84) | 7 (14.58) | 8 (27.59 | 4 (7.84) | |
| Cryptogenic cirrhosis | 37 (28.91) | 12 (25) | 10 (34.48) | 15 (29.41) | |
| Inherited diseases | 45 (35.16) | 21 (43.75) | 8 (27.59) | 16 (31.37) | |
| Tumors/ other | 7 (5.47) | 4 (8.33) | 1 (3.45) | 2 (3.92) | |
| Medical comorbidities | 0.781 c | ||||
| No comorbidity | 117 (73.12) | 40 (71.43) | 30 (78.95) | 47 (71.21) | |
| Contagious diseases | 10 (6.25) | 5 (8.93) | 2 (5.26) | 3 (4.55) | |
| Non-Contagious diseases | 15 (9.38) | 4 (7.14) | 4 (10.53) | 7 (10.61) | |
| Other | 18 (11.25) | 7 (12.5) | 2 (5.26) | 9 (13.64) | |
| Candidate for transplant | 0.140 c | ||||
| Yes | 29 (24.17) | 13 (33.33) | 4 (12.90) | 12 (24) | |
| No | 91 (75.83) | 26 (66.67) | 27 (87.10) | 38 (76) | |
| Taking medication | 0.673 d | ||||
| Patient | 37 (23.27) | 14 (25) | 10 (26.32) | 13 (20) | |
| Patient Family assistance | 18 (11.25) | 6 (10.71) | 2 (5.26) | 10 (15.38) | |
| Family assistance | 101 (63.52) | 34 (60.71) | 26 (68.42) | 41 (63.08) | |
| Staff assistance | 3 (1.89) | 2 (3.57) | 0 | 1 (1.54) | |
| Medication instruction | 0.403 c | ||||
| Yes | 117 (75.48) | 45 (83.33) | 28 (75.68) | 44 (68.75) | |
| No | 21 (13.55) | 5 (9.26) | 4 (10.81) | 12 (18.75) | |
| So-so | 17 (10.97) | 4 (7.41) | 5 (13.51) | 8 (12.50) | |
a Analysis of variance (ANOVA)
b Kruskal-Wallis test
c Chi-square test,
d Fisher exact test
The most prevalent underlying diseases were inherited disease (45, 35.2%), cryptogenic (37, 28.9%), non-viral hepatitis (20, 15.62%), biliary tract and vascular disease of the liver (19, 14.8%), and other diseases (7, 5.5%). Most of the patients (117, 73.1%) did not report comorbidities. The assistance in taking medication was as follows: children themselves (37, 23.3%), children and family (18, 11.3), only family (101, 63.52%), and caregivers (3, 1.9%). The medical staff provided the necessary drug instructions to 117 (75.5%) patients (Table 1).
The most commonly used drugs were multivitamin/mineral supplements (48.8%), medications to treat the complications of cirrhosis (34.1%), immunosuppression (9.5%), medication to treat liver disease (4.9%), and others (2.7%).
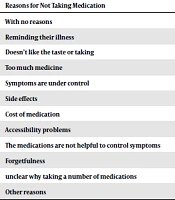
Responses showed that about 40% of patients forget sometimes to take medications; however, more than 60% of patients never/rarely had difficulty in remembering to take drugs (Table 2). According to the MMAS-8 questionnaire, the prevalence of high adherence to liver disease medication was 56 (35%). The prevalence of medium and low adherence levels was 38 (23.75%) and 66 (41.25%), respectively. The most important factors for non-adherence to medication in patients were forgetting (37, 23.13%), lack of access to medicines (21, 13.13%), feeling that their disease is under control (15, 9.38%), and cost (12, 7.5%) (Table 3).
| Item | No. (%) of Patients Who Answered Yes |
|---|---|
| Do you sometimes forget to take your liver disease medications? | 69 (43.13) |
| Over the past two weeks, were there any days when you did not take your liver disease medications? | 41 (25.63) |
| Have you ever cut back or stopped taking your medication without telling your doctor because you felt worse when you took it? | 28 (17.5) |
| When you travel or leave home, do you sometimes forget to bring along your medications? | 24 (15) |
| Did you take your liver disease medicine yesterday? | 35 (21.88) |
| When you feel like your liver disease is under control, do you sometimes stop taking your medicine? | 19 (11.88) |
| Do you ever feel hassled about sticking to your liver disease treatment plan? | 56 (35) |
| Reasons for Not Taking Medication | Yes Answered Frequencies, No. (%) |
|---|---|
| With no reasons | 9 (5.63) |
| Reminding their illness | 5 (3.13) |
| Doesn’t like the taste or taking | 8 (5) |
| Too much medicine | 8 (5) |
| Symptoms are under control | 15 (9.38) |
| Side effects | 11 (6.88) |
| Cost of medication | 12 (7.5) |
| Accessibility problems | 21 (13.13) |
| The medications are not helpful to control symptoms | 10 (6.25) |
| Forgetfulness | 37 (23.13) |
| Unclear why taking a number of medications | 4 (2.5) |
| Other reasons | 13 (8.13) |
The patients with low medication adherence levels were numerically older than the other adherence levels (12.06 ± 4.62 vs. 10.75 ± 3.93 and 10.58 ± 4.41 years old), but there was no statistically significant difference among the adherence levels (P-value = 0.137). Regarding gender, there were no significant differences among the adherence levels (P-value = 0.733). Of all patients who lived with both parents, 59 cases (41.55%) had low drug adherence, 37 cases (26.06%) were medium adherent, and 46 cases (32.39%) were high adherent. However, there was no statistically significant difference in this regard (P-value = 0.109). There was a significant difference among the drug adherence levels regarding the parents’ education (P-value = 0.048). The difference between housing status in low, medium, and high drug adherence was statistically significant (P-value = 0.021). Approximately half of the patients who were from families with an income level of lower than 15,000,000 Rials, 51 cases (46.36%) were low drug adherent, 17 (15.45%) medium adherent, and 42 (38.18%) high adherent. However, the analysis showed that there was a statistically significant difference among the medication adherence levels (P-value < 0.001). There was a significant difference among the medicine adherence levels (P-value = 0.02) based on the traveling time to the clinic. Patients who had inherited disease accounted for a higher percentage in the high adherence group (21; 46.6%). Also, 14 (70%) patients with the non-viral disease were low adherent to the liver disease medication. There was no statistically significant difference among the adherence levels regarding the cause of the chronic liver disease (P-value =0. 057) (Table 1).
Table 4 shows the results of the multivariate analysis. According to multivariate ordinal logistic regression modeling, the factors showed to be significantly associated with higher levels of medication adherence; the factors were patients’ age (OR = 0.875, CI: 0.781 - 0.980), underlying liver disease (non-viral disease patients (OR = 0.083, CI: 0.016 - 0.442), and cryptogenic patients (OR = 0.223, CI: 0.065 - 0.763)).
| Item | OR (95% CI) | P-Value |
|---|---|---|
| Patient’s age | 0.875 (0.781 - 0.980) | 0.021 * |
| Gender | ||
| Female | 1 | - |
| Male | 0.938 (0.347 - 2.537) | 0.9 |
| Parents’ education | ||
| Literate | 1 | - |
| Elementary | 0.775 (0.063 - 9.529) | 0.842 |
| Middle/high school | 2.933 (0.253 - 34.047) | 0.390 |
| Diploma | 1.109 (0.099 - 12.421) | 0.934 |
| Higher education | 0.831 (0.066 - 10.430) | 0.886 |
| Housing | ||
| Proprietary | 1 | - |
| Leased/ other | 0.351 (0.121 - 1.023) | 0.055 |
| Family monthly income | ||
| ≤15000000 | 1 | - |
| >15000000 | 0.648 (0.228 - 1.840) | 0.415 |
| Traveling time to the clinic | 0.999 (0.998 - 1) | 0.191 |
| Underlying liver disease | ||
| Inherited disease | 1 | - |
| Non-viral hepatitis | 0.083 (0.016 - 0.442) | 0.003* |
| Biliary obstruction/ lack of bile duct/ PSC/ hepatic vascular disease | 1.425 (0.374 - 5.424) | 0.603 |
| Cryptogenic | 0.223 (0.065 - 0.763) | 0.017 * |
| Tumor/ other | 0.719 (0.108 - 4.796) | 0.734 |
| Transplant candidate | ||
| No | 1 | - |
| Yes | 1.401 (0.436 - 4.507) | 0.571 |
5. Discussion
Medication adherence is a significant concern for health care providers around the world. It should be considered a significant issue in children with chronic disease in order to improve the outcomes and reduce the health care costs. The prevalence of medication adherence among children ranged from 11% to 93%, with an average of 50% (3, 15). Decompensated cirrhotic patients experience about 22 - 37% of 30-day readmission that is avoidable with accurate medication monitoring (16).
We reported medication adherence in children with chronic liver diseases in this study. The prevalence of patients with high adherence to medication was 35%. Also, medium and low adherence levels were 23.7 % and 41.25 %, respectively. The results of a study on end-stage liver disease patients showed 54 (30%) highly adherent patients and 127 (70%) low-adherers (9). Another study showed that 70% of those with decompensated liver cirrhosis had “low” or “medium” levels of medication adherence (16). The results are consistent with our results.
The most frequent reason for non-adherence was forgetfulness, followed by accessibility problems. These results are in line with previous surveys in pediatric and adult settings (9, 17). Interestingly, the reason for non-adherence in some cases was the unfavorable taste of drugs. About 10% of patients mentioned that they felt that their disease is under control. This could be a reflection of inadequate medical training. Moreover, 12 patients declared that their non-adherence is due to financial problems, and five of them felt that it was a reminder of their sickness. It may demonstrate the psychological aspect of non-adherence. The same reasons are reported in another study (18). One of the affordable and simple methods used to improve medication adherence is attention to the causes of medication non-adherence.
In most cases, the patients’ family members were responsible for assistance in taking medication, while in one-fourth of cases, children were taking drugs by themselves. Also, in about 10% of them, both children and their families participated. We could not find any significant association between non-adherence and parents’ role in medicine taking, and the overall distribution of patients with low, middle, and high adherence levels in different medication-taking groups were alike. In order to lower the low adherence to medications, especially in adolescents, it is recommended that we should shift from parent-care to self-care and autonomy (19).
About three-fourths of patients claimed that they had got necessary instruction on how to take their medication by medical staff. More than half of the patients who did not get the instructions were in the low adherence level group. Although no significant relationship was found regarding this issue, another study showed that it could improve the adherence level (20). A systematic review investigated the effect of interventions on medication adherence in children and adolescents with chronic illness; it was found that educational interventions alone were unlikely to enhance medication adherence in children and adolescents (21).
The patients with low medication adherence were older than other adherence levels, this group was in the adolescent period (mean age ± SD; 12.06 ± 4.62) in our study; however, there was no significant difference among the adherence levels. Hoegy et al. in a review study, reported low adherence levels among adolescents (10). The adolescence period of life is known as the transition process to decrease medication adherence for several reasons. For instance, Dobbels et al. reported behavioral factors as a significant reason for medical-non-adherence in adolescent stages (22).
The current study did not find any significant difference among adherence levels regarding the patients' gender. This may be due to the age group of our participants since they have not yet developed their own complete identity and sexual image. Boucquemont et al. reported the influence of age on the gender difference in adherence evaluation. There was no gender difference in adherence level among those aged 11 - 16 years; however, young women were more adherent than young men aged 17 - 24 years. The lack of gender variations in younger adolescents indicates that parents are responsible in part or completely for taking medication among this age group (23). On the other hand, another study has mentioned the difference between genders regarding adherence among adult patients (24).
We did not find a significant association between drug adherence and living status based on living with both parents or with one of them. Regarding this issue, the study of Hamilton et al. on young adults following kidney transplants indicated that a contributing factor associated with a higher medication adherence score was living with parents (25). This result may be attributed to the support they have from their family and/or better social support.
In multivariate logistic regression, age and underlying disease remained significantly associated with medication adherence.
In our study, there was no significant association between the parental education level and adherence level (Table 4). Although a strong association between lower levels of education and poorer health outcomes has been shown, it is not clear which degree of education can affect health outcomes. Today, health literacy is considered as a bridge between education and health and also a significant issue for improving health (26-28). A qualitative study from Iran mentioned that one of the weaknesses in healthcare systems is the educational problem, which has a prominent influence on medication adherence (29). Many experts suggested providing general health literacy, irrespective of their literacy or education levels, for all patients (30).
In the present study, the monthly income of the family did not have a significant relationship with adherence level (Table 4). This is inconsistent with the study by Albekairy et al. on liver transplant recipients from Saudi Arabia. They concluded that 68% of lower-income patients were adherent to their medication. In comparison, patients with a higher and median level of income were only 52% adherent (12). This result may be due to the differences in classifying monthly income and/or cultural variation.
In most cases, the underlying cause of the chronic liver disease was a genetic factor, the most frequent underlying cause in the high adherence group was inherited disease, followed by cryptogenic and non-viral hepatitis.
We faced some limitations in this study. We studied non-adherence using a questionnaire and self-declaration. Patients may not be honest in the socioeconomic parameters because they think that their financial status affects their insurance support, and it may affect the result of the study. An element of selection bias may exist in the present study. As we know, our study is the first to evaluate medication adherence using a self-reported Morisky scale in children with chronic liver diseases in Iran. This study can be a benchmark for other interventional and longitudinal studies. In this study, we recognized the children with low medical adherence that were liver transplant candidates. Medication non-adherence after transplant has serious outcomes, such as liver rejection or opportunistic infections. If we implement interventions to improve medication adherence among the children before transplantation, the impact of the intervention will sustain after transplantation. There are some suggested instructions to improve medication adherence in pediatric patients, such as personalized advising, simplified regimens, educational and medication reminder tools, improving drug taste, and collaborative partnership among health care providers, pharmacists, family members, and social workers (3, 15). However, prescribing medicines in children with liver disease is challenging, but most non-adherence reasons are modifiable.
5.1. Conclusions
Almost half of the children with chronic liver disease demonstrated low medication adherence. Our data highlight the need for chronic liver disease management programs to improve medication adherence in this vulnerable population.