1. Background
Atrial special defect (ASD) can cause left-to-right shunt at the atrial level, right atrial and ventricular dilation (1, 2), arrhythmia, pulmonary vascular disease, and other complications, which in the long term, may lead to an increase in morbidity and negative heart function. Remodeling and changes in the heart function can happen following the closure of ASDs, which may be complete or incomplete (3, 4). Following ASD and its closure, the left ventricle changes will also be predictable according to the ventricular-independent phenomenon (5-7). However, the changes in the right and left atria, ventricular size and function, and structural changes have not been fully identified following ASD closure (6). ASD closure may also have some complications, such as atrioventricular block, device displacement, aortic rupture, bleeding, and even death (1).
This study evaluated the cardiac cavities sizes and function by transthoracic echocardiography among children and adolescents whose ASDs were closed percutaneously, and the complications during the follow-up were specified.
2. Methods
Cardiac catheterization for the samples was done during 2010 - 2017 in Namazi teaching hospital of Shiraz University of Medical Sciences, Shiraz, Iran in this cross-sectional study. The patients were under the age of 18 years. Firstly, the previous echocardiography and angiographic records were checked out, and the characteristics regarding ASD size and the brand and size of the occluders and complications during angiography and follow-up were extracted from our database. The occluders were ASD with Amplatzer devices, and the average sizes of the used occluders were 20 - 25% bigger than the sizes of the ASDs in transthoracic echocardiography.
The inclusion criteria were QP/QS more than 1.5 in echocardiography and pulmonary vascular resistance less than 6 wood unit × m2 during the catheterization. The exclusion criteria were other interventions besides ASD closure, remaining shunts after ASD closure, other cardiac disorders, and cardiac arrhythmia before and after the procedures. Cardiac confounding factors were determined with echocardiography or cardiac catheterization, and pulmonary artery contrast injection with levophase was performed for all cases to rule out the abnormal pulmonary venous connection.
The patients were recruited for transthoracic echocardiography during 2018-2019, of whom half were selected randomly for echocardiography. In this study, both groups' information was provided, but the echocardiography characteristics belonged to the group accepted echocardiography. M-mode, 2- dimensional, flow Doppler, and tissue Doppler imaging (TDI) echocardiography was done for the selected group, and the function and dimensions of the right and left cardiac cavities, and the pulmonary artery and valve were evaluated (8).
Echocardiography was executed by the Samsung HS70A machine. The position of the patients was supine and left lateral during echocardiography. The echocardiographic data were determined as Z-score and divided into ≤ -2 and ≥ 2 Z-score groups. The Z-score parameters as the normal population with no ASD were obtained from the site: Nomograms for two-dimensional echocardiography derived valvular and arterial dimension in Caucasian children (9).
Size of the ASD and weight and age of the patients at the closure time are important factors during follow-up. Thus, we compared outcomes of the cardiac sizes and Z-scores of the patients with less and more than 15 mm ASD size, and less and more than 15 kg, and less and more than 3 years at the time of procedures.
Transthoracic echocardiography method: echocardiography was done on apical four chambers, subcostal, long axis, and short-axis views, and the sizes of the atria and ventricles and other cardiac parts were obtained according to the American Society of Echocardiography protocol (10).
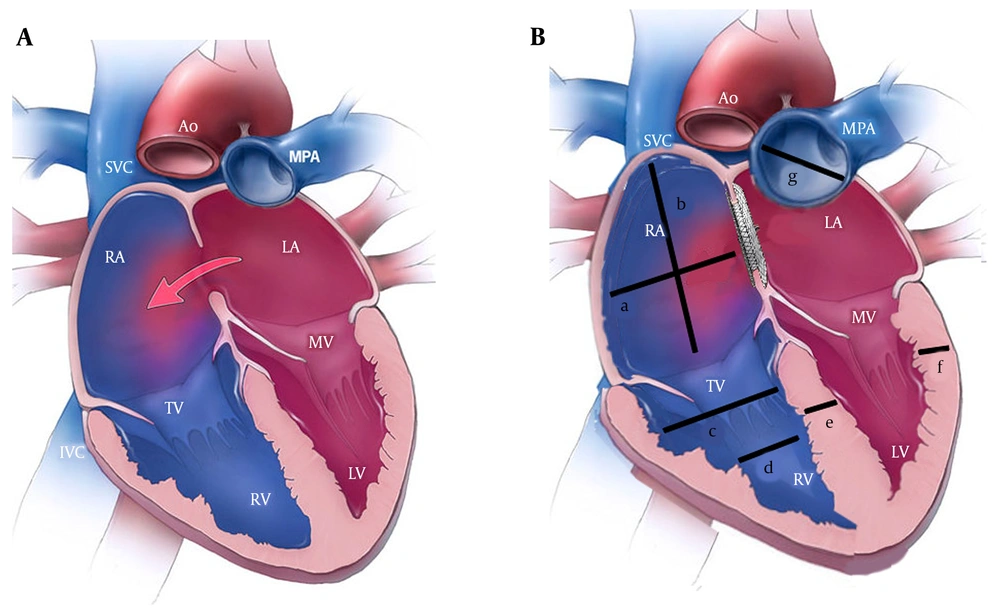
In the parasternal long-axis view, the right atrium and ventricle dimensions in systole and diastole, interventricular septal thickness, and ejection fraction were assessed (Figure 1). In the four-chamber view, the curser was placed on mitral and tricuspid valve leaflets, and the inflow E and A velocity, the dimension of the right atrium, and tricuspid annular plane systolic excursion (TAPSE) were recorded by the M-mode method.
(A) A schematic heart before atrial septal defect closure; (B) A schematic heart after atrial septal defect closure; a: Right atrial transverse dimension, b: Right atrial long axis dimension, c: Right ventricular end-diastolic diameter at the basal area; d: Right ventricular end-diastolic diameter at the mid cavity, e: Interventricular septal diameter in diastole, f: Left ventricular posterior wall diameter in diastole, and g: Main pulmonary artery. Abbreviations: ASD, atrial septal defect; TAPSE, tricuspid annular plane systolic excursion; TDI, tissue Doppler imaging.
Furthermore, in the four-chamber view, TDI was obtained while the cursor placed one cm apical to the mitral and tricuspid annuli, and pulse wave Doppler velocity was -20 to +20 cm/sec. An experienced pediatric cardiologist did echocardiography for all cases, and the parameters were obtained in three cycles, and the average values were used.
2.1. Statistical Analysis
The data were analyzed by SPSS version 23. The Kolmogorov-Smirnov test was used to assess the normal distribution, and continuous variables were described by mean ± standard deviation and medium. The data were statistically analyzed by the Pearson's correlation test, t-test, and chi-squared test. The P-value < 0.05 was considered as the significance level.
3. Results
Totally, 370 patients underwent interventional ASD closure, of whom 150 cases, including 75 males and 75 females were selected for echocardiography. The patient's mean follow-up time was 2.56 years (range: 6 months to 6 years). The patient's demographic characteristics are presented in Table 1. The average size of the occluders was 17.74 ± 4.0. In 126 patients (84%), the device size was 12 - 23 mm, and in 24 patients, the device size was bigger than 24 mm. The brand names of the occluders were Occlutech (Figula) from Germany and Lifetech, Memopart, Cardiofix, Starway, and Comed from China.
| Characteristics | Mean ± SD |
|---|---|
| The patients’ age at the time of catheterization (y) | 3.3 ± 6.61 |
| The patients' age at the time of the study (y) | 9.25 ± 3.44 |
| The patients’ weight at the time of catheterization (y) | 15.12 ± 11.83 |
| The patients' weight at the time of the study (y) | 13.06 ± 25.82 |
| The size of atrial septal defects (mm) | 14.43 ± 3.92 |
| Device size (mm) | 4.04 ± 17.74 |
The characteristics of M-mode echocardiography of the left ventricle, ejection fraction, and dimensions of the right atria and ventricles and the pulmonary artery are shown in Table 2. As it can be seen, 72% of these patients in the follow-up, in terms of interventricular septal dimension in diastole, had a Z-score of more than +2, and the left ventricular posterior wall dimension and the left ventricular internal dimension in systole of these patients were significantly higher than their peers.
| Characteristics | Mean ± SD | Z-score ± SD | The Percentage of Patients with Z-scores ≥ 2 | The Percentage of Patients with Z-scores ≤ -2 |
|---|---|---|---|---|
| IVSDD (cm) | 0.18 ± 0.708 | 1.88 ± 2.12 | 72 | 0 |
| LVPWD (cm) | 0.17 ± 0.72 | 1.50 ± 1.92 | 61 | 1 |
| LVIDD (cm) | 0.53 ± 3.66 | 1.20 ± 0.46 | 15 | 3 |
| LVIDS (cm) | 0.41 ± 2.15 | 1.59 ± 2.23 | 61 | 10 |
| IVSS (cm) | 0.25 ± 0.911 | 1.23 ± 0.63 | 9.3 | 1.3 |
| LVPWS (cm) | 0.21 ± 0.815 | 1.23 ± 0.96 | 2.6 | 18 |
| EF% | 9.58 ± 72.06 | - | -- | - |
| FS% | 8.14 ± 41.10 | - | - | - |
| TAPSE (cm) | 2.21 ± 0.52 | 1.76 ± 0.81 | 55 | 2 |
| Right atrial transverse dimension (cm) | 3.24 ± 0.47 | 1.57 ± 0.78 | 40 | 4 |
| Right atrial long axis dimension | 3.57 ± 0.84 | 1.66 ± 0.93 | 45 | 0 |
| RVED basal diameter (cm) | 3.54 ± 12.58 | 1.89 ± 0.73 | 47 | 4 |
| RVED mid cavity diameter | 2.27 ± 8.22 | 1.74 ± 0.61 | 35 | 3 |
| RVED length (cm) | 5.61 ± 18.34 | 1.61 ± 0.95 | 33 | 2 |
| Pulmonary annulus (cm) | 1.99 ± 4.23 | 2.04 ± 1.21 | 68 | 0 |
| Main pulmonary artery (cm) | 2.11 ± 5.37 | 2.23 ± 1.19 | 70 | 0 |
Abbreviations: EF, ejection fraction; FS, fractional shortening; IVSDD, interventricular septal diameter at the end of diastole; IVSS, interventricular septal dimension in systole; LVIDD, left ventricular internal dimension in diastole; LVIDS, left ventricular internal dimension in systole; LVPWD, left ventricular posterior wall thickness in diastole; LVPWS, left ventricular posterior wall thickness in systole; RVEDD, right ventricular end-diastolic dimension; SD, standard deviation; TAPSE, tricuspid annular plane systolic excursion.
Although the right atria and ventricular dimensions were more than the same population, the TAPSE of this group was more than the same-age children and adolescents (Table 2). Therefore, the activity of the right ventricle was not reduced in this regard. According to Table 2, Z-scores of the pulmonary valve annulus and the main pulmonary artery at the follow-up time were higher than the normal population.
Besides, according to Tables 3 and 4, Z-scores of the flow Doppler and TDI data of the mitral valve were not significantly different from the normal population, but the Z-scores of the E/A and Eat/Aat of the tricuspid valve in TDI was less than the peers. The tricuspid valve E-velocity was less than the peers, but the tricuspid valve Aa velocity was similar to the normal population.
| Characteristics | Mean ± SD | Z-score ± SD | The Percentage of the Patients with Z-scores ≥ 2 | The Percentage of the Patients with Z-scores ≤ -2 |
|---|---|---|---|---|
| Et | 17.76 ± 75.81 | -2.71 ± 0.71 | 0 | 57 |
| At | 16.10 ± 48.49 | -0.85 ± 0.97 | 1 | 3.3 |
| Et/At | 1.33 ± 0.44 | 0.98 ± 0.63 | 2 | 48 |
| Em | 97.71 ± 25.12 | 1.21 ± 0.35 | 3 | 6 |
| Am | 55.08 ± 19.27 | 1.43 ± 0.51 | 2 | 3 |
| Em/Am | 1.99 ± 0.71 | 1.52 ± 0.61 | 4 | 6 |
Abbreviations: Am, peak A velocity in the mitral valve; AT, peak A velocity in the tricuspid valve; Em, peak E velocity in the mitral valve; Et, peak E velocity in the tricuspid valve; Em/Am, the ratio of peak E to peak A in the mitral valve; Et/At, the ratio of peak E to peak A in the tricuspid valve.
| Variables | Mean ± SD | Z-score ± SD | The Percentage of Patients with Z-scores ≥ 2 | The Percentage of the Patients with Z-scores ≤ -2 |
|---|---|---|---|---|
| Sat (cm/s) | 2.81 ± 13.13 | 1.34 ± 0.20 | 9 | 5 |
| Eat (cm/s) | 3.56 ± 15.80 | 1.10 ± 0.31 | 2 | 2 |
| Aat (cm/s) | 3.74 ± 12.62 | 1.23 ± 0.79 | 19 | 0 |
| Eat/Aat | 4.99 ± 1.63 | 2.12 ± 0.75 | 0 | 43 |
| Eas (cm/s) | 3.37 ± 13.16 | 1.71 ± 0.25 | 11 | 3 |
| Aas (cm/s) | 2.76 ± 8.26 | 1.59 ± 1.31 | 22 | 0 |
| Sam (cm/s) | 8.61 ± 2.01 | 1.25 ± 1.24 | 11 | 5 |
| Eam (cm/s) | 13.65 ± 2.87 | 0.98 ± 0.78 | 9.24 | 4 |
| Aam | 5.53 ± 1.78 | 1.51 ± 1.13 | 10 | 11 |
| Em/Aam | 4.11 ± 1.25 | 1.34 ± 0.69 | 2 | 8 |
Abbreviations: Aam, mitral annular late diastolic velocity; Aas, septal annular late diastolic velocity; Aat, tricuspid annular late diastolic velocity; Eam, mitral annular early diastolic velocity; Eam/Aam, the ratio of early to late mitral annular diastolic velocity; Eas, septal annular early diastolic velocity; Eat, tricuspid annular early diastolic velocity, Eat/Aat, the ratio of early to late tricuspid annular diastolic velocity; SD, standard deviation; Sm, mitral annular systolic velocity; St, tricuspid annular systolic velocity.
In terms of complications, 27 patients (7.29%) out of 370 patients had significant complications. One patient had femoral vein thrombosis (0.27), and in six patients, the occluders were displaced from the ASD site after releasing (1.62%). In three patients, the devices were embolized immediately after the device was released, and in three other patients, the devices were dislocated one, three, and seven days after implantation. Of these six patients, two patients' occluders were retrieved percutaneously, and the rest were removed in the operating room, and their ASDs were surgically closed. Furthermore, five out of 370 patients (1.35%), developed the third-degree atrioventricular block following device implantation and just before their release, and the devices were retrieved, and they were sent for surgery, and the heart block was resolved.
However, two out of 370 patients (0.59%) developed the third-degree atrioventricular block a few days after inserting the occluders. The ASD was closed surgically, but the heart block was not resolved, and for the second patient, a pacemaker was inserted into the heart without removing the Amplatzer.
Some chambers in ASDs larger than 15 mm were bigger at follow-up in comparison to the ASDs less than 15 mm, and there was a significant positive correlation among the right ventricular end-diastolic dimension at the basal part (r = 0.39, P = 0.026), the mid cavity part (r = 0.421, P = 0.031), pulmonary valve annulus (r = 0.33, P = 0.042) and the main pulmonary artery (r = 0.59, P = 0.001) in cases with larger ASDs. Besides, the flow Doppler velocity of the At was higher among the larger ones (r = 0.377, P = 0,028).
Also, Z-scores of some parameters were significantly higher in ASDs larger than 15 mm, in comparison to smaller than or equal to 15 mm so that the right atrial transverse dimensions were 2.17 ± 1.78 and 1.37 ± 0.98 (P = 0.045), and the right ventricular end-diastolic dimensions at the basal part were 2.16 ± 0.83 and 1.33 ± 0.65 (P = 0.021), the Z-scores of St were 12.93 ± 2.71 and 14.36 ± 3.22 (P = 0.034), and the Z-scores of At were 4.67 ± 1.33 and 5.70 ± 2.30 (P = 0.038), respectively.
Furthermore, some parameters in patients less than or equal to 15 kg and above 15 kg had significant differences. In this regard, the Z-scores of the interventricular septal dimension in systole were 0.32 ± 0.10 and 0.72 ± 0.12 (P = 0.010), and the Z-scores of the Et were -2.25 ± 0.09 and -2.8 ± 0.06 (P = 0.001), respectively (Table 5).
| Variables | Group | P-Value | |
|---|---|---|---|
| ≤ 15 kg | > 15 kg | ||
| EF% | 72.92 ± 1.79 | 72.05 ± 0.89 | 0.655 |
| FS% | 41.61 ± 1.69 | 41.29 ± 0.78 | 0.852 |
| Z-score -IVSD | 1.72 ± 0.23 | 2.27 ± 0.19 | 0.141 |
| Z-score -LVIDD | 0.35 ± 0.21 | 0.50 ± 0.11 | 0.537 |
| Z-score -LVIDS | -0.45 ± 0.19 | -0.20 ± 0.17 | 0.458 |
| Z-score -IVPWD | 2.08 ± 0.29 | 1.86 ± 0.13 | 0.473 |
| Z-score -LVPWS | -1.15 ± 0.25 | -0.90 ± 0.11 | 0.323 |
| Z-score -IVSS | 0.32 ± 0.10 | 0.72 ± 0.12 | 0.010 |
| Z-score -Sat | 0.07 ± 0.27 | -0.22 ± 0.12 | 0.281 |
| Z-score -Eat | -0.35 ± 0.17 | -0.27 ± 0.10 | 0.704 |
| Z-score -Aat | 0.85 ± 0.19 | 0.80 ± 0.12 | 0.827 |
| Z-score -Sas | 0.53 ± 0.25 | 0.37 ± 0.16 | 0.613 |
| Z-score -Eas | -0.29 ± 0.24 | 0.12 ± 0.17 | 0.227 |
| Z-score -Aas | 1.32 ± 0.31 | 1.31 ± 0.15 | 0.971 |
| Z-score -Et | -2.25 ± 0.09 | -2.84 ± 0.06 | 0.001 |
| Z-score -At | -0.74 ± 0.17 | 0.89 ± 0.14 | 0.576 |
| Z-score -TAPSE (cm) | 1.21 ± 0.52 | 1.36 ± 0.81 | 0.651 |
| Z-score -right atrial transverse dimension (cm) | 1.61 ± 0.39 | 1.57 ± 0.69 | 0.257 |
| Z-score -right atrial long axis dimension (cm) | 1.19 ± 0.72 | 1.71 ± 0.72 | 0.549 |
| Z-score -RVEDwidth in the basal area (cm) | 1.54 ± 1.49 | 1.28 ± 0.53 | 0.813 |
| Z-score -RVED width in the mid-cavity (cm) | 1.22 ± 1.49 | 1.34 ± 0.61 | 0.122 |
| Z-score -RVED length (cm) | 1.62 ± 1.38 | 1.47 ± 0.78 | 0.425 |
Abbreviations: Aas, septal tissue late diastolic velocity; Aat, tricuspid annular late diastolic velocity; At, peak A velocity in the tricuspid valve; Eas, septal tissue early diastolic velocity; Eat, tricuspid annular early diastolic velocity; EF, ejection fraction; Et, peak E velocity in the tricuspid valve; FS, fractional shortening; IVSD, interventricular septal thickness in diastole; IVSS, interventricular septal thickness in systole; LVIDD, left ventricular internal dimension in diastole; LVIDS, left ventricular dimension in systole; LVPWD, left ventricular posterior wall thickness in diastole; LVPWS, left ventricular posterior wall thickness in systole; RVED, right ventricular end-diastolic dimension; Sas, septal tissue systolic velocity; Sat, tricuspid annular systolic velocity; TAPSE, tricuspid annular plane systolic excursion.
aValues are expressed as mean ± SD.
In comparison to patients less than or equal to 3 years and older, the Z-scores of the Sat were 0.19 ± 0.21 and -0.29 ± 0.13, (P = 049), Z-scores of the Aat were (1.14 ± 0.15 and 0.67 ± 0.13 (P = 0.042), Z-scores of the Aas were (1.80 ± 0.28 and, 1.11 ± 0.15 (P = 0.020), and Z-scores of the At were (-0.39 ± 0.25 and -1.04 ± 0.11 (P = 0.009) respectively, and there were significant statistically differences; however, they were in the normal range (Table 6).
| Variables | Group | P-Value | |
|---|---|---|---|
| ≤ 3 (y) | > 3 (y) | ||
| EF% | 70.99 ± 11.60 | 72.73 ± 0.86 | 0.38 |
| FS% | 40.76 ± 1.72 | 41.59 ± 0.72 | 0.65 |
| Z-score-IVSD | 2.12 ± 0.26 | 2.16 ± 0.19 | 0.91 |
| Z-score -IVIDD | 0.22 ± 0.19 | 0.57 ± 0.11 | 0.11 |
| Z-score -IVIDS | -0.27 ± 0.34 | -0.25 ± 0.13 | 0.97 |
| Z-score -IVPWD | 1.83 ± 0.23 | 1.94 ± 0.15 | 0.69 |
| Z-score -LVPWS | -1.01 ± 0.17 | -0.93 ± 0.12 | 0.73 |
| Z-score -IVSS | 0.42 ± 0.21 | 0.71 ± 0.11 | 0.20 |
| Z-score -Sat | 0.19 ± 1.33 | -0.29 ± 1.33 | 0.049 |
| Z-score -Eat | -0.28 ± 0.17 | -0.29 ± 1.11 | 0.93 |
| Z-score -Aat | 1.14 ± 0.15 | 0.67 ± 0.13 | 0.42 |
| Z-score -Sas | 0.74 ± 0.34 | 0.28 ± 0.13 | 0.12 |
| Z-score -Eas | -0.69 ± 0.18 | 0.31 ± 0.18 | 0.000 |
| Z-score -Aas | 1.80 ± 0.28 | 1.11 ± 0.15 | 0.02 |
| Z-score -Et | -2.60 ± 0.12 | -2.7 ± 0.62 | 0.28 |
| Z-score -At | -0.39 ± 0.25 | -1.04 ± 0.11 | 0.009 |
| Z-score -TAPSE (cm) | 1.21 ± 0.52 | 1.36 ± 0.81 | 0.651 |
| Z-score -right atrial transverse dimension (cm) | 1.82 ± 0.39 | 1.45 ± 0.69 | 0.341 |
| Z-score -right atrial long axis dimension (cm) | 1.76 ± 0.61 | 1.74 ± 0.49 | 0.649 |
| Z-score -RVED width in the basal area (cm) | 1.54 ± 0.99 | 1.28 ± 0.75 | 0.568 |
| Z-score -RVED width in the mid-cavity (cm) | 1.92 ± 1.63 | 1.92 ± 0.78 | 0.922 |
| Z-score -RVED length (cm) | 1.71 ± 0.99 | 1.83 ± 0.86 | 0.701 |
Abbreviations: Aas, septal tissue late diastolic velocity; Aat, tricuspid annular late diastolic velocity; At, peak A velocity in the tricuspid valve; Eas, septal tissue early diastolic velocity; Eat, tricuspid annular early diastolic velocity; EF, ejection fraction; Et, peak E velocity in the tricuspid valve; FS, fractional shortening; IVSD, interventricular septal thickness in diastole; IVSS, interventricular septal thickness in systole; LVIDD, left ventricular internal dimension in diastole; LVIDS, left ventricular dimension in systole; LVPWD, left ventricular posterior wall thickness in diastole; LVPWS, left ventricular posterior wall thickness in systole; RVED, right ventricular end-diastolic dimension; Sas, septal tissue systolic velocity; Sat, tricuspid annular systolic velocity; TAPSE, tricuspid annular plane systolic excursion.
aValues are expressed as mean ± SD.
Furthermore, out of 370 patients, three cases (0.81%) had congenital third-degree heart block with appropriate heart rate before ASD closure, and positive anti-Ro/SSA antibody in the mother, but following ASD closure, they experienced a decrease in the heart rate that permanent pacemaker was inserted for them.
4. Discussion
The presence of ASD, if there is an indication of closure, can lead to the enlargement of the right atrium and ventricle and reduces the dimensions of the left atrium and ventricle. Also, the ASD closure can move the dimensions of the cavities and parts of the heart toward normal (11).
In some studies, echocardiographic parameters have been studied by two interventional and surgical methods. After the mid-term follow-up, echocardiographic data had less diversion from the normal population in the intervention method than the surgical method (12, 13). However, there was no difference between surgical and interventional methods in most studies according to the outcome (14-17). Some studies have shown that ASD closure reduces the size of the right anatomical structures and increases the left side of the heart (18).
Blood flow and TDI data of patients were also examined and compared to normal cases by researchers. Although no study or few has been done on the Z-scores of the cardiac cavities and the main pulmonary artery and the echocardiographic parameters after ASD closure, the parameters mentioned above were assessed in this study.
In some studies, following the closure of ASDs, the left ventricular ejection fraction increased, whereas the TAPSE decreased. It seems that further blood flow to the left side of the heart can increase the size of the left cardiac chambers, and also, along with an increase in the left ventricular preload, the ejection fraction increases according to Frank Sterling's law (19). Furthermore, after reducing the preload of the right cardiac chambers, the size of these cavities and the TAPSE will reduce. Nonetheless, in some studies, the mitral annular plane systolic excursion showed an increase, but the TAPSE did not (20).
However, a remarkable percentage of the patients had a Z-score > 2 after 2.5 years of follow-up regarding the right cardiac sizes, and the diameter of the pulmonary valve annulus, pulmonary artery diameter, TAPSE, the interventricular septal dimension in diastole, left ventricular posterior wall dimension in diastole, and the left ventricular internal dimension in systole.
On the other hand, in some studies, in patients with ASD, apical right ventricular strain parameters were higher than the basal part, and after the ASD closure, the strain of both parts reduced (1). In another study, patients before and after ASD closure were examined for blood flow Doppler echocardiography and TDI, in which the Et/At decreased and Et/et increased, but there was no diversion in TDI parameters (21, 22). In our study, a Z-score ≤ 2 was observed in the Et/At and Eat in a noticeable percentage of subjects after ASD closure (Tables 4 and 3).
In a study, in the adult cases, echocardiographic results of ASD closure before and after 25 years old were compared to older cases, and tricuspid regurgitation increased significantly more than the other group (23).
In our study, if the age at the ASD closure was three years old, Z-scores of the Sat, Aat, Aas, and At were significantly lower than the age of over three years. Also, regarding the correlation between ASD size greater than and smaller than 15 mm, the Z-scores of the right cardiac chamber sizes, the pulmonary valve annulus, and the main pulmonary artery were higher in patients with the larger ASDs.
Our study compared ASD closure among patients under and more than 15 kg and showed that those with lower weight had lesser interventricular septal dimension in systole.
According to our study, closure of the large ASDs might be recommended earlier, at the age of fewer than three years and the weight of less than 15 kg, to prevent dilating the right cardiac chambers; however, this suggestion should be further examined in the next studies.
Furthermore, the third-degree heart block can occur in some patients, and several studies have declared that this impediment can be treated with steroids (17). However, in one of our patients, steroids could not solve the problem, and the Amplatzer was removed surgically after two weeks, and the ASD was closed with surgical method, and the cardiac block remained. In our second patient, following the block, the steroid was prescribed, but the block did not resolve, and a pacemaker was used. Nonetheless, some studies have suggested that the block may be resolved by steroids administration, and the block of some patients has been removed through the retrieval of the Amplatzers (24).
4.1. Conclusions
The larger ASDs possibly have more adverse effects on the Z-scores than the smaller ones after closure, and the larger ASDs should be closed earlier.
Patients who underwent ASD closure at the age of fewer than three years had more normal cardiac Z-scores than cases over three years, and longer follow-ups require to find out the adverse effects of the ASD on the cardiac Z-scores.