1. Context
In 2015, the United Nations decided on a new set of sustainable development goals which for the first time recognized surgery as an integral and necessary component for a functioning health system (1). Prior to this, with the support of The Lancet, a commission for global surgery was formed with the goal of identifying the barriers to access of surgical care and offer recommendations. At that time, there was little to no published data on the actual burden of surgical disease from either a clinical perspective or economic standpoint in low and middle income countries (LMICs). The hope was to first define the problem and next identify the opportunities for improvement and development for LMICs to provide quality and safe surgery. In January 2014, 25 international commissioners, advisors and collaborators came together with representatives of over 110 countries for the first lancet commission meeting.
Over the course of the next year, the group came up with 5 key messages, a set of indicators, and recommendations to improve access to surgery and provide a framework for national surgical planning which was ultimately published in the spring issue of the Lancet in 2015. The utmost important conclusion from the commission was that an increase in surgical access is not only affordable, but also cost effective and achievable for LMICs. The expansion of widespread surgical care was shown to improve overall health and welfare of populations while also providing significant economic returns. Here we will summarize the key messages and recommendations brought forth in the report (2).
2. Defining the Problem
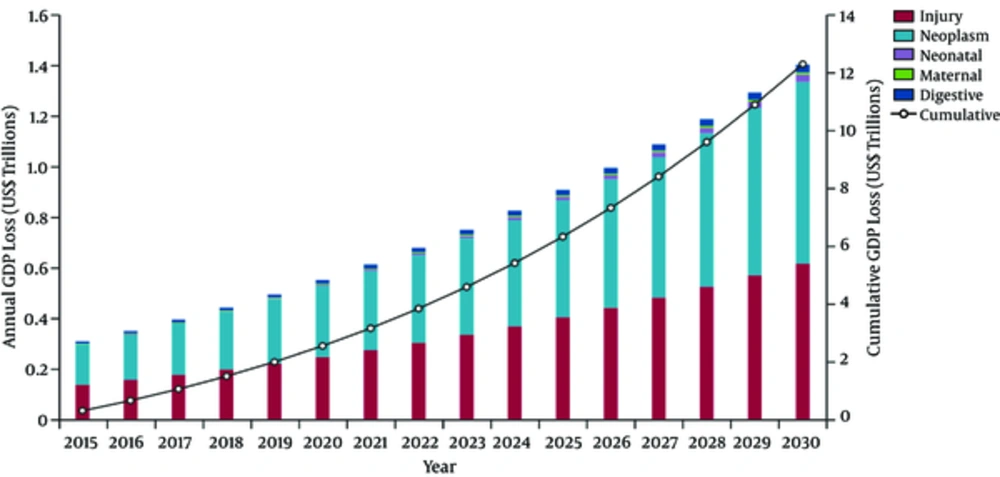
Surgery has rightfully been called the neglected step child of global health (2). However, with 28% - 32% of the global burden of disease attributed to surgically treatable conditions, the importance is undeniable (3). In 2010, nearly 17 million people died from surgical conditions alone (3). Despite the high prevalence of surgical disease, for the majority of the world surgical care remains out of reach (4). The consequence of untreated surgical conditions leads to significant morbidity and mortality (5-7). From an economic standpoint, the lack of surgery affects not only economic productivity but growth and development (2). If access to surgical care does not improve, the financial losses from surgical conditions is estimated to be $12.3 trillion between 2015 - 2030 (2). This translates to a reduction of annual GDP growth by as much as 2% in some countries (Figure 1) (2).
Annual and cumulative GDP lost in low-income and middle-income countries from five categories of surgical conditions (2010 US$, purchasing power parity) (8). Data are based on WHO’s projecting the economic cost of ill-health (EPIC) model (2010 US$, purchasing power parity). GDP = gross domestic product
3. Target Audience
The report was written with key stakeholders in mind – those with the investment capabilities, power and ability to implement policy change. The major target audience is government officials of LMIC’s who ultimately have the lead in strengthening their own surgical services and health systems. NGOs (non-governmental organization) and other developmental organizations have a well-known roll in surgical delivery in LMIC’s thus this report also highlighted the importance of implementation of the suggested surgical indicators within the already existing health monitoring systems. Funding agencies both locally and globally are motivated to invest in surgical care as a means to avoid further financial catastrophe for those impoverished and altogether poverty alleviation. The report calls to action international partners as well to further support LMIC’s in their efforts to deliver surgical care. Further, a recognition by the general public of the right to surgical care is emphasized. Finally, advances in surgical care delivery and access will only be achievable with the cooperation of all stakeholders under the direction and lead of a national government (2).
4. Methodology
The commissioners were divided into four working groups - health care delivery and management, workforce and education, information management, and financing and economics. Each group consisted of not only commissioners but also key advisors, and research assistants that would discuss in depth the specific area of importance. The groups would engage with stakeholders, providers, NGOs, funders, patients and students to provide the most informative and comprehensive recommendations based on these discussions.
The final output from each group combined formed the final report which included surgical indicators, recommendations, and goals to achieve universal access to safe and affordable surgical care by 2030 (2).
5. Key Messages
Currently 5 billion people lack access to safe, affordable surgical and anesthesia care (Figure 2). Access to care is defined as the proportion of the population that can access a facility capable of performing bellwether procedures (cesarean sections, exploratory laparotomy, and treatment of open fractures) (2). The definition was derived by evaluating the four dimensions of access which include timeliness, surgical capacity, safety and affordability (9-12). It is estimated that nearly 70% of the global population currently cannot access the surgical treatment they need (2). Not surprisingly, surgical access is worse in LMICs and particularly for those patients in the poorest wealth quintiles within countries of all income groupings (4). The proposed 2030 goal is for 80% coverage of essential surgical and anesthesia services per country (2). This will require data collection by LMICs to evaluate their current access followed by strategic integration of surgical services across all levels of care. Delays in seeking care and evaluating for safe and affordable surgical care will also need to be addressed in parallel with surgical systems strengthening.
143 million additional surgical procedures are needed each year to save lives and prevent disability. The lack of access to surgical care leads to significantly higher mortality rates for common surgical conditions. Obstructed labor is a common example that without access to a surgeon can lead to death of both the mother and infant. Open fractures left untreated can lead to debilitating disability with catastrophic loss from a financial, personal and social perspective. The estimated unmet annual surgical need is geographically variable, with roughly 3384 per 100,000 population additional cases needed in Latin America compared to almost double that number in sub-Saharan Africa (6496 cases per 100,000). The need is greatest in Sub-Saharan Africa (west, east, and central) as well as South and Southeast Asia. The 2030 target proposed is 5000 procedures for 100,000 populations. This will require extensive expansion of surgical systems and in many countries nearly doubling of the current workforce, while simultaneously maintaining or improving quality, safe and equitable delivery (2).
33 million individuals face catastrophic health expenditure due to payment for surgery and anesthesia each year. This number represents 22% of the estimated 150 million people who suffer catastrophic expenditure from all types of healthcare (13). Catastrophic expenditure is defined as the direct medical payments for surgical care that exceed 10% of a patient’s total income or 40% of income after basic needs for food and shelter are met (14). The issue stems from out of pocket user fees for surgical care that are often high resulting in large rates of impoverishment from healthcare interventions (15, 16). It is estimated that 1/4 of all people who have a surgical procedure will face financial catastrophe (17). This burden falls heavily on the poor, and again is more common in LMICs and the poorest wealth quintiles (4). The 2030 target is therefore 100% protection against catastrophic expenditure. This will involve implementation of strategic financial safety mechanisms based on the pooling of risk through taxation or insurance models with phasing out of fee for service and out of pocket payment models. This movement will lead down a path towards universal health coverage and acommitmentto coverage of the poor. Surgical care will need to be included in all basic universal health coverage (UHC) packages and policies(2).
Investment in surgical and anesthesia is affordable, saves lives, and promotes economic growth. In order to reach the 2030 target of 5000 procedures per 100, 000 populations there must be a scale up of surgical services by an estimated 9% worldwide (2). The cost of expanding surgical services in 88 LMICs by 2030 is estimated to be close to $300 billion dollars ($16 billion annually) (2). Although this cost seems astronomical, the calculated loss of total GDP is 12.3 trillion dollars, which equates to a reduction of annual GDP growth to as much as 2% (2). Further, access to basic surgical care will avert an estimated 77.2 million disability-adjusted life years each year (5). To improve the overall general health of a population while also decreasing the economic burden of surgical conditions, the Commission recommends national governments to include surgical system needs within the movement towards UHC. The expectation needs to be that UHC will include a package of essential surgical care early in the quality, access, and financial risk protection expansion pathways. This will not only need to be championed by National Governments but will require a combined financial commitment from domestic and international funding partners (2).
Surgery is an indivisible, indispensable part of healthcare. Universal access to surgery is essential for widespread improvement in global health, welfare, and economic development (2). The surgical burden continues to grow and if not addressed, common treatable conditions will continue to lead to significant morbidity, mortality and economic catastrophe (2). The implementation of timely intervention has the potential to avert over 100,000 maternal deaths and reduce neonatal mortality by 30% - 70% (18). Because of the necessary equipment and staffing required for surgical services, the integration of surgery at the district level will lend itself to expansion of other healthcare’s services. The presence of surgical care will then be an indicator of a higher functioning health system given the inherent complexity of delivering safe surgery (2). In order to achieve higher levels of health for a community, safe and affordable surgical care is obligatory, and therefore, policy makers, implementers, and funders must include surgical care into their national health plan (2).
6. Implementation
In order to integrate surgical care into a national health system it is first necessary to develop a system for clinical audit, impact evaluation, and health research capabilities to generate local data on current surgical services and outcomes (2). Ministries of Health, Academic institutions, private and public health service providers and institutions all have a role in delivering surgical and anesthetic care. The commission hence developed a set of 6 core indicators for monitoring universal access to safe and affordable care that revolved around preparedness, delivery, and impact of surgical and anesthetic care (Table 1). The Commission urges ministries of health to commit and invest in data collection for these indicators to be used as a starting point for decision making regarding policy changes and resource allocation. This data collection would allow countries to not only identify areas of unmet need, implement new programs and policy specific to their country, but also provide a means for monitoring progress. The indicators can also function as a benchmark to compare and facilitate learning between countries.
| Indicator Name | Target |
|---|---|
| Access to timely essential surgery | A minimum of 80% coverage of essential surgical anaesthesia services per country by 2030 |
| Specialist surgical workforce density | 100% of countries with at least 20 surgical, anaesthesia and obstetric physicians per 100 000 population by 2030 |
| Surgical volume | 80% of countries by 2020 and 100% of countries by 2030 tracking surgical volume; A minimum of 5000 procedures per 100 000 population by 2030 |
| Perioperative mortality rate (POMR) | 80% of countries by 2020 and 100% of countries by 2030 tracking POMR; In 2020, evaluate global data and set national targets for 2030 |
| Protection against impoverishing expenditure | 100% protection against impoverishment from out of pocket payments for surgical and anaesthesia care by 2030 |
| Protection against catastrophic expenditure | 100% protection against catastrophic expenditure from out of pocket payments for surgical and anaesthesia care by 2030 |
Indicators 1 and 2 focused on preparedness for surgical access. It is recommended that a minimum of 80% of the country have access to timely surgery (2). Timely surgery was defined as the proportion of the population with access, within 2 hours, to a facility capable of performing the Bellwether procedures (2). The second indicator is the density of the specialist surgical workforce, defined as the number of specialist surgical, anesthetic and obstetric physicians who are working per 100,000 populations (2). The target is 100% of countries with at least 20 surgical, anesthetic, and obstetric physicians per 100,000 populations by 2030 (2).
Indicators 3 and 4 monitor the delivery of surgical and anesthesia care. The number of surgical procedures done per year is an indicator of met need. The target by 2020 is 80% of countries and 100% of countries by 2030, to be not only tracking surgical volume, but be performing 5000 procedures per 100,000 populations (2). The fourth indicator, peri-operative mortality rate (POMR), highlights the integral component of safety in care delivery (19). POMR is defined as the all-cause death rate prior to discharge among patients who have undergone a procedure in an operating room, divided by the total number of procedures presented as a percentage (2). The target for 2020 is 80% of countries to be tracking POMR and by 2030, 100% of countries be able to assess their POMR and set future national targets (2).
The final two indicators, 5 and 6, revolve around the financial impact that surgical care can have on patients. The fifth core indicator is protection against impoverishing expenditure, defined as the proportion of households protected against impoverishment from direct out of pocket payments (OOP) for surgical and anesthetic care that drive them into or further into poverty (2). The target for 2030 is 100% protection against impoverishment from OOP payments for surgical and anesthesia care. The final indicator is protection against catastrophic expenditure which is the proportion of households protected against catastrophic expenditure from direct OOP payments for surgical and anesthetic care. Similarly, the goal is 100% protection from catastrophic expenditure.
7. National Surgical Planning
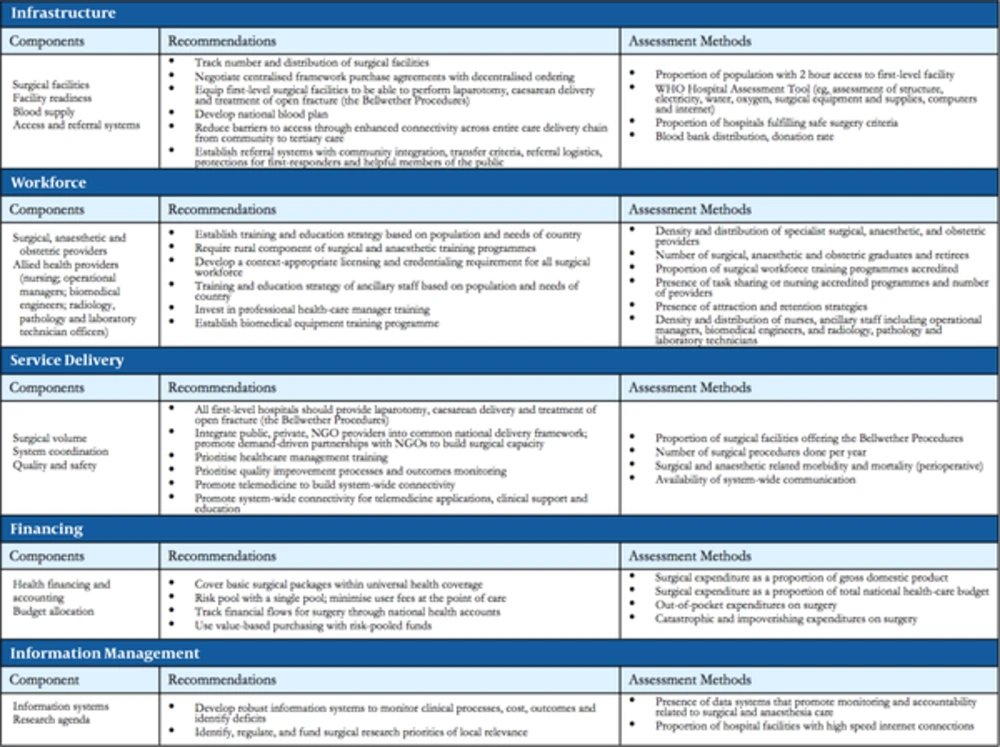
Finally, the commission provides a template for development of a national surgical plan (NSP) with the hopes of accelerating the scale up of surgical care and ultimately improving the health welfare and economic state of LMICs (Figure 3). The formation of a NSP is essential in order to improve delivery, expand education and develop research capabilities. It requires a commitment at both the national and international level with involvement of various stakeholders to be successful. The template includes five major domains that should be considered in construction of a NSP infrastructure, workforce, service delivery, information management, and financing.
8. Infrastructure
Surgical facilities, facility readiness, blood supply, and access to referral systems are the building blocks required for surgical delivery. It is recommended that number and distribution of surgical facilities should be tracked. Furthermore, there needs to be a negotiation for centralized framework purchase agreements with decentralized ordering. Pre-identified facilities lacking the ability to perform Bellwether procedures need to be equipped and staffed to expand their current surgical capacity to perform cesarean sections, exploratory laparotomies and open fracture treatment.
A National blood plan should be incorporated to ensure that safe and appropriate supplies are available for any patients requiring transfusion. Moreover, referral processes including transfer criteria, referral logistics, and community integration need to be addressed and defined. Assessment of the current state can be accomplished with the utilization of the WHO hospital assessment tool and data collection of current hospitals fulfilling safe surgery criteria, existing blood bank distribution and donation rate, as well as 2-hour access to surgical facilities.
9. Workforce
The surgical workforce includes not only surgical, anesthetic and obstetric providers, but also allied health providers including but not limited to nursing, operational managers, engineering, radiology, pathology, and laboratory technicians.
A NSP should define the training and education strategy based on the population and specific needs of the country. A rural training component should be required and encouraged for all surgical and anesthetic training programs. Training of ancillary staff should cater to the specific needs of the country. An emphasis on professional health care manager training is crucial. Allocation of resources to develop a biomedical engineering and equipment maintenance training program should be considered.
The assessment methods for workforce include evaluating the current density and distribution of specialist surgical, anesthetic and obstetric providers. It is also important to identify the number of surgical workforce training programs and number of surgical and nursing graduates. The density and distribution of nurses and ancillary staff must also be documented and the role of task sharing if present.
10. Service Delivery
The components of service delivery include surgical volume, system coordination and quality and safety. The commission recommends that all first level hospitals be capable of providing laparotomy, cesarean delivery and treatment of open fractures as bellwether procedures indicating the ability to provide a wide variety of surgical services. When forming a national delivery framework, providers from public, private and NGOs should be integrated, with the promotion of a demand-driven partnership between NGOs to build surgical capacity. Priority should be placed on quality improvement processes, outcomes monitoring, telemedicine promotion, and system wide connectivity for clinical support and education. Suggested assessment methods for surgery delivery include identifying the proportion of surgical facilities offering the bellwether procedures, identifying the number of procedures /year, collecting morbidity and mortality data, and assessing the availability of system wide communication.
11. Financing
Core components of financing are framed around patient costs for surgical care, systemic costs for providing surgical care, and budgetary considerations for surgical services.
Highlighting the foundational role of surgery in universal health services, the commission recommends implementing financial risk protection mechanisms for basic surgical packages. This combined with risk pooling to minimize user fees at point-of-care for patients will achieve great strides in decreasing financial barriers for populations to access surgical services. Systemic costs and budgetary needs can be addressed through tracking financial flows for surgery through existing health accounts. Furthermore, methods to risk pool funds and ensure protection from governmental and economic shifts should be used to engage in value-based purchasing and resilient supply chains.
Consistent assessment and optimization of surgical care’s financial impact can be established once basic tracking of financial flows for surgical care is established. After this crucial step, expenditure on surgery as a proportion of GDP and as a proportion of total national health budgets can be calculated to monitor systemic costs. Additionally, patient costs can be monitored through assessing out-of-pocket expenditures to access surgical care.
12. Information Management
The most basic processes of information management include data collection, analysis, reporting, and implementation. To address these processes the commission developed recommendations for information systems and research agendas.
Whether paper-based or digital, a key first step identified by the commission for information management is the development of robust information systems to monitor surgical care processes, costs, and outcomes. This serves to identify deficits, which can directly lead to impactful research and innovations. To facilitate this next step, the other recommendation is to identify, regulate, and fund surgical research to sustainably improve the health system in an internally relevant manner.
As these efforts expand, modes of assessment can look to the objective presence of data systems that promote monitoring and accountability of access, quality and costs of surgical care. Even basic measures such as proportion of hospital facilities with high-speed internet connections may be a proxy measure of information management system development.
13. Conclusion
In the 18 months since the lancet commission on global surgery finalized its report there has been increasing action to improve surgical care worldwide. Stakeholders ranging from local professional societies, to national ministries of health, to international bodies such as the WHO and world bank are implementing the recommendations of the commission to varying degrees. Systems assessments, indicator collection, and national surgical planning processes are now developing around the world. The surgical patient is no longer the neglected stepchild of global health, rather action is being taken to ensure that they have access to surgical facilities, that the procedures they require are available, that they are not driven into poverty for receiving care, and that these changes are systemic and lasting. These steps will improve the lives of an estimated 5 billion people based upon the recognition of surgery’s indivisible and indispensable role in health.