1. Background
Since December 2019, Wuhan, Hubei of China, has experienced an outbreak of Coronavirus disease 2019 (COVID-19). The COVID-19 global pandemic has posed a severe threat to international health and the economy. Under such circumstances, clinicians are the main staff to fight against the epidemic. As a result, first-line medical staff from emergency departments, fever clinics, respiratory departments, and intensive care units (ICUs) have been associated with an increased risk of being infected. Similarly, medical staff from other clinical departments are also the high-risk population of infection. According to a study from Tongji Hospital, Wuhan, China (1), 72.2% of medical staff infected with COVID-19 were from non-first-line departments. Therefore, under the COVID-19 pandemic, medical staff from all clinical departments are at risk and under the stress of getting infected.
Previous studies during the SARS or Ebola epidemics indicate that a sudden major epidemic may cause great pressure on medical staff (2). Lacked understanding of the epidemic situation, increased workload, and the risk of family members getting infected may have a great influence on their physical and mental well-being, which brings a series of problems, such as fear, insomnia, and anxiety that may last for a long time (3, 4).
2. Objectives
Recently, Xiang et al. (5) demonstrated that only insufficient attention was paid to the mental health of medical staff under the COVID-19 epidemic, and that it was urgently needed to develop timely mental health services. In China, pediatricians are encountered with a heavy work burden and sensitive doctor-patient relationships, and may face greater challenges and mental stress. However, relevant studies are lacking at present. To this end this study aimed to analyze the mental stress and its influencing factors among pediatricians during the outbreak of COVID-19 in China, so as to provide a certain theoretical basis for psychological interventions among medical staff by the Department of Health under “public health emergencies”.
3. Methods
3.1. Research Subjects
In this cross-sectional study, a questionnaire survey was conducted among pediatricians from four specialist children’s hospitals and five general hospitals in Jiangsu province, China, from February 9, 2020, to February 13, 2020. Eligible pediatricians who were in service within the past month were enrolled, whereas those with previous mental illnesses or major illnesses within the past six months were excluded from the study. Altogether, 418 questionnaires were distributed, and those with less than 5% missing data were considered valid questionnaires. As a result, a total of 352 valid questionnaires were collected. The mean values were used to complete the missing data of the valid questionnaires. Of them, 240 collected questionnaires were from the specialist children’s hospitals, comprising of respiratory departments, infectious departments, outpatient and emergency departments (including fever clinics), ICUs, and other departments. Meanwhile, the remaining 112 questionnaires were collected from general hospitals and assigned to the general pediatric group. All participants were informed of the purpose of this study, and the study was approved by the Ethics Committee of the Children’s Hospital in Jiangsu, China (Approval #2020017).
3.2. Survey Methods
3.2.1. Survey Mode
The “SO JUMP” platform was applied in the Chinese anonymous online questionnaire survey. One investigator was selected from each hospital, who was responsible for informing the research subjects of the research objectives, organizing the training of questionnaire operation skills among the research subjects, and providing detailed explanations to the questions. The questionnaire would be independently completed within 20 minutes. A total of 352 valid questionnaires were collected in this study.
3.2.2. Basic Information Questionnaire
The questionnaire included gender, age, education, professional title, work experience, previous physical condition, living pattern, marital status, and the extent of the concern on COVID-19.
3.2.3. Measuring Tools
The Perceived Stress Scale (PSS-10, Cohen et al., 1983) (6) indicates the stress level in the past month. The Chinese adaptation of PSS-10 (7) was used to evaluate the perceived stress among individuals in this work. All 10 items were rated on a five-point scale, from 0 (never) to 4 (very often). The total score ranged from 0 to 40, and a higher score indicated greater perceived stress. To be specific, the PSS-10 score of 0 - 13 indicated mild stress, a score of 14 - 26 represented moderate stress, and a score of over 27 suggested severe stress. The PSS-10 score achieved acceptable reliability (the Cronbach coefficient = 0.70 - 0.91) and good structural validity (8).
Moreover, the Chinese adaptation of the Self-rating Anxiety Scale (SAS, Zung, 1971) (7, 9) was utilized to assess the subjective feelings of individuals with anxiety symptoms in the past week. The scale contained 20 items, and each item was divided into four grades, from 1 (no time or little time) to 4 (most time or all the time). The total score of 20 items was the rough score, which was multiplied by 1.25 to calculate the standard score. The SAS standard score of 50 - 59 indicated mild anxiety, a score of 60 - 69 suggested moderate anxiety, and a score of 69 or above was indicative of severe anxiety. The scale exhibited favorable reliability (Cronbach coefficient = 0.767) and good validity (10).
Besides, the Chinese adaptation of the Pittsburgh Sleep Quality Index Scale (PSQI, Buysse et al., 1989) (11, 12) was employed to assess the sleep quality of respondents in the past month. The scale contained 18 items, which were divided into seven dimensions: sleep quality, time to fall asleep, sleep time, sleep efficiency, sleep disorder, sleep medication, and daytime function. Each dimension was converted to 0 - 3 points according to the scoring standard, and the standard scores of all dimensions are added to the final score of the questionnaire. Specifically, a PSQI score of seven points or below indicated good sleep quality, while that of eight points or above suggested poor sleep quality. The PSQI scale showed good reliability (Cronbach coefficient = 0.845) and good validity (13).
3.3. Statistical Analysis
The SPSS23.0 software was used for statistical analysis. Enumeration data were expressed as frequency and percentage, whereas measurement data were presented as mean ± standard deviation (SD). The data conformed to the normal distribution or the homogeneity of variance. Therefore, the independent sample t-test was used for the comparison of perceived stress between the two groups, one-way analysis of variance (ANOVA) was employed for the comparison of perceived stress among multiple groups, and the least significant difference (LSD) test was used for comparisons among multiple groups. The correlations of perceived stress with anxiety level and sleep quality were analyzed by Pearson correlation analysis. Moreover, multiple linear regression analysis was adopted for multivariate analysis. A difference of P < 0.05 indicated statistical significance.
4. Results
4.1. General Information
A total of 352 valid questionnaires were collected in this study, with an effective recovery rate of 84.2%. There were 99 (28.1%) males and 253 (71.9%) females, among whom, 74 (21%) were aged 20 - 30 years, 195 (55.4%) aged 31 - 40 years, 55 (15.6%) aged 41 - 50 years, and 28 (7.9%) aged 50 years. In terms of education, 170 (48.3%) subjects were of bachelor's degrees or below, and the remaining 182 (51.7%) were of master's degrees or above (51.7%). In addition, 114 (32.4%) subjects had junior professional titles, 133 (37.8%) had intermediate professional titles, and 105 (29.8%) had senior professional titles. Concerning work experience, 91 (25.9%) worked for less than five years, 90 (25.6%) for 5 - 10 years, 83 (23.6%) for 10 - 15 years, and 88 (25.0%) for more than 15 years. In terms of living style, 31 (8.8%) lived alone, 293 (83.2%) lived with families, and 28 (8.0%) lived in collected dormitories provided by the hospitals. Besides, 68 (19.4%) were unmarried, 281 (79.8%) were married, and three (0.8%) were divorced. Regarding previous physical conditions, 110 (31.3%) were in an excellent physical condition, 161 (45.7%) in a good physical condition, 71 (20.2%) in a moderate physical condition, and 10 (2.8%) in a poor physical condition.
4.2. Concerns About COVID-19 Epidemic Among Pediatricians
Over the past one week, the average time spent on reading the COVID-19 epidemic information was more than three hours, one to three hours, and less than one hour a day in 102 (29.0%), 164 (46.6%), and 86 (24.4%) subjects, respectively.
4.3. Stress Status of Pediatricians from Various Departments
In 352 pediatricians from all departments, the average PSS-10 score was 14.28 ± 5.28, and they suffered from moderate stress on the whole. To be specific, the PSS-10 scores were ≥ 14 in 184 (52.3%) subjects and ≥ 27 in seven (2.0%) subjects. The PSS-10 scores of pediatricians from different departments are shown in Table 1. As observed, the perceived stress was significantly greater in pediatricians from outpatient and emergency departments than in those from the respiratory department and other inpatient departments (P < 0.05).
| Department | Respiratory Department | Infection Department | Outpatient and Emergency | Intensive Care Unit | Other Departments | General Pediatrics | In Total |
|---|---|---|---|---|---|---|---|
| Number of subjects | 30 | 34 | 48 | 38 | 90 | 112 | 352 |
| Score (mean ± SD) | 13.17 ± 4.44 | 14.18 ± 4.68 | 14.60 ± 4.57a | 14.45 ± 4.67 | 13.97 ± 5.78 | 14.55 ± 5.76 | 14.28 ± 5.28 |
| ≥ 14 points; No. (%) | 12 (40.0) | 20 (58.8) | 27 (56.2) | 17 (44.7) | 46 (51.1) | 62 (55.4) | 184 (52.3) |
Perceived Stress of Pediatricians from Different Departments a
4.4. Analysis of Relevant Factors of Perceived Stress Among Pediatricians
The perceived stress scores of all participants were grouped and analyzed according to the general information. Differences in age, education, professional title, work experience, and physical condition were statistically significant among different groups. Moreover, the perceived stress was higher in pediatricians aged 31 - 40 years than in those aged 41 - 50 years or over 51 years, and the difference was statistically significant (P < 0.05). Pediatricians with bachelor’s degrees or below had significantly higher perceived stress scores than those with master's degrees or above (P < 0.05). The perceived stress in pediatricians with intermediate professional titles was significantly greater than that in pediatricians with junior or senior professional titles (P < 0.05). Pediatricians with work experience of 10 - 15 years had a higher perceived stress level than those with work experience of 0 - 5 years or over 15 years (P < 0.05). Further, there was a significant difference in the perceived stress level among the groups with different physical conditions (P < 0.05), and pediatricians with poor physical conditions had higher perceived stress. However, gender, marital status, and living pattern did not significantly affect the perceived stress (P > 0.05) (Table 2).
| Items and Category | Number (Constituent Ratio) | PSS-10 Score (Mean ± SD) | Statistics; t/F | P-Value |
|---|---|---|---|---|
| Gender | t = 0.365 | 0.715 | ||
| Male | 99 (28.1) | 14.11 ± 4.83 | ||
| Female | 253 (71.9) | 14.40 ± 5.46 | ||
| Age (y) a | F = 4.737 | 0.003 | ||
| 20 - 30 | 74 (21.0) | 14.16 ± 5.44 | ||
| 31 - 40 | 195 (55.4) | 15.04 ± 5.19 b | ||
| 41 - 50 | 55 (15.6) | 13.05 ± 5.27 | ||
| Over 50 | 28 (7.9) | 11.68 ± 4.39 | ||
| Educational level a | t = 2.133 | 0.034 | ||
| Bachelor degree or below | 170 (48.3) | 14.89 ± 5.46 | ||
| Master degree or above | 182 (51.7) | 13.70 ± 5.06 | ||
| Professional title a | F = 4.239 | 0.015 | ||
| Junior | 114 (32.4) | 13.83 ± 5.18 | ||
| Intermediate | 133 (37.8) | 15.30 ± 5.14 c | ||
| Senior | 105 (29.8) | 13.46 ± 5.42 | ||
| Work experience (y) a | F = 4.137 | 0.007 | ||
| 0 - 5 | 91 (25.9) | 13.59 ± 5.21 | ||
| 5 - 10 | 90 (25.6) | 15.04 ± 4.85 | ||
| 10 - 15 | 83 (23.6) | 15.46 ± 5.72 d | ||
| Over 15 | 88 (25.0) | 13.08 ± 5.08 | ||
| Living style | F = 0.454 | 0.636 | ||
| Living alone | 31 (8.8) | 15.06 ± 5.74 | ||
| Living with family | 293 (83.2) | 14.16 ± 5.18 | ||
| Collective dormitory | 28 (8.0) | 14.57 ± 5.90 | ||
| Marital status | F = 0.584 | 0.558 | ||
| Unmarried | 68 (19.4) | 14.68 ± 5.55 | ||
| Married | 281 (79.8) | 14.21 ± 5.22 | ||
| Divorced | 3 (0.8) | 11.67 ± 5.51 | ||
| Physical condition a | F = 12.476 | < 0.001 | ||
| Excellent | 110 (31.3) | 12.11 ± 5.02 e | ||
| Good | 161 (45.7) | 14.78 ± 4.77 e | ||
| Moderate | 71 (20.2) | 15.83 ± 5.76 e | ||
| Poor | 10 (2.8) | 19.00 ± 3.80 e |
Comparison of Perceived Stress Among Pediatricians
4.5. Anxiety Level and Sleep Status Among Pediatricians
Under the COVID-19 epidemic, the SAS score in pediatricians was 38.72 ± 9.47, of whom, 39 (11.1%) had mild anxiety, seven (2.0%) had moderate anxiety, and four (1.1%) had severe anxiety. The average sleep time of pediatricians was 6.06 ± 0.76 h, and the average PSQI score in pediatricians was 6.98 ± 3.52. Of them, 106 (30.1%) subjects had a total score of ≥ 8 (poor sleep quality), 188 (53.4%) had difficulty in falling asleep at least once a week, and 17 (4.8%) took hypnotic drugs at least once a week.
4.6. Correlation Analysis of Stress with Anxiety Level and Sleep Status Among Pediatricians
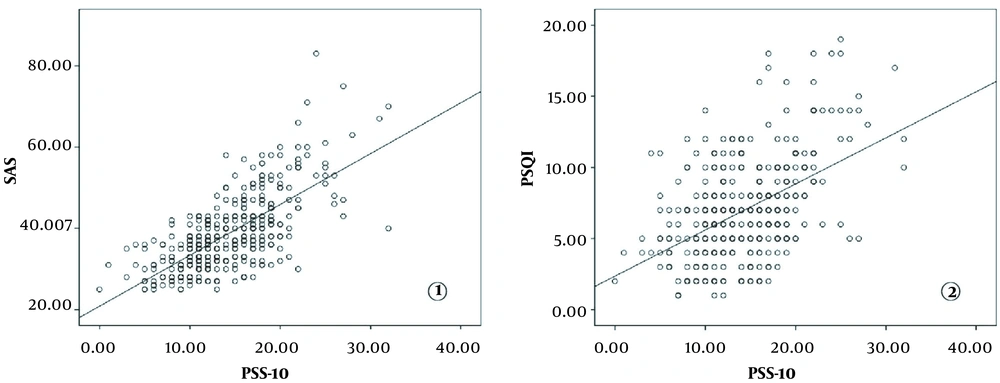
Pearson linear correlation analysis was conducted to analyze the correlation of perceived stress with the anxiety level and sleep quality among pediatricians. As a result, the total PSS-10 score was positively correlated with the SAS score (r = 0.698) (Figure 1), indicating that greater stress was correlated with higher anxiety levels. In addition, the total PSS-10 score was positively correlated with the total PSQI score (r = 0.487) (Figure 1), revealing that greater stress was correlated with a higher PSQI score, namely, worse sleep quality.
Correlation analysis of PSS-10 with SAS and PSQI in pediatricians (PSS-10, Perceived Stress Scale; SAS, Self-rating Anxiety Scale; and PSQI, Pittsburgh Sleep Quality Index). 1, the total PSS-10 score was positively correlated with SAS score (r = 0.698); 2, the total PSS-10 score was positively correlated with the total PSQI score (r = 0.487).
4.7. Regression Analysis on Relevant Factors of Perceived Stress Among Pediatricians
Five significant dimensions obtained from one-way ANOVA, including age, education, professional title, work experience, and physical condition, were used as independent variables, whereas the PSS-10 score was utilized as the dependent variable for multiple linear regression analysis. Moreover, stepwise multiple linear regression indicated that age, professional title, and physical condition all had a linear relationship with the individual’s perceived stress (P < 0.05), as shown in Table 3.
| Variables | B | SE | β | T-Value | P-Value |
|---|---|---|---|---|---|
| Constant | 11.067 | 1.769 | 6.254 | < 0.001 | |
| Age | -1.932 | 0.487 | -0.347 | -3.965 | < 0.001 |
| Education | -1.065 | 0.571 | -0.141 | -1.866 | 0.063 |
| Professional title | 1.074 | 0.611 | 0.152 | 1.758 | 0.034 |
| Work experience | 1.016 | 0.464 | 0.078 | 0.649 | 0.517 |
| Physical condition | 1.677 | 0.365 | 0.288 | 4.599 | < 0.001 |
Multiple Linear Regression Analysis of Influencing Factors on Perceived Stress
5. Discussion
The COVID-19 epidemic is the most serious international public health emergency currently. Clinicians are at a high risk of infection, and they may experience various mental health problems, such as panic, great mental stress, anxiety, and sleep disorders. Besides, after the outbreak of public health emergencies, such as SARS, part of medical staff are still burdened with mental problems (2, 14), which may thus affect their work efficiency and interpersonal relationships. Therefore, it is important to understand the mental stress experienced by clinicians during the epidemic.
In this study, a questionnaire survey was conducted during the outbreak of COVID-19 in China, and data on the mental stress, anxiety, and sleep status of 352 pediatricians were subsequently collected. According to our results, 75.6% of the 352 pediatricians were highly concerned about the epidemic and browsed the epidemic information for at least one to three hours or more every day. Besides, the perceived stress of these 352 pediatricians was at a moderate level.
As known, COVID-19 is highly contagious, and physicians are at risk of infection during the diagnosis and treatment processes. According to data reported from a study published in February 2020 (3, 15), 3,019 medical staff in China were infected with COVID-19 (including 1,716 confirmed cases). Although pediatric COVID-19 cases account for less than 2.0% of the total number of cases in China, the onset of pediatric cases is insidious, with atypical clinical manifestations. Moreover, misdiagnosis or missed diagnosis may occur in the process of consultation. As a result, pediatricians are at a high risk of occupational exposure. In addition, the high-risk factors readily exist in pediatrics per se, such as difficulty in inquiring the medical history, inadequate examinations on infants and young children, and harsh communication with parents under the currently sensitive doctor-patient relationship in China, all of which can aggravate the mental stress of pediatricians.
In this study, various factors were found to affect the mental stress level of pediatricians under the COVID-19 epidemic. As the first line of defense against the epidemic, pediatricians from outpatient and emergency departments are responsible for pre-diagnosis screening and fever diagnosis in the affected children. Therefore, pediatricians from outpatient and emergency departments suffer from higher mental stress than those at respiratory departments or other inpatient departments. According to our results, pediatricians with bachelor's degrees or below experienced greater mental stress than those with master’s degrees or above. This is because the highly educated pediatricians have higher professional knowledge levels, greater capacities in clinical diagnosis and identification, and thus lower mental stress. Besides, the perceived stress in pediatricians with intermediate professional titles was also higher. Under the COVID-19 epidemic, attending physicians play an important role in clinical practice and are responsible for most of the screening duties in fever clinics, checking out the epidemic situation among patients admitted to the inpatient departments, and coordinating the deployment of medical staff in the department; as a result, they have a higher stress level.
Moreover, the results of our study provided evidence of a negative linear relationship between the age of pediatricians and stress levels. Previous studies have shown that the stress level tends to decrease with age, and older people are less affected by stress than younger people (16). On the other hand, older pediatricians have enriched clinical experience and management experience, and most of them have left the clinical front-line. Our study warns that we cannot neglect the mental health condition of younger pediatricians, as they seem to be the most stressed during the COVID-19 outbreak. In this study, subjects with poor physical fitness had higher levels of mental stress. Among the COVID-19-infected patients, those with chronic concurrent diseases have a poor prognosis, which may increase the panic among pediatricians with poor physical conditions. Thus, we need to provide more reasonable rest arrangements and psychological counseling to pediatricians with poor physical conditions to relieve their mental pressure.
Living alone has been previously linked to higher indices of depression and anxiety, and other common mental disorders (17). But in our study, the living style did not make any difference to mental stress. It is possible that many of those who live alone use social media to maintain high levels of connections with their families or friends. Although a recent study (18) in 26 countries indicates that women report greater levels of stress during the COVID-19 situation, our study found gender to be unrelated to stress levels. It is possible that, in China, male and female pediatricians assume almost the same intensity of clinical work, and also in families, both fathers and mothers will take care of children and home. The ratio of male to female pediatricians in China is uneven, with female dominance, and this may cause bias in sample selection. A recent study shows that married individuals experience lower levels of stress than single individuals (18), while in our study, marital status did not make any difference to mental stress. This may be because part of married couples in China works in different cities.
The anxiety level and sleep status are correlated with stress levels among pediatricians. Under the COVID-19 epidemic, the SAS score in pediatricians is higher than the normal standard in the Chinese population. To be specific, 14.2% of physicians have anxiety tendencies, which is higher than the incidence of anxiety among the Chinese population (2, 19). Upon Pearson linear correlation analysis, the anxiety level was positively correlated with the stress level in pediatricians (r = 0.698). We speculate that excessive stress causes increased anxiety levels. Meanwhile, individuals who are prone to anxiety may also have excessively conscious pressure under stress. Therefore, the high-stress level is closely correlated with the anxiety level. The average daily sleep time of pediatricians was 6.06 h, less than the average daily sleep time of 6.78 h among the Chinese medical staff reported in 2019 (4, 20). In this study, 30.1% of pediatricians had poor sleep quality and over one-half of them had difficulty in falling asleep. Moreover, Pearson's linear correlation analysis also revealed that sleep quality was positively correlated with stress level. As reported by some studies, the increased mental stress causes the regulatory dysfunction of the hypothalamic-pituitary-adrenal axis, thereby affecting sleep quality (2, 21). Furthermore, poor sleep quality also reversely increases mental stress, thereby causing a vicious circle of high perceived stress and poor sleep quality. In addition, the anxiety symptoms are generally accompanied by physiologically and consciously high arousal states, which is also closely related to sleep disorders (2, 22). In summary, the stress level, anxiety level, and sleep quality interact with and affect each other.
Both medical institutions and society should pay attention to the mental stress issue of pediatricians under public health emergencies. Our findings in this study can provide certain guidance and suggestions on relevant psychological interventions: under the COVID-19 epidemic, professional psychological counseling should be performed and humanistic care should be strengthened for physicians at outpatient and emergency departments. In addition, the training of epidemic prevention and control should be reinforced on physicians with lower education. Moreover, rotation to the outpatient and emergency departments should be avoided among physicians with poor physical conditions, while the rotational schedule should be executed to ensure high-quality rest and sleep, so as to better respond to the clinical burden and to maximally avoid mental problems among physicians after the outbreak. However, this study was conducted only based on several hospitals from Jiangsu province with a relatively small sample size, and data on the general stress levels of pediatricians are still lacking. After the global pandemic is over, changes in the stress levels of pediatricians can be followed up.
5.1. Conclusion
Our study showed that under the global COVID-19 epidemic, Chinese pediatricians experience great psychological stress, and the stress experienced by outpatient and emergency pediatricians is greater than the stress perceived by inpatient pediatricians. The factors affecting the stress of pediatricians included educational background, age, professional title, working years, and physical quality. In addition, pediatrician anxiety levels and sleep quality were associated with the psychological stress of pediatricians. Our findings are helpful to provide reasonable guidance and suggestions for scientific psychological interventions for pediatricians in the face of international public health emergencies.