Dear editor,
From December 2019, the novel coronavirus, SARS COV-2, spread rapidly from China to the rest of the world, including Iran. There have been studies on the prevalence of neonatal and maternal complications of COVID-19 (1-4).
Relatively high rates of fetal distress and NICU admissions have also been reported on recent systematic reviews of the existing literature (5-8). A small number of studies have shown that the increased risk of preterm labor is more common in affected mothers (9, 10).
We conducted the study to clarify the clinical features and obstetrics and neonatal outcomes of pregnant patients with COVID-19. In this case-series, single-centre study, we aimed to assess all patients suspected of COVID-19 who were admitted to the Imam Sajjad Hospital, a referral hospital in Shahriar City of Tehran Province, from March to the end of September 2020. According to clinical, laboratory, and radiologic findings, 42 pregnant women suspected of COVID-19 undergoing vaginal delivery or cesarean section were detected by internist physician.
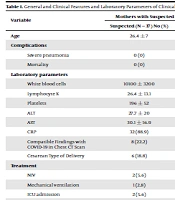
COVID-19 was confirmed in five pregnant women out of 42 suspected cases (Table 1). The percentage of need for mothers to be admitted to the ICU was 5.6%, showing an increase compared to that at the same time interval (six months) last year, which was 0.4%.
The preterm delivery rate was 9.4% in the suspected group (PCR negative group), 0% in the affected group (PCR positive group), and 8.3% in total, which increased compared to the preterm labor rate at the same time interval last year (4.64%). However, the LBW rate was 2.8%, which was lower than that at the same time interval last year (3.55%). We had only one positive PCR test of the neonate, which was positive after 36 hours of birth. However, there was no higher mortality rate or hospitalization in the NICU.
Our study showed an increased risk of preterm labor in neonates of the suspected mothers compared to that at the same time interval last year before the COVID-19 pandemic. Higher rates of preterm delivery can also be considered consequences of a maternal complication in the suspected mothers or because of the possibility of disease transmission from mother to fetus, which is unknown and requires more studies with a larger population (11, 12).
| Variable | Mothers with Suspected or Confirmed COVID-19 | Mothers with Confirmed COVID-19 | |||||
|---|---|---|---|---|---|---|---|
| Suspected (N = 37), No (%) | Confirmed (N = 5), No (%) | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
| Age | 26.4 ± 7 | 31.2 ± 6.3 | 34 | 23 | 35 | 26 | 38 |
| Complications | |||||||
| Severe pneumonia | 0 (0) | 0 (0) | no | no | no | no | no |
| Mortality | 0 (0) | 0 (0) | no | no | no | no | no |
| Laboratory parameters | |||||||
| White blood cells | 10100 ± 3200 | 7900 ± 1300 | 8400 | 6600 | 8000 | 9900 | 6700 |
| Lymphocyte % | 26.4 ± 13.1 | 31.2 ± 6.1 | 40 | 25 | 31 | 34 | 26 |
| Platelets | 196 ± 52 | 232 ± 83 | 280 | 129 | 340 | 237 | 177 |
| ALT | 27.7 ± 20 | 17 ± 9.6 | - | 24 | 16 | - | 21 |
| AST | 30.1 ± 16.9 | 19.6 ± 10.9 | - | 32 | 11 | - | 16 |
| CRP | 32 (88.9) | 3 (60) | 2+ | 3+ | 3+ | neg | neg |
| Compatible Findings with COVID-19 in Chest CT Scan | 8 (22.2) | 2 (40) | no | yes | yes | no | no |
| Cesarean Type of Delivery | 6 (18.8) | 1 (25) | - | No | no | no | yes |
| Treatment | |||||||
| NIV | 2 (5.6) | 0 (0) | no | no | no | no | no |
| Mechanical ventilation | 1 (2.8) | 0 (0) | no | no | no | no | no |
| ICU admission | 2 (5.6) | 0 (0) | no | no | no | no | no |
| Neonatal features | |||||||
| IUFD | 0 (0) | 0 (0) | no | no | no | no | no |
| PTL | 3 (9.4) | 0 (0) | no | no | no | no | no |
| LBW | 1 (3.1) | 0 (0) | no | no | no | no | no |
| NICU admission | 4 (12.5) | 1 (25) | no | no | no | no | yes |
| Pneumonia | 0 (0) | 0 (0) | no | no | no | no | no |
| Fever | 0 (0) | 0 (0) | no | no | no | no | no |
| Mortality | 0 (0) | 0 (0) | no | no | no | no | no |
General and Clinical Features and Laboratory Parameters of Clinically Suspected or Confirmed Mothers for COVID-19