1. Background
The coronavirus disease 2019 (COVID-19) is an infected disease with a long commune period that has affected 213 countries (1). As of November 8th, 2020, a total of 10,185,012 cases in the United States and 673,250 cases in Iran have been reported, increasing day by day (2). The review of epidemiologic studies has shown that epidemic infections can influence a wide range of people, communities, and international areas and cause psychological problems, including fear of getting sick, feeling of helplessness, and social exclusion that can increase the stress level in the society (3, 4).
Although mental health-related studies are limited regarding patients with COVID-19, many researchers emphasize that it is possible to predict expected mental and physical health outcomes in the vulnerable population (5). In this regard, evaluation of severe and acute respiratory syndrome (SARS) showed that younger people, including children, are more likely to be affected by psychological problems (6). The main factors that can increase the risk of stress in children during the outbreaks such as COVID-19 are school closures, home quarantines, home-schooling, or worrying about parents' death resulting from infection (7). Due to these fundamental changes in the environment, children may experience social isolation, child neglect or child abuse, and domestic violence that can cause psychological problems in the future (8). Studies have also shown that even children as young as two years old are aware of what is happening in their environment (9). Since the COVID-19 outbreak has created much tension among families and communities, and children and adolescents are more inclined to use virtual media due to quarantine conditions, they are quickly exposed to large amounts of information and high levels of adult stress and anxiety (10). On the other hand, timely identification of children’s and adolescents’ symptoms of stress can help parents and the health care system prevent serious physical, mental, and social injuries in adulthood.
The literature review showed that most studies related to the COVID-19 outbreak paid more attention to physical problems. Furthermore, there were significant gaps in the literature on the mental health consequences for children and the youth during COVID-19 (11), while psychological problems of children and adolescents, as a vulnerable population, have been neglected by families and the health care system; thus, it seems necessary to assess symptoms of stress in this age group.
2. Objectives
Since recent Iranian studies have paid less attention to children and adolescents and their psychological needs in this outbreak, this study aimed to evaluate the frequency and severity of stress symptoms and associated factors amongst children and adolescents aged 4 - 18 years during the early phase of COVID-19 outbreak in Shiraz, Iran. Therefore, this study represents the psychological impacts on children and adolescents within the first four months of the COVID-19 outbreak.
3. Methods
This descriptive-analytic cross-sectional study was conducted on children and adolescents in Shiraz, Iran using an anonymous online questionnaire during the first four months of the COVID-19 outbreak from March 2020 to June 2020.
The inclusion criteria were children and adolescents aged 4 - 18 years, without physical and mental disability, and having literate parents familiar with using mobile phones and virtual media. The participants who did not answer more than 10% of the questionnaires' items (12) or their age was less than four or higher than 18 years were excluded.
The samples were selected using a convenient and purposeful sampling method. The sample size was calculated using PASS software version 15 based on a previous study (13). Before data collection, permission was obtained from the local ethics committee. After that, the researcher referred to the recruitment department of the university and the main health centers in Shiraz, Iran. The eligible samples were selected according to the records in the health centers and inclusion criteria. First, the phone numbers of eligible people were extracted from the recodes of health centers and university personnel. Then, the online link of the electronic questionnaire was sent to 471 eligible people via SMS and WhatsApp. At the beginning of the online questionnaire, the study aims and the way of answering the questions were explained. Parents or their children were requested to answer all questions accurately. Finally, 363 questionnaires were included in the study (response rate = 73.48%)
This questionnaire included two sections, including cognitive-emotional (11 items) and physical symptoms (13 items). Cognitive-emotional variables included madness, worrying, crying, early agitation, being afraid, bad temper, no clear thoughts, thinking about death, desire to hit someone, embarrassment and shame, and feeling weird. Physical symptoms variables included headache, stomach-ache, sweating, fast heart beating, feeling unwell, chills, tiredness, muscle stiffness, face blushing and warmness, weakness, skin rash, cold feeling, and hunger. Sharrer and Ryan-Wenger (14) designed this tool to evaluate school-age children's self-reported stress symptoms, scored by yes/no questions [yes = presence of symptom (1) and no = lack of symptom (0)].
Two items of ‘having nausea and vomiting’ and ‘feeling sad’ were added by Valizadeh et al. (13), (26 items). Their study approved the translated version, and content validity and test-retest reliability coefficients calculated reliability as 0.76. The scores related to stress symptoms ranged from zero to 26, and the presence of stress symptoms was reported at three levels: low (having ≤ 8 stress symptoms), medium (having 9 - 13 stress symptoms), and high (having ≥ 18 stress symptoms). The reliability of the questionnaire was also confirmed in another study with an alpha coefficient of 0.88 (15). Moreover, demographic data, including gender, age group, education level, parents' job, residential location, economic status, and duration of the quarantine were collected.
As the Iranian government recommended the public to minimize face-to-face interaction, observe social distancing, and quarantine themselves at home, the potential respondents were electronically invited. The questionnaire was completed by parents or adolescents through an online survey platform.
3.1. Statistical Analyses
The data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) for Windows (version 21). Descriptive statistics such as frequency and percent were calculated for reporting demographic characteristics of participants, cognitive-emotional symptoms, physical symptoms variables, and severity of stress. Percentages of responses were calculated according to the number of respondents per response concerning the number of total responses to a question. The chi-square test was used to calculate the relationship between demographic characteristics with cognitive-emotional symptoms and physical symptoms variables and demographic characteristics with the severity of stress. A P-value equal to 0.05 was considered as significant. Also, we used the STROBE cross sectional reporting guidelines (16).
4. Results
The research population included 363 children and adolescents aged 4 - 18 years who completed the online questionnaire during the first four months of the COVID-19 outbreak in Shiraz and other parts of Fars province in Iran. Most of the samples were female (57%) and lived with both parents (91.2%). Based on the age group, 132 (36.4%) cases were in the age range of 4 - 7 years, 128 (35.3%) cases in the age range of 8-11 years, and 103 (28.4%) cases in the age range of 12 - 18 years.
According to the birth rank, 134 (36.9%) cases were the first child, 85 (23.4%) cases were the second child, 17 (4.7%) cases were the third child and more, and 127 (35%) cases were a single child.
Also, 238 (65.6%) cases lived in Shiraz, 110 (30.3%) cases lived in other towns of the Fars province, and 15 (4.1%) cases lived in the rural areas. Table 1 shows the frequency of other demographic data of the participants.
| Variables and Items | No. (%) |
|---|---|
| Gender | |
| Female | 156 (43) |
| Male | 207 (57) |
| Age group (Y/O) | |
| 4 - 7 | 132 (36.4) |
| 8 - 11 | 128 (35.3) |
| 12 - 18 | 103 (28.4) |
| Birth rank | |
| Only child | 127 (35) |
| The first child | 134 (36.9) |
| The second child | 85 (23.4) |
| ≥ The third child | 17 (4.7) |
| Location of living | |
| Shiraz | 238 (65.6) |
| Other town of Fars | 110 (30.3) |
| Village | 15 (4.1) |
| Economic status | |
| Poor | 17 (4.7) |
| Moderate | 181 (49.9) |
| Good | 152 (41.9) |
| Very good | 13 (3.6) |
| Mother’s job | |
| Self-employment | 30 (8.3) |
| Employee | 126 (34.7) |
| housekeeper | 207 (57) |
| Father’s job | |
| Employee | 147 (40.5) |
| Worker | 32 (8.8) |
| Self-employment | 149 (41) |
| Others | 35 (9.6) |
| Workplace of mother | |
| Hospital | 77 (21.2) |
| University of medical sciences | 22 (6.1) |
| Government agencies | 22 (6.1) |
| Private agencies | 31 (8.5) |
| None | 211 (58.1) |
| Workplace of father | |
| Hospital | 19 (5.2) |
| University of medical sciences | 10 (2.8) |
| Government agencies | 93 (25.6) |
| Private agencies | 86 (23.7) |
| None | 155 (42.7) |
| Education level of mother | |
| Elementary | 11 (3) |
| Middle school | 17 (4.7) |
| Diploma | 94 (25.9) |
| 2-years Associate Degree | 30 (8.3) |
| Bachelor’s Degree | 158 (43.5) |
| ≥ Master’s Degree | 53 (14.6) |
| Education level of father | |
| Elementary | 18 (5) |
| Middle school | 35 (9.6) |
| Diploma | 105 (28.9) |
| 2-years associate degree | 27 (7.4) |
| Bachelor’s degree | 108 (29.8) |
| ≥ Master’s degree | 70 (19.3) |
| Total | 363 (100) |
According to our results, 85 (23.4%) cases stayed at home for 30 days, 60 (16.5%) cases for 45 days, 112 (30.9%) cases for 60 days, and 60 (16.5%) cases for two months and more during the COVID-19 quarantine. During this study, COVID-19 infected none of the participants, and only five participants (1.4%) reported that one of their relatives had been infected with the virus.
All the 26 items of the questionnaire were mentioned by the subjects as stress symptoms. Our results revealed that 270 (74.4%) cases had low stress, 77 (21.2%) cases had moderate stress, and 16 (4.4%) cases had severe stress. In this regard, age group, living with both parents, and birth rank had a significant relationship with the degree of stress (P < 0.05).
Our findings showed that more than 50% of participants reported worrying, anger, and weakness as symptoms of stress. Furthermore, sadness, no clear thoughts, and physical symptoms of stress, including tiredness and muscle stiffness, were reported by 37.2%, 35.8%, and 35% of participants, respectively. Chills (3.9%), cold feeling (5%), fast heart beating (8.8%), face blushing and warmness (9.1%), embarrassment and shame (11%), sweating (14%), thinking about death (16.3%), headache (16.5%), and hunger (16.5%) were the least reported symptoms of stress (Table 2).
| Items | No. (%) | |
|---|---|---|
| Stress Symptom | No Stress Symptom | |
| Madness | 146 (40.12) | 217 (59.8) |
| Worrying | 214 (59) | 149 (41) |
| Crying | 87 (24) | 276 (76) |
| Early agitation | 217 (59.8) | 146 (40.2) |
| Being afraid | 155 (42.7) | 208 (57.3) |
| Bad temper | 190 (52.3) | 173 (47.7) |
| No clear thoughts | 130 (35.8) | 233 (64.2) |
| Thinking about death | 59 (16.3) | 304 (83.7) |
| Desire to hit someone | 94 (25.9) | 269 (94) |
| Embarrassment and shame | 40 (11) | 323 (89) |
| Feeling weird | 88 (24.2) | 275 (75.8) |
| Sadness | 135 (37.2) | 228 (62.8) |
| Headache | 60 (16.5) | 303 (83.5) |
| Stomach-ache | 72 (19.8) | 291 (80.2) |
| Sweating | 51 (14) | 312 (86) |
| Fast heart beating | 32 (8.8) | 331 (91.2) |
| Feeling unwell | 93 (25.6) | 270 (74.4) |
| Chills | 14 (3.9) | 349 (96.1) |
| Tiredness | 127 (35) | 236 (65) |
| Muscle stiffness | 127 (35) | 236 (65) |
| Face blushing and warmness | 33 (9.1) | 330 (90.9) |
| Weakness | 209 (57.6) | 154 (42.4) |
| Skin rash | 93 (25.6) | 270 (74.4) |
| Feeling cold | 18 (5) | 345 (95) |
| Hunger | 60 (16.5) | 303 (83.5) |
| Nausea and vomiting | 77 (21.2) | 286 (78.8) |
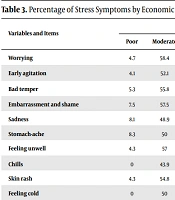
Chi-square showed a significant relationship between symptoms of stress and some demographic variables. There was a significant relationship between chilling and cold feelings with gender, so it was higher in males (P < 0.05). Furthermore, bad temper and sadness had a significant relationship with the duration of quarantine (P < 0.05). Also, there was a significant relationship between no clear thoughts with the mother's workplace and the father's job (P < 0.05). The mother's education level was significantly related to feeling weird (P < 0.05). Tables 3 and 4 show the significant relationships between other symptoms of stress with economic status, birth rank, residential location, education level of the father, and age group (P < 0.05).
| Variables and Items | Economic status | Birth rank | Residential location | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Poor | Moderate | Good | Very good | P* | Only child | First | Second | ≥Third | P* | Shiraz | Fars | Village | P* | |
| Worrying | 4.7 | 58.4 | 35.5 | 1.4 | < 0.001 | 30.8 | 40.7 | 24.8 | 3.7 | 0.115 | 64 | 30.4 | 5.6 | 0.23 |
| Early agitation | 4.1 | 52.1 | 41 | 2.8 | 0.58 | 29.5 | 43.3 | 24 | 3.2 | 0.004 | 65 | 30.9 | 4.1 | 0.95 |
| Bad temper | 5.3 | 55.8 | 37.9 | 1.1 | 0.008 | 26.8 | 42.1 | 26.3 | 4.7 | 0.008 | 64.2 | 31.1 | 4.7 | 0.764 |
| Embarrassment and shame | 7.5 | 57.5 | 35 | 0 | 0.333 | 15 | 62.5 | 15 | 7.5 | 0.002 | 62.5 | 30 | 7.5 | 0.522 |
| Sadness | 8.1 | 48.9 | 41.9 | 3.6 | 0.042 | 31.9 | 37 | 25.2 | 5.9 | 0.659 | 69.6 | 25.9 | 4.4 | 0.377 |
| Stomach-ache | 8.3 | 50 | 40.3 | 1.4 | 0.091 | 25 | 47.2 | 23.6 | 4.2 | 0.158 | 689.1 | 22.2 | 9.7 | 0.012 |
| Feeling unwell | 4.3 | 57 | 37.6 | 1.1 | 0.257 | 23.7 | 47.3 | 25.8 | 3.2 | 0.028 | 64.5 | 32.3 | 3.2 | 0.808 |
| Chills | 0 | 43.9 | 57.1 | 0 | 0.54 | 14.3 | 57.1 | 21.4 | 7.1 | 0.307 | 57.1 | 21.4 | 21.4 | 0.004 |
| Skin rash | 4.3 | 54.8 | 39.8 | 1.1 | 0.394 | 23.7 | 47.3 | 25.8 | 3.2 | 0.028 | 64.5 | 32.3 | 3.2 | 0.808 |
| Feeling cold | 0 | 50 | 50 | 0 | 0.409 | 16.7 | 55.6 | 22.2 | 5.6 | 0.565 | 55.6 | 22.2 | 22.2 | < 0.001 |
a P < 0.05 at chi square correlation.
| Variables and Items | Education Level of Father | Age Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Elementary | Middle School | Diploma | 2-Years Associate Degree | Bachelor Degree | ≥ Master | P* | 4 - 7 | 8 - 11 | 12 - 18 | P a | |
| Early agitation | 2.8 | 11.1 | 34.1 | 6.5 | 29 | 16.6 | 0.01 | 35.3 | 34.7 | 30 | 0.170 |
| Desire to hit someone | 5.3 | 7.4 | 33 | 4.3 | 33 | 17 | 0.565 | 47.9 | 29.8 | 22.3 | 0.026 |
| Sadness | 5.2 | 10.4 | 38.5 | 4.4 | 26.7 | 8.1 | 0.029 | 27.4 | 37 | 35.6 | 0.012 |
| Sweating | 7.8 | 9.8 | 37.3 | 9.8 | 25.5 | 9.8 | 0.307 | 18.8 | 28.1 | 53.1 | < 0.001 |
| Fast heart beating | 0 | 9.4 | 40.6 | 9.4 | 25 | 15.6 | 0.536 | 18.8 | 28.1 | 53.1 | 0.004 |
| Feeling unwell | 3.2 | 6.5 | 37.6 | 4.3 | 33.3 | 15.1 | 0.121 | 28 | 34.4 | 37.6 | 0.044 |
| Chills | 7.1 | 7.1 | 35.7 | 14.3 | 28.6 | 7.1 | 0.776 | 7.1 | 42.9 | 50 | 0.048 |
| Face blushing and warmness | 0 | 9.1 | 39.4 | 6.1 | 27.3 | 18.2 | 0.642 | 18.2 | 33.3 | 48.5 | 0.014 |
| Weakness | 2.9 | 11 | 34.3 | 6.2 | 28.2 | 17.2 | 0.024 | 41.1 | 30.6 | 28.2 | 0.047 |
| Hunger | 5 | 11.7 | 41.7 | 3.3 | 31.7 | 6.7 | 0.035 | 18.3 | 35 | 46.7 | 0.001 |
a P < 0.05 at chi-square correlation.
5. Discussion
The present study evaluated the frequency and severity of stress symptoms and associated demographic factors in children and adolescents aged 4 - 18 years during the COVID-19 outbreak in Shiraz, Iran. According to the results, children were worried about this unknown disease and the probability of their parents’ death resulting from the disease (17).
In this study, all the 26 items of the questionnaire were reported as symptoms of stress by children and adolescents. The symptoms of stress were classified into cognitive-emotional and physical symptoms. Our results revealed that participants had experienced cognitive-emotional symptoms more than physical ones. More than 50% of participants reported symptoms, including worrying, anger, and bad temper, and more than 35% of them reported sadness and no clear thoughts. These results are consistent with the findings of an Iranian study in terms of reporting worrying and sadness as the most common cognitive-emotional symptoms of stress in children (13). In addition, the Center for Diseases Control and Prevention (CDC) stated that children show symptoms such as excessive worrying or sadness, crying or irritation, irritability etc., during the COVID-19 outbreak (18).
The present study showed that the least symptoms that pediatric cases reported were related to physical ones, including cold feeling, chilling, fast heart beating, face flushing, sweating, hunger, etc. On the contrary, a study showed that physical symptoms such as headache and stomach-ache were the most common symptoms of stress in children (19). Another study also approved the physical symptoms of stress (20). These controversies can be related to the unique situation of the COVID-19 outbreak because this unknown disease with high transmissibility and mortality has caused a great deal of panic and fear in the communities. In our study, weakness, unwell feeling, skin rash, nausea and vomiting, and stomach-ache were identified as the most common physical symptoms of stress. Since stress can be the main factor causing many psychosomatic diseases, especially during the pandemic, the parents and caregivers are suggested to pay more attention to children's mental health.
Frequency and severity of physical symptoms of stress had a significant relationship with the age group, such that older children showed more physical symptoms of stress. As other studies showed that children are aware of their surroundings even from two years (9), it seems essential that parents inform their children based on their age. This effective relationship can benefit children and even their families to improve their psychological well-being during the outbreak.
A previous study showed that children aged 4 - 7 years have magical thinking so that their thoughts and beliefs can cause an external event such as a disease (21). Our findings revealed that participants aged 4 - 7 years reported feeling weird more than other age groups. Thus, adults should help the children to refrain from blaming themselves during illness or not consider their illness as a punishment for their destructive behaviors. On the other hand, in the COVID-19 outbreak, the parents have an essential role in protecting children from stress and preventing negative emotions.
Quarantine and its psychological effects are other problems resulting from COVID-19. Parents' involvement with the consequences of COVID-19 may cause them to ignore to respond to their children's distress timely. On the other hand, children may show challenging external behaviors such as fight instead of routine responses to stress (22). Our results showed that children who spent more time at home quarantine reported more cognitive-emotional symptoms of stress, including bad temper, sadness, and a tendency to fight. In this regard, the World Health Organization (WHO) announced that parents and child caregivers should help children find positive methods for expressing their feelings of fear and sadness during the COVID-19 outbreak, and they should keep their children close to themselves (23).
As our results showed, the children whose mothers worked in a hospital or university-related centers reported more stress-related cognitive-emotional symptoms, including no clear thoughts. Therefore, it is recommended that parents involve their children in creative activities such as playing and drawing during the quarantine period and encourage them to state their thoughts in a safe and supportive environment.
Moreover, due to quarantine, it is suggested that parents use mental health improvement strategies, including spending time with children, answering questions, and sharing facts about COVID-19 in a way that they can understand, guiding children into regular activity schedule, and even consulting with a pediatric psychologist at the time of severe symptoms of stress.
5.1. Strengths and Limitations
This study had some limitations. We used the online sampling strategy because of the limited face-to-face contact and time sensitivity of the COVID-19 outbreak. Therefore, the study population may not reflect the actual pattern of the general population. Furthermore, self-reported symptoms of stress may not always be aligned with assessments evaluated by mental health experts. Likewise, respondents might have provided socially desirable responses in terms of satisfaction with the health information received.
Regardless of the limitations mentioned above, this study provides invaluable information on symptoms of stress among children in the first four months after the outbreak of COVID-19. To the best of our knowledge, few studies have used an online questionnaire to examine both physical and psychological symptoms of stress in children and adolescents. Given the home quarantine situation, it was impossible to access people. Also, paper questionnaires could increase the risk of virus transmission and more samples attrition. Therefore, online questionnaires could help to achieve better results. Our study was conducted with an almost acceptable response rate.
5.2. Conclusions
During the first four months of the COVID-19 outbreak, most of the respondents reported the degree of stress as low-to-moderate, and almost 25% of participants reported moderate-to-severe stress. The most common symptoms of stress in children were worrying, anger, and weakness. Also, older children, those being the first child, and children living with both parents were more exposed to stress. Therefore, these items should be included in the training provided to the health care team. Besides, psychological experts should formulate evidence-based guidelines and cost-effective psychological plans to cope with COVID-19 outbreak-related symptoms of stress in children and adolescents. This study confirmed the presence of stress symptoms in children aged 4-18 years during the COVID-19 outbreak. Therefore, it is recommended to conduct further longitudinal studies on the impact of long-term consequences of stress caused by the COVID-19 pandemic. Future studies can help to design the management and reduction interventions of stress to promote the health of this age group.