1. Background
Although extremely low birth weight (ELBW) has claimed fewer infant lives in the last few decades, still accounts for a considerable share of newborn deaths (1-3). Furthermore, the increased survival in premature infants has not been accompanied by a reduction in bronchopulmonary dysplasia (BPD), which is also an important cause of morbidity and mortality. Therefore, these infants remain a significant patient group for healthcare professionals caring for newborns (4).
Several scoring systems have been developed not only to predict potential problems and guide management strategies in ELBW infants but also to provide counseling for parents concerned about the health of their babies in the future (5-8). However, such scoring tools have been developed before the widespread use of surfactant and antenatal steroid therapy and, therefore, suffer from significant shortcomings (9). For instance, these tools cannot reflect clinical changes during the care process, nor the severity of the lung disease. Oxygenation index (OI), on the other hand, is measured invasively, generally requiring the use of arterial catheterization.
Furthermore, due to time intervals between blood samplings, continuous assessment is not possible. Iatrogenic anemia, infection, thrombosis, and necrotizing enterocolitis (NEC) are among potential complications due to the need for arterial catheterization and frequent blood sampling performed to estimate the OI (10, 11).
Respiratory severity score (RSS) is a non-invasive respiratory failure assessment tool that can be used on a continuous basis without blood sampling and is the product of mean airway pressure (MAP) and the fraction of inspired oxygen (FiO2). RSS has been shown to closely correlate with OI in newborns receiving mechanical ventilation (12) and has been utilized as a measure of disease severity in several large-scale, multi-center studies (13, 14). Further areas of previous research include the role of RSS in preparation for extubation as well as in the prediction of BPD, mortality, and short-term complications (15-17). Also, it has been found that RSS/kg is correlated more closely with pulmonary hypertension than RSS alone (18).
In the current era of less invasive strategies in newborn intensive care units, we believe that RSS may have an important value in the prediction of mortality or severe BPD, as suggested by the increasing number of studies providing promising data regarding the utility of this parameter. However, most of the available data on the role of RSS in the prediction of morbidity and mortality have been derived through single-center studies or those involving follow-up in a single center.
2. Objectives
To firmly establish the predictive value of a scoring system, its usefulness in patients admitted to different institutions and managed through varying respiratory therapeutic approaches should be demonstrated. In this study that involved patients admitted to two different academic hospitals, our aim was to evaluate the role of RSS in the first three days of life in predicting mortality or severe BPD in ELBW infants undergoing mechanical ventilation (MV).
3. Methods
3.1. Patients
Following a retrospective design, this study was performed on ELBW infants who received mechanical ventilation at the Newborn Intensive Care Units of Yeni Yuzyil University Medical Faculty Hospital and Biruni University Medical Faculty Hospital between July 2016 and December 2019. The study population consisted of infants weighing < 1000 g who were born in the study centers or born in other institutions but referred to one of the study centers. Infants intubated within the first day of life and requiring invasive mechanical ventilation for a minimum duration of three days were included. Exclusion criteria included late referrals, intubation after the first day of labor, successful extubation within the first three days, presence of major congenital anomaly, and death within the first three postnatal days. The study protocol was subjected to scrutiny by the local ethics committee of Yeni Yuzyil University.
3.2. Data Collection
Patient files and hospital electronic database were used to collect data on the following: demographics (gestational age, birth weight, route of labor, gender, antenatal steroid treatment, Apgar score at 5 minutes, intrauterine growth status, maternal age, preeclampsia, preterm premature rupture of membranes, chorioamnionitis), data on the clinical course (duration of invasive and non-invasive mechanical ventilation, duration of oxygen therapy, need for surfactant therapy, postnatal steroid treatment, late-onset sepsis, grade ≥ 3 intraventricular hemorrhage, patent ductus arteriosus requiring medical or surgical treatment, stage ≥ 2 necrotizing enterocolitis (NEC), stage ≥ 3 retinopathy of prematurity), duration of hospital stay, BPD, and mortality data.
RSS and RSS/kg for postnatal days 1, 2, and 3, as well as the average RSS and RSS/kg for the first three days, were estimated. For each study day, the highest RSS and RSS/kg were recorded in forms developed by the research team. The fraction of RSS durations in the first three days of life was taken into account in the calculation of time-weighted averages. RSS estimations were based on the MAP x FiO2 formula, while the birth weight was taken into consideration for RSS/kg calculation. If MAP was not available in the patient records, the following formula was used to calculate the MAP.
(PEEP, positive end-expiratory pressure; PIP, peak inspiratory pressure; Ti, inspiratory time; Te, expiratory time).
For patients receiving respiratory support in the high-frequency oscillatory ventilation (HFOV) mode, MAP values in the ventilatory settings of the device were used. The patients were categorized into two groups of those who survived without severe BPD and those who had severe BPD or died. Intra-group comparisons were performed concerning the RSS and RSS/kg.
3.3. Respiratory Management
Since this was a multi-center study and some patients were referred from other institutions, adopting a standard respiratory management strategy was not possible at the delivery room. However, despite the differences in treatment decisions between physicians, both centers strictly followed the international guidelines regarding the target oxygen saturation, permissive hypercapnia, mechanical ventilation, and weaning strategies, as well as the criteria for postnatal steroid use (19). HFOV was used only as a rescue treatment in both centers.
3.4. Definitions
Late referrals were defined as those who were transferred to the study centers after the first 6 postnatal hours, considering the time required for patient stabilization and city traffic conditions. Successful extubation was defined as the absence of the need for re-intubation for at least 24 since RSS could not be calculated. National Institutes of Health Consensus Classification was used for the diagnosis of severe BPD (20), the modified Bell’s criteria for stage ≥ 2 NEC (21), Papile classification for grade ≥ 3 intraventricular hemorrhage (IVH) (22), and the International Classification for the Retinopathy of Prematurity (23) for stage ≥ 3 retinopathy of prematurity (ROP). The presence of positive blood cultures after the first three days of life was defined as late-onset sepsis (24). Our criterion for PDA was the detection of hemodynamically significant PDA, whose criteria were specified in the PDA diagnosis and treatment guideline of the Turkish Neonatology Society (25).
3.5. Statistical Analyses
Data analysis was administered using IBM SPSS v.23 software. Quantitative data with normal distribution were compared using the independent sample t-test, while the Mann Whitney U test was used for non-parametric data. Categorical data were compared using the chi-square test. A binary logistic regression analysis was performed to determine risk factors for death or severe BPD. The performance of RSS in predicting death or severe BPD as well as the cut-offs for each parameter were determined with receiver operating characteristics (ROC) analysis. Statistical significance was considered when P-value < 0.05.
4. Results
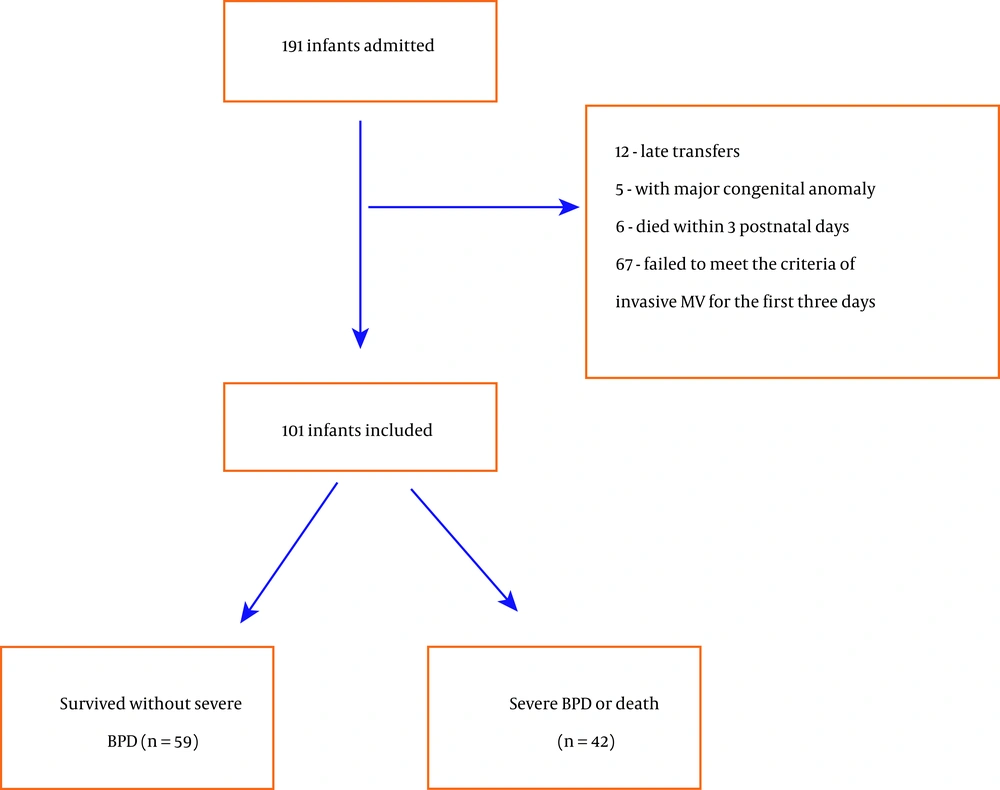
A total of 191 infants with a birth weight of < 1000 g were admitted to both centers during the study period, whom 67 were excluded due to failure to meet the criteria for invasive MV for the first three days, while 12, 5, and 6 were excluded due to late referral, presence of major congenital anomaly, and mortality within the first 3 days. Of the remaining 101 infants, 59 were survived without BPD, while 42 had severe BPD or died (21 deaths). The flow diagram of the study is shown in Figure 1, while Table 1 shows the demographic characteristics of the study groups. Birth weight, antenatal steroid treatment, and Apgar score at 5 minutes were significantly lower in infants who had severe BPD or died. Clinical characteristics and neonatal morbidities in the study groups are shown in Table 2. Infants with severe BPD or who died had a significantly higher duration of invasive MV, oxygen therapy, and hospital stay as compared to infants who survived without severe BPD. Also, infants with severe BPD or death had increased frequency of surfactant use and were more likely to suffer grade ≥ 3 IVH.
| Survival Without Severe BPD (n = 59) | Severe BPD or Death (n = 42) | P b | |
|---|---|---|---|
| Gestational age c (weeks) | 26 (25 - 27) | 25 (24 - 27) | 0.176 |
| Birth weight (g) | 785.5 ± 129.1 | 715.5 ± 145.4 | 0.012 |
| Male | 27 (45.8) | 24 (57.1) | 0.260 |
| SGA | 5 (8.5) | 8 (19) | 0.118 |
| 5-Min Apgar score c | 6 (5 - 7) | 6 (5 - 6) | 0.004 |
| Cesarean delivery | 43 (72.9) | 26 (61.9) | 0.243 |
| Antenatal steroid | 28 (47.5) | 9 (21.4) | 0.007 |
| Maternal age (y) c | 28 (23 - 31) | 29 (24.8 - 37) | 0.064 |
| Preeclampsia | 11 (18.6) | 4 (9.5) | 0.204 |
| Chorioamnionitis | 5 (8.5) | 2 (4.8) | 0.469 |
| pPROM > 18 h | 17 (28.8) | 6 (14.3) | 0.086 |
Abbreviations: BPD, bronchopulmonary dysplasia; SGA, small for gestational age; pPROM, preterm premature rupture of membranes.
aValues are expressed as No. (%) and mean ± SD unless otherwise indicated.
bU: Mann Whitney U test, t: Student t-test for independent samples, χ2: Chi-square test.
c Values are presented as median (interquartile range)
| Survival Without Severe BPD (n = 59) | Severe BPD or Death (n = 42) | Pb | |
|---|---|---|---|
| Surfactant ≥ 2 doses | 26 (44.1) | 33 (78.6) | < 0.001 |
| Duration of invasive MV c (days) | 10 (5 - 15) | 29 (15.5 - 53) | < 0.001 |
| Duration of non-invasive MV c (days) | 15 (9 - 25) | 20 (13 - 30.5) | 0.120 |
| Duration of supplemental oxygen c (days) | 22 (16 - 37) | 38.5 (25.5 - 47.8) | 0.003 |
| Postnatal steroid | 49 (83.1) | 24 (96) | 0.108 |
| Pneumothorax | 2 (3.4) | 3 (7.1) | 0.391 |
| Late onset sepsis | 17 (28.8) | 7 (16.7) | 0.239 |
| Grade ≥ 3 IVH | 10 (16.9) | 16 (38.1) | < 0.001 |
| PDA requiring treatment | 28 (47.5) | 29 (69) | 0.051 |
| Stage ≥ 2 NEC | 13 (22) | 13 (31.7) | 0.394 |
| Stage ≥ 3 ROP | 16 (27.1) | 13 (43.3) | 0.192 |
| Length of stay (days) c | 87 (76 - 105) | 130 (108 - 171) | < 0.001 |
Abbreviations: BPD, bronchopulmonary dysplasia; IVH, intraventricular hemorrhage; PDA, patent ductus arteriosus; NEC, necrotizing enterocolitis; ROP, retinopathy of prematurity; MV, mechanical ventilation.
aValues are expressed as No. (%) and mean ± SD unless otherwise indicated.
bU: Mann Whitney U test, χ2: Chi-square test.
c Values are presented as median (interquartile range).
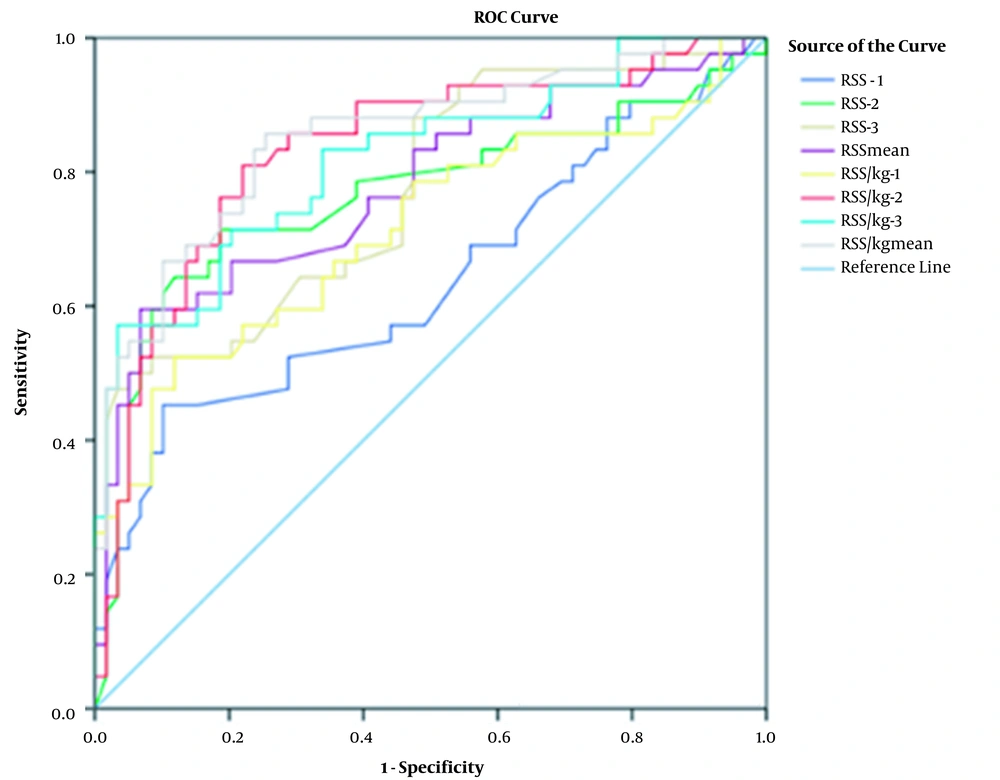
All RSS and RSS/kg parameters in each of the first three days of life as well as the time-weighted average values for the same period were significantly higher in infants with severe BPD or death, as compared to infants surviving without severe BPD (Table 3). Table 4 shows the sensitivity and specificity of RSS values in predicting severe BPD or death, while Figure 2 presents the ROC curves. Of all RSS values, the highest AUC (area under the curve) value was identified for RSS/kg mean with a cut-off of 3.62 (AUC = 85.3%). We categorized the RSS/kg mean values above this cut-off value as high and the values below it as low. While RSS/kg mean value was higher than 3.62 in 6.8% of the infants in the survival without severe BPD group, this rate was 52.4% in the severe BPD or death group. This difference was statistically significant between the study groups (P = 0.001). We performed multivariate logistic regression analysis including birth weight, 5th min Apgar score, antenatal steroid use, duration of invasive mechanical ventilation, multiple surfactant use, grade ≥ 3 intraventricular hemorrhage, PDA, and RSS/kg mean score. In this analysis, RSS/kg mean score and duration of invasive mechanical ventilation remained statistically significant. It was determined that a RSS/kg mean score of > 3.62 is accompanied by an increased risk of death or severe BPD by 2.28 times. (P = 0.001) (Table 5).
| Survival Without Severe BPD | Severe BPD or Death | Pb | |
|---|---|---|---|
| RSS - 1 | 2.7 (2.2 - 3) | 2.9 (2.5 - 3.8) | 0.018 |
| RSS - 2 | 2.4 (2 - 2.8) | 4 (2.6 - 7.1) | < 0.001 |
| RSS - 3 | 2.1 (1.8 - 2.7) | 3.2 (2.3 - 5.7) | < 0.001 |
| RSS mean | 2.4 (2.1 - 2.8) | 3.7 (2.6 - 5.9) | < 0.001 |
| RSS/kg - 1 | 3.5 ± 0.8 | 4.71 ± 1.85 | < 0.001 |
| RSS/kg - 2 | 3 (2.6 - 3.7) | 5.8 (4 - 9.3) | < 0.001 |
| RSS/kg - 3 | 2.9 (2.3 - 3.4) | 5.2 (3.3 - 8.2) | < 0.001 |
| RSS/kg mean | 3.2 (2.7 - 3.7) | 5.4 (4 - 8.1) | < 0.001 |
Abbreviation: RSS, respiratory severity score.
aValues are presented as median (interquartile range) or mean ± SD.
bU: Mann Whitney U test, t: Student t-test for independent samples.
| Measurement | Cut-off | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC |
|---|---|---|---|---|---|---|
| RSS - 1 | ≥ 3.260 | 45.2 | 89.8 | 76.0 | 69.7 | 63.8 |
| RSS - 2 | ≥ 2.850 | 71.4 | 81.4 | 73.2 | 80.0 | 76.5 |
| RSS - 3 | ≥ 3.350 | 50.0 | 94.9 | 87.5 | 72.7 | 77.2 |
| RSS mean | ≥ 3.300 | 59.5 | 93.2 | 86.2 | 76.4 | 77.8 |
| RSS/kg - 1 | ≥ 4.400 | 52.4 | 88.1 | 75.9 | 72.2 | 71.5 |
| RSS/kg - 2 | ≥ 3.760 | 81.0 | 78.0 | 72.3 | 85.2 | 83.3 |
| RSS/kg - 3 | ≥ 4.850 | 57.1 | 96.6 | 92.3 | 76.0 | 82.0 |
| RSS/kg mean | ≥ 3.620 | 85.7 | 74.6 | 70.6 | 88.0 | 85.3 |
Abbreviations: BPD, bronchopulmonary dysplasia; RSS, respiratory severity score; PPV, positive predictive value; NPV, negative predictive value; AUC, area under the receiver operating characteristic curve.
| B | S.E | Wald | OR (%95 CI) | P | |
|---|---|---|---|---|---|
| Birth weight | -0.002 | 0.003 | 0.370 | 0.999 (0.993 - 1.004) | 0.543 |
| Antenatal steroid | 1.151 | 0.713 | 2.602 | 3.16 (0.781 - 12.791) | 0.107 |
| 5-Min Apgar score | -0.101 | 0.323 | 0.099 | 0.904 (0.48 - 1.702) | 0.754 |
| RSS/kg mean | 0.824 | 0.259 | 10.139 | 2.279 (1.373 – 3.784) | 0.001 |
| Duration of invasive MV | 0.08 | 0.027 | 8.885 | 1.083 (1.028 – 1.142) | 0.003 |
| Surfactant ≥ 2 doses | 0.642 | 0.801 | 0.643 | 1.901 (0.395 – 9.136) | 0.423 |
| Grade ≥ 3 IVH | 0.23 | 0.773 | 0.088 | 1.258 (0.276 – 5.73) | 0.766 |
| PDA requiring treatment | -0.044 | 0.732 | 0.004 | 0.957 (0.228 – 4.017) | 0.953 |
| Constant | -4.945 | 2.861 | 2.988 | 0.007 | 0.084 |
Abbreviations: BPD, bronchopulmonary dysplasia; RSS, respiratory severity score; MV, mechanical ventilation; IVH, intraventricular hemorrhage; PDA, patent ductus arteriosus.
aCox & Snell R2 = 0.487; Nagelkerke R2 = 0.656; Hosmer-Lemeshow χ2 = 3.323 (P = 0.913).
5. Discussion
This study demonstrated that all RSS values are higher in the first three days of life in infants in the severe BPD or death group. Among these values, RSS/kg mean has the highest AUC compared to other scores. In the multivariate logistic regression analysis performed in terms of its association with severe BPD or death, it was determined that the duration of invasive mechanical ventilation, as well as the RSS/kg mean score, remained statistically significant.
In a previous study, Malkar et al. (26) reported that a RSS of ≥ 6 at 30 days of life was associated with higher mortality and longer duration of MV in newborns requiring prolonged MV. In a more recent study, no significant differences in RSS scores at 2 and 7 days of life were observed, while those measured at days 14, 21, and 28 were associated with a higher risk of severe BPD or mortality (16). Results from both of these studies imply a predictive value for RSS at later days following labor. Although non-invasive MV techniques are increasingly more frequently preferred in the care of extremely low birth weight infants, approximately half of these babies continue to require endotracheal intubation and invasive MV (27, 28). Barotrauma and volutrauma associated with mechanical ventilation, as well as the cellular injury caused by free oxygen radicals formed by oxygen toxicity play significant roles in the development of BPD (29, 30). Obviously, lung injury inflicted in the first days of life is likely to affect the clinical course of the infant. In one study utilizing parameters other than the respiratory severity score, ELBW infants still requiring mechanical ventilation at postnatal day 7 were found to have an increased risk of BPD (31). Bhattacharjee et al. (32), in their study involving 69 ELBW infants, showed that the mean RSS scores in the first three days of life had good predictive value for the combined outcome of IVH, BPD, ROP, and mortality. Similarly, we also based our study on the assumption that early lung injury would affect the consequent risk of morbidity and mortality; thus, explored the association of severe BPD and death with the RSS scores in the first three days of life, showing that all RSS parameters were higher in infants who had severe BPD or died. A ROC analysis incorporating all RSS parameters also suggested that the mean RSS had a better predictive value than daily RSS scores. Based on these observations, we may assume that as compared to sporadic RSS measurements, a mean RSS score may be a better indicator of the severity of lung disease in the first three days of life and may have a higher predictive power in reflecting the risk of severe BPD or death.
The respiratory severity score is simply the product of MAP and FiO2 and has been effectively utilized in previous studies to estimate the severity of lung disease (13, 14). Despite recommendations regarding the target oxygen saturation in ELBW infants, no definitive MAP value guaranteeing optimum ventilation in each infant exists, and this value is dependent upon the severity of the lung disease. Additionally, the same MAP value should lead to various effect sizes in different lungs. For example, Seo et al. (18) pointed out the fact that a MAP of 10 cmH2O would lead to differential effects in the lungs of an infant with a birth weight of 500 g and in the lungs of an infant with a birth weight of 1000 g and calculated RSS as well as RSS/kg in the first 5 days of life in their study that intended to investigate the relationship between the development of pulmonary hypertension and RSS. They also found elevated RSS only on days 2 and 4, while RSS/kg was increased throughout the whole 5-day period. In that study, RSS/kg at day 2 of life had the largest AUC and maintained its statistical significance in the multivariate logistic regression analysis. Similarly, we also assumed differential effect sizes on lungs for a given MAP value, and calculated RSS/kg in addition to RSS when exploring the correlation between RSS and severe BPD or death. ROC analyses suggested that RSS/kg had a higher predictive value than RSS, not only within each study day but also when compared with using the mean values, i.e., RSS/kg mean vs. RSS mean for the whole study duration. Among all RSS parameters, the RSS/kg mean had the largest AUC with a cut-off of 3.62. In our study, we performed multivariable logistic regression analysis because there were significant differences between the study groups concerning some important risk factors that may have an impact on mortality or the development of severe BPD. Birth weight, 5th min Apgar score, antenatal steroid use, duration of invasive mechanical ventilation, multiple surfactant use, grade ≥ 3 intraventricular hemorrhage, and PDA were included in this analysis. RSS/kg mean score along with the duration of invasive mechanical ventilation remained statistically significant.
Most studies exploring the predictive role of RSS involved patients who required invasive MV. In Shah et al.’s study (17), NCPAP pressure was considered equal to MAP in infants requiring nasal continuous positive airway pressure (NCPAP) in the birth room with no need for subsequent MV. These authors found that a RSS of ≥ 2 on the first postnatal day was associated with increased morbidity and mortality in infants weighing ≤ 1250 g. On the other hand, in infants undergoing NCPAP or nasal positive pressure ventilation (NIPPV) therapy, the ventilator settings for PEEP/MAP are not equal to the achieved MAP (33, 34). In our view, the target MAP and MAP achieved in the lungs are dissimilar in infants undergoing noninvasive MV, due to a number of factors including the choice of interface, air leakage, spontaneous respiration by the patient, and synchronization problems. Thus, if RSS is to be used in infants requiring noninvasive MV, the noninvasive respiratory management strategy should be well standardized. Since this was a multi-center study with variations between study centers in terms of device and interface choices, we excluded patients undergoing noninvasive MV in the first three days of life in order to preserve the reliability of MAP and RSS values.
Ideally, a scoring system should be practical, be applicable in the early course of hospital admission, be able to provide certain morbidity, mortality, and cost-effectiveness estimations in a reproducible and reliable manner, and should also be feasible for all newborn patient groups (35). Previous studies on RSS have established the ease of use, predictive value for morbidity and mortality, as well as utility in the early phases of life, for this scoring tool. However, most of these studies followed a single-center approach, involving patients managed within that center following labor (15, 16, 18, 26, 32). In this regard, our study differs from these previous investigations, as it was a multi-center study and included referrals from other centers within the first 6 hours of life. The inclusion of patients undergoing different respiratory management strategies from birth indicates that our findings are based on a heterogeneous group of ELBW infants, improving the generalizability of our observations.
It is necessary to mention some limitations of our study. Firstly, it was a retrospective study with data collection from patient records. Also, although it was a multi-center study, the sample size was relatively small. The main reasons for this include the increased use of noninvasive ventilation and minimally invasive surfactant treatments in recent years, as well as the lack of reliability of RSS scores in infants undergoing noninvasive ventilation. Considering the recent trends in the respiratory management of this patient group, data collection was restricted to the study period only. In our study, IVH differed between the study groups and was somewhat higher than previously reported (36). The most likely explanation for this finding was the exclusion of ELBW infants who were never intubated or extubated in the first three days of life, leading to the inclusion of higher-risk patients. On the other hand, the reason for the exclusion of infants referred to study centers after the first 6 postnatal hours related to the fact that late referrals usually involve severe morbidities (respiratory distress requiring the use of HFOV, IVH, sepsis, etc.) experienced during intensive care that would directly interfere with study findings.
5.1. Conclusions
In conclusion, our study demonstrated that RSS/kg mean in the first 3 days of life has predictive value in indicating severe BPD or death. Furthermore, mean RSS had more predictive power than single RSS determinations, and incorporating body weight was associated with improved sensitivity of the score. Prospective multi-center studies with larger patient populations may provide further insights into the utility and predictive value of RSS in these patients.