1. Case Presentation
A 4.5-year-old boy was referred with a history of fever, limping, and pain in the left hip for six days. He had been admitted upon the beginning of symptoms and was discharged by personal consent without a certain diagnosis. There were no histories of recent drug use or previous illnesses, including recent upper respiratory tract infection, gastroenteritis, or urinary tract infection. No previous episodes of limping, arthralgia, or myalgia was reported. The patient did not complain of abdominal pain. No trauma history was given. The parents did not report any unusual episode of bleeding formerly. The patient was immunized according to national protocols.
Evaluation of a limping child must include careful history taking. The duration of the problem guides us towards different diagnoses. Acute onset limps, as is the case here, are usually because of infection or trauma. A history of trauma should be specifically asked, and child abuse should always be taken into consideration. Fever is a very important symptom, suggesting osteomyelitis, septic arthritis, or myositis. Causes of chronic limping are also plausible in case of an acute episode. Systemic lupus sclerosis, leukemia, and juvenile idiopathic arthritis are rare causes of fever and chronic limping.
The patient’s age gives us valuable clues in the differential diagnosis. Slipped capital femoral epiphysis, for instance, is usually seen in children older than 10 years old.
Henoch-Schoenlein purpura can be presented with arthralgia or arthritis accompanied by rash and abdominal pain. Sickle cell disease, via venoocclusive attacks and hemophilia, by causing hemarthrosis, might cause joint pain. A careful previous illness history can be very beneficial; transient synovitis might occur after a viral upper inspiratory infection, and reactive arthritis can follow urinary tract infection or gastroenteritis. Recent use of antibiotics can be in favor of serum sickness or serum sickness like disease.
The patient appeared well but in slight pain when seated. He kept his left leg immobile and slightly flexed, and externally rotated in hip joint. His vital signs were within normal limits. He could not bear to stand on his feet and was completely reluctant to be examined. When the patient was distracted, severe tenderness was found when the left hip was touched by the parent, and he expressed severe pain on hip movement in all directions, thus presented a restriction in left hip range of motion. Erythema and hotness were not found. A thorough examination of other joints did not yield any abnormal results. No skin abnormality could be observed, including rash or bruising. Also, abdominal examination was normal.
When a child is presented with an inability to walk properly, the site of the lesion must be differentiated. Young children might not be able to specify pain location. A meticulous physical examination, mostly helpful when a child is distracted, or analgesics are provided, can be very informative. Therefore, nonopioid analgesics can help get better results in this examination. When the child is uncooperative, parents can be asked for help, cautiously touching the normal limb first and then the painful one, trying to find the affected area. This child seemed to be pain-free in the spine and right lower limb, and the pain and tenderness seemed localized to the left hip, with remarkable loss in the left hip range of motion. Since the child was very irritable when touching or moving the left hip, it could not be surely stated whether bone tenderness was present.
If the cause of limp cannot be specified, a complete examination must follow, including all the parts of the lower limbs, spine, and central nervous system. Abdominal pains can present as hip pain, and pelvic inflammatory disease and psoas abscess can be reasons for pain and limping. External genitalia must be observed, having testicular torsion in mind.
Laboratory evaluation revealed a white cell count of 10170 per cubic millimeter with a neutrophil count of 5930, ESR of 64 mm/hour, and CRP of 57 mg/L. Other laboratory values were as follows: Hemoglobin 11.2 g/dL, platelets 233000 per cubic millimeter, LDH 441 U/L, CPK 21 IU/L, Aldolase 15 U/L, AST 43 U/L, and ALT 65 U/L. Wright, COOMBS Wright, and 2ME results were negative. Also, blood culture was negative.
With a primary impression of septic arthritis, parenteral clindamycin and oral Naproxen therapy were initiated. Since ESR increased to 74 in one-day interval, WBC count reached 15170 with a neutrophil count of 10000, and the patient’s pain did not decrease, the antibiotic was changed to vancomycin.
Infections induce leukocytosis and high ESR and CR. High values of LDH, CPK, aldolase, and AST can show muscle involvement, especially in infectious myositis. Pyomyositis, however, might not be presented with elevated muscle enzymes. This patient showed mild elevations in LDH, AST, and aldolase, and had normal CPK.
When a patient complains of acute limp and signs of acute bacterial infection, such as fever, joint tenderness with decreased range of motion, focal bone tenderness, or localized redness, warmth, or swelling, CBC, ESR, CRP, and blood culture must be studied. Septic arthritis should always be considered and ruled out in such patients since delay in therapy can cause non-reprimandable outcomes.
As the most common pathogen responsible for septic arthritis is Staphylococcus aureus in all ages, it should be covered in empiric therapy, and that is why clindamycin was administered before imaging interpretations were ready. This choice could also be appropriate for the other possible differential diagnoses, such as osteomyelitis and pyomyositis.
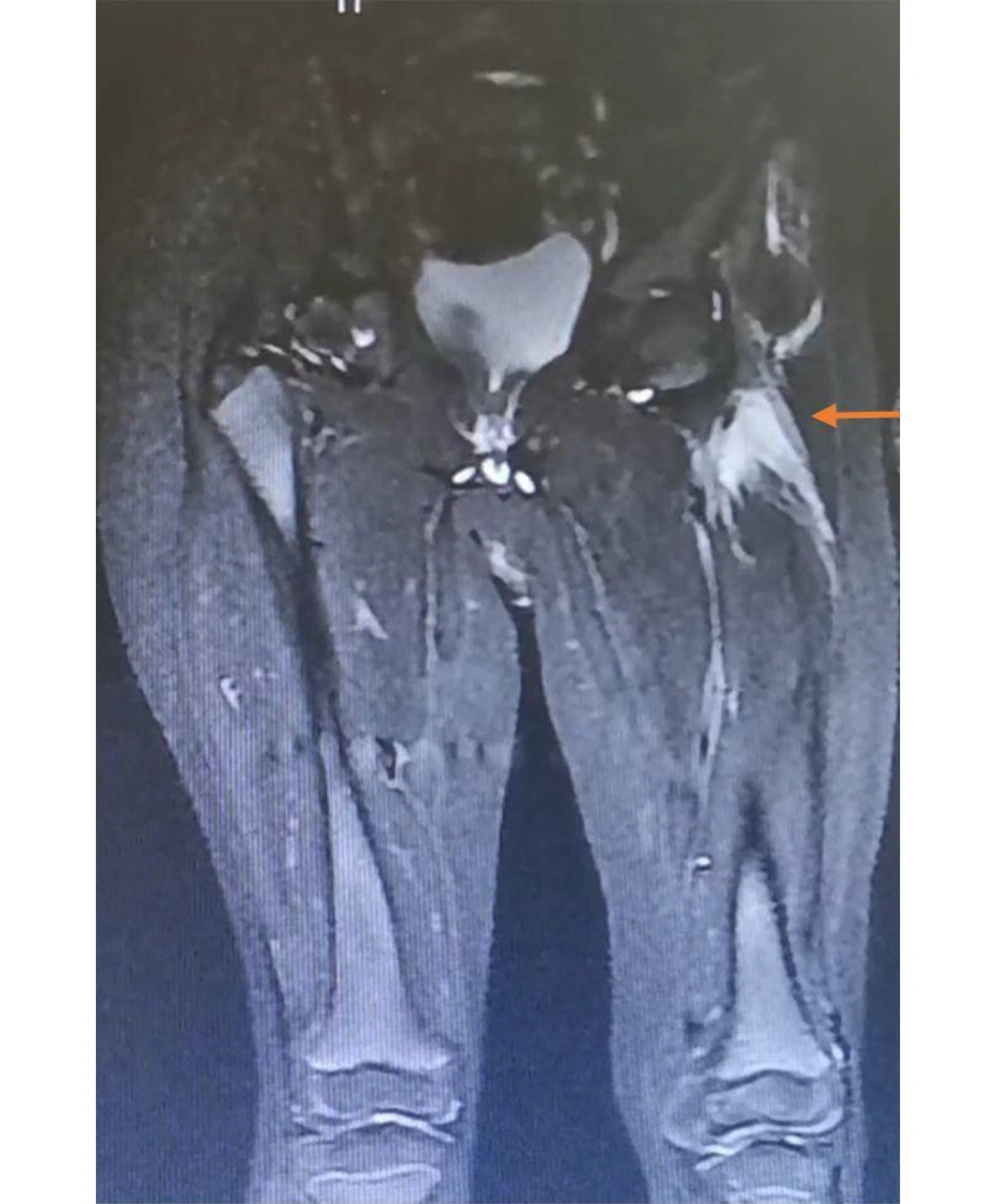
The patient’s previous sonography did not report any effusion in the hip or knee, neither did it find a psoas abscess. Repeated sonography showed the same results. Hip magnetic resonance imaging (MRI) found no joint effusion but elucidated signs of inflammation in muscles of the periarticular and proximal femoral area (iliopsoas and gluteus maximus), and no collection could be noticed (Figure 1). By the time MRI was reported, the patient’s pain had worsened, ESR had raised to 90, CRP had decreased to 46, and CPK and LDH were increased to 31 and 466, respectively.
When septic arthritis is in doubt, diagnostic evaluations and subsequently appropriate treatment must be initiated promptly. Since the patient was referred with unilateral hip pain, fever, leukocytosis, and high inflammatory markers, we were highly suspicious of septic arthritis. That is why MRI was performed to search for possible effusion that could be missed by sonography, and to search for abscess or myositis. Septic arthritis was ruled out with MRI, and the findings were compatible with myositis and combined with laboratory findings, pyomyositis seemed to be a favorable diagnosis. As the administered antibiotic was effective against the most common cause of pyomyositis, S. aureus, it was continued.
The patient received 11 days of parenteral antibiotic therapy and was discharged by personal consent. Oral clindamycin and naproxen were prescribed to be used at home. On discharge day, he was fever-free, and a slight pain decrease was reported, yet he was still unable to walk. The parents were strongly recommended to bring their son for follow-up visit at the clinic within a week and to come to the emergency department in case of worsening of the symptoms or systemic manifestations.
In the first follow-up visit, the parents declared that their son had been complaining of pain less often. A slight restriction in left hip range of motion (ROM) was found upon examination. Since the illness seemed to be in the recovery phase, no imaging was obtained. After one month, the parents had no complaints, and they expressed that the child was “running and jumping more than ever”.
2. Discussion
This patient presented with an acute episode of limping and fever. Combining the history, physical examination, and primary laboratory values, septic arthritis of the left hip appeared a possible diagnosis and needed to be ruled out due to importance and prevalence. Since sonography could not find effusion or any abnormality in the area, MRI was performed and carefully analyzed by expert radiologists and orthopedists. Inflammation in periarticular and proximal femoral muscles was noted, and no joint effusion could be found. Since inflammatory markers, i.e., neutrophil count, ESR, and CRP were markedly increased, and biochemical markers of muscular damage were only slightly elevated, pyomyositis seemed to be the most suitable diagnosis.
Pyomyositis or purulent infectious myositis is a pyogenic muscular infection. The course of pyomyositis can be divided into three stages (1). The first stage, with a duration of 10 to 21 days, is the diffuse inflammation phase, characterized by local muscle pain and cramp with or without fever. As the inflammation progresses, systemic symptoms predominate in the second stage. The third stage presents with severe systemic manifestations and complications due to bacteremia.
Although formerly known as tropical, the frequency of pyomyositis has increased in temperate climates (2). Some predisposing factors can be found in affected patients, such as immunodeficiencies, injection drug use, diabetes, concurrent infection, or a blunt trauma (3).
The most common cause of pyomyositis is S. aureus, and methicillin-resistant S. aureus (MRSA) has been an increasingly prevalent pathogen. Other less common causes include non-group A beta-hemolytic streptococci, pneumococci, gram-negative bacilli, mycobacteria, and rarely, especially in immunodeficient patients, polymicrobial (4). It is notable that pneumococcal vaccination is not a part of the national vaccination program in Iran, and this should be considered when evaluating children with probable pyomyositis.
As a bacterial infectious disease, leukocytosis with neutrophil predominance and high inflammatory markers such as ESR and CRP is noticed in pyomyositis. It is of interest that serum markers of muscle injury are not generally elevated (5). This is a remarkable distinction between pyomyositis and viral myositis, as the two diagnoses are occasionally hard to be distinguished clinically from one another.
MRI is the choice imaging modality for muscular infections, as it is fairly sensitive and specific, has admirable soft tissue contrast, and can show bone edema early in the course of the disease (6). However, its high price, unavailability in regions with limited resources, and the need for anesthesia in children make it less favorable, especially as the first option for imaging. Sonography, on the other hand, is widely available, has a low cost, and unlike CT scan, does not expose the child to radiation. It should always be noted that sonography is operator-dependent and needs high skill for performance and interpretation (7).
Sonography may detect muscle volume increase, disarrayed and hyperechoic muscle fibers, and hyperemia in the early stages of pyomyositis. However, it might be unable to distinguish these changes as they occur subtly at the beginning of the course. As the condition deteriorates, a more precise and complex fluid collection or abscess can be observed (3, 8). In our patient, sonography was unable to detect any alteration in muscles, although it was performed by highly skilled radiologists, which might be due to the non-advanced stage of the disease.
If the patient is referred in stage 1, antibiotics are the mainstay of treatment, and they should be promptly administered in all cases of pyomyositis. Yet, most patients are presented in stage 2 or 3, and the treatment should include both drainage and intensive antibiotic regimen. As the most common etiology for pyomyositis is S. aureus, antibiotics should cover this pathogen in the first place, including MRSA and also beta-hemolytic streptococci. Clindamycin is a good option for these cases. If the patient is immunodeficient, however, broader coverage is mandatory (9). Our patient was treated with clindamycin initially, and since the symptoms did not improve and the inflammatory markers worsened, it was changed to vancomycin. Nevertheless, worsening of the condition could be due to the progression of the disease course, and it is not always anticipated that symptoms and signs abate upon starting antimicrobials.
Clinical and radiographic improvement determine the duration of antibiotic therapy. The exact duration of parenteral and oral antibiotic therapy varies in different trials. Two studies administered 11-13 days of parenteral and 20-30 days of oral antibiotic therapy (10, 11), while two other series recommended four to seven days of intravenous therapy with a mean total duration of two to six weeks (12, 13). All these studies yielded acceptable outcomes. However, extensive infections need longer durations of therapy (14, 15). Our patient received parenteral therapy for 11 days followed by two weeks of oral therapy, fortunately with a plausible outcome.
Physical therapy has been discussed in the literature in different types of joint and muscle inflammation. Its role has been emphasized in idiopathic inflammatory myopathies such as dermatomyositis (16). In pyomyositis, however, it has not been well-described and needs to be further evaluated.