1. Introduction and Case Presentation
A 6-year-old boy was referred to our hospital with the complaint of stiffness in both knees, which had commenced 2 years ago and progressed gradually to both hips, ankles, elbows, fingers, and toes. He occasionally had arthralgia without complaint of joint swelling, fever, or weight loss. There were no signs of any other organ involvement.
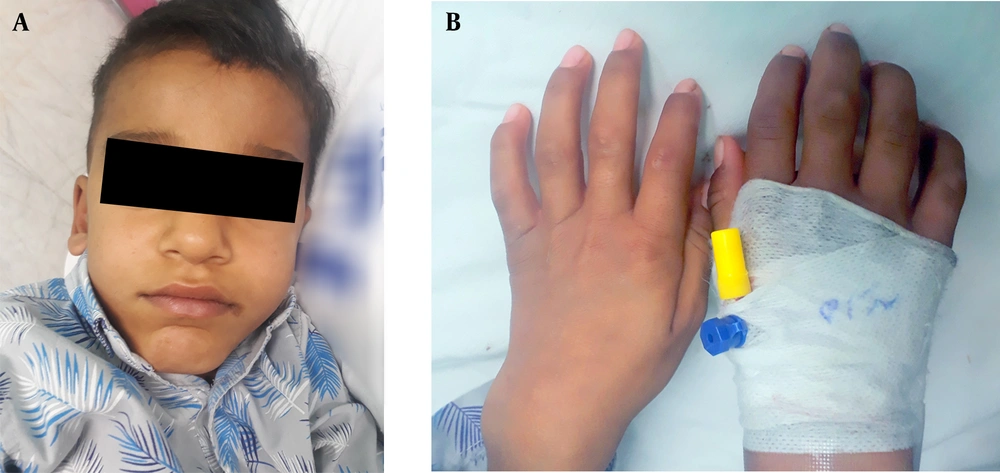
He had short stature, and his weight and height matched the 5th percentile. He gained normal developmental milestones but with poor school performance. He had a long face, prominent forehead, chin, and short neck (Figure 1A). His hearing and vision seemed intact with a clear cornea. A grade 2 systolic murmur was auscultated. The liver and spleen had normal sizes in palpation. Cervical spine movements were normal. There was a limitation in the range of motion of all shoulder movements, especially abduction. Elbows had deformity with flexion contracture. Decreased range of motion of knees in extension and flexion was evident. All hip joint movements were restricted. Claw hand deformity, flexion deformity of distal interphalangeal joints in the feet, and dorsiflexion limitation in the ankle were found (Figure 1B).
His past medical history was notable for several hospitalizations due to pulmonary infections. He was the first child of consanguineous marriage, and his younger sister was healthy. His father suffered from major thalassemia, and there was no history of rheumatologic or metabolic diseases in the family.
Laboratory data, including CBC, CRP, and ESR, were normal except for microcytic RBCs. FANA, RF, Anti CCP antibodies were negative. Hemoglobin electrophoresis demonstrated Thalassemia minor (HbA: 94.4 and HbA2: 5.6). Calcium, phosphorus, ALK, and PTH levels were within normal limits. A 3+ glycosaminoglycan (GAG) excretion was detected in the urine test.
Echocardiography identified mild mitral and tricuspid valve regurgitation.
2. Discussion
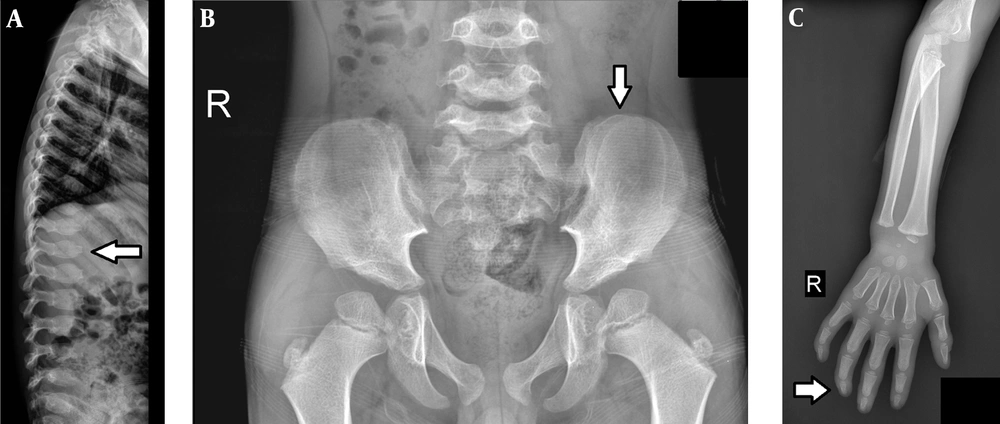
Skeletal survey images revealed a normal skull, central beaking, bullet shape appearance in the cervical and lumbar vertebra, tapering of the iliac wings (Figure 2B), deformity of the femoral head, and short sacral length. He also had proximal tapering of metacarpals (Figure 2C).
The whole body Triphasic bone scan was normal.
Whenever there is joint stiffness without evidence of inflammation, metabolic diseases should be considered. In this patient joint stiffness, dysostosis multiplex, valvular heart disease, and positive GAG in urine denoted MPS disease (1, 2). Since enzyme assays for MPS were unavailable and the child was the offspring of a consanguineous marriage, genetic testing was performed which revealed Mucolipidosis type III_Gamma. Mucopolysaccharidoses and Mucolipidoses are progressive storage disorders that share many clinical characteristics. Their diagnosis is confirmed by specific enzyme assays in the serum, leukocytes, or skin fibroblasts (3).
Joint stiffness or contracture demonstrates the loss of passive range of motion of diarthrodial joints. It has different causes, including congenital arthrogryposis, chronic inflammatory and non-inflammatory disorders, trauma, and prolonged immobility. A complete history (including the course and progression of contracture and distribution of affected joints) and thorough musculoskeletal examination are important to narrow the differential diagnosis of a stiff joint.
Characteristic appearance, consanguinity, positive family history, absence of inflammatory markers in the laboratory tests, and peculiar radiological findings are clues for the diagnosis of noninflammatory disorders (e.g., storage diseases) as the cause of joint contracture.
Dysostosis multiplex refers to skeletal changes which occur in storage disorders such as mucopolysaccharidoses, mucolipidoses, or gangliosidoses. These changes are due to the progressive storage of complex carbohydrates (glycoproteins or glycolipids) in the lysosomes. Classical presentations of dysostosis multiplex include abnormal J-shaped sella turcica, paddle-shaped ribs, several superiorly notched (inferiorly beaked) vertebral bodies, middle beaked vertebral bodies, tapered inferior iliac, proximally pointed metacarpals, and short broad metacarpals with thin cortices.
Treatment for mucolipidosis type 3 consists of orthopedic interventions and physiotherapy. Intravenous pamidronate has been used to reduce pain and improve mobility. Progress is usually slow, and patients generally live up to the fifth decade of life.