1. Background
Nephrotic syndrome is still the most common glomerular disease worldwide, with an incidence around 1 to 3 cases per 100,000 people (1-3). The disease is usually diagnosed following a viral infection of upper respiratory tract with sudden edema, proteinuria in the range of nephrotic syndrome (> 50 mg/kg/day), hypoalbuminemia (serum albumin < 2.5 g/dL), and hyperlipidemia (TG > dL/200mg) (3). The average age of children with NS is 4 years, being more prevalent in boys than girls (2, 4-6). However, the prevalence varies according to age, sex, race, and geographical location (6).
Frequent exposure of these patients to corticosteroids and the recurrent nature of disease itself can pose serious health-related challenges to quality of life (5, 7). Growth retardation, bone deformity, gingival hypertrophy, hirsutism following corticosteroid and cyclosporine use, and edema are the most common complications posing physical changes which can be distressing, especially in adolescence. These children seem to suffer from problems such as lack of self-confidence due to retardation of growth and development and have limitations in academic and social performance. Frequent absences from school due to long-term hospitalizations and restrictions on group activities can also add to their problems (8). One aspect of the management of these patients is the issue of their compliance with medical instructions, caused by the long course of the disease and the side effects of medications. This is especially problematic in adolescents who are going through the critical years of life physically and emotionally. Proper identification and management of issues which affect the quality of life of these patients can ultimately lead to better adherence to medical instructions and hence better management of the disease. In fact, by recognizing the impact of the disease on various aspects of the lives of patients with nephrotic syndrome, they may receive better care. A better understanding of the health-related quality of life of people with nephrotic syndrome helps understand how patients feel about themselves and their performance and to better guide their therapy (5, 9).
Health-related quality of life (HRQoL) is a multidimensional concept developed by the US Centers for Disease Control and Prevention (CDC) which includes the physical, emotional, and social aspects and goes beyond simply measuring population health, life expectancy, and causes of death (10). Children's Quality of Life Questionnaire, or Ped’sQoL, is a tried and tested tool based on classical test theory for assessing individuals' emotional, physical, social, and school functioning. Fortunately, the validity and reliability of the Persian translation of the "Quality of Life for Children" questionnaire was justified in the study of Amiri et al. (11).
2. Objectives
There have been many studies around the world on the impact of nephrotic syndrome on patients' health-related quality of life, but it is not possible to generalize the results of these studies due to racial, geographical, and genetic diversity (6). Our study is different regarding its` special design, consisting a cohort of patients with nephrotic syndrome and two control groups, including a group of people with other chronic diseases and a control group of healthy people. We also try to examine the impact of disease complications and demographic characteristics on people's quality of life. To manage the disease properly, it is necessary to acknowledge the condition of people with the disease and the problems they face. After knowing the quality of life of children with nephrotic syndrome, perhaps one of the first steps in managing the problems of these patients is to periodically assess their quality of life using the standard Ped’sQL questionnaire. This allows early identification of these problems and take timely action to manage them. Perhaps a better management of patients with nephrotic syndrome may be adressed in a multidisciplinary team (12).
3. Methods
This is a cross-sectional, case-control study conducted at Children’s Medical Center, a teaching hospital of Tehran University of Medical Sciences, Iran. With Alpha of 0.0500, power of 0.9500, Delta of 7.800, M1 of 79.500, M₂ of 87.300, Sd1 of 11.900, and Sd of 8.600, the estimated total volume of study cohort would come to 96 subjects. The case group included 60 children who met the following criteria: Children aged 6 - 18 years with nephrotic syndrome for more than one year; with normal kidney function (Glomerular filtration rate > 90 mL/min/1.72 m2 [Schwartz et al., 1987]); without any physical, psychological or obesity-related disorder; without any active infection, Edema and not hospitalized at the time of enrollment. Those with obesity, low GFR, or any other disability were excluded from the study.
There were two different control groups. First, healthy control group included 81 children visiting the outpatient clinic of Children’s Medical Center, without any chronic renal disease or other chronic illnesses. To better elucidate the specific effects of the nephrotic syndrome as a chronic disease and its complications on HRQoL, and not just as a chronic illness, the second control group of 98 unhealthy subjects with chronic illnesses involving other systems - juvenile rheumatoid arteritis 19 subjects, Cystic fibrosis 21 subjects, epilepsy 24 subjects, hematological disorders 16 and cardiovascular diseases 18 subjects- were assigned.
A PedsQL™ 4.0 generic core scale is a questionnaire that includes child self-report and parent-report that covers 4 domains: Physical function containing 8 questions, Emotional, Social and Educational functions each with 5 questions. To answer each question, a 5-option response is asked from 0 to 4 which means 'never a problem' to 'almost always a problem', respectively. A Farsi version (language of all participants) of the PedsQL™ 4.0 Generic Core Scale is available for free after registration at here provided by MAPI research institute, Lyon, France] and its reliability and validity in Iranian population was justified (11). After getting informed consent from the participant/guardian, any individual entering the survey was asked to fill in the standard PedsQL™ Generic Core Scale questionnaire. Besides, participants were asked to complete an information form about sociodemographic characteristics (age at enrollment, gender, weight, length, disease or disorder (for unhealthy controls), income, and geographical location). Moreover, for patients with NS, some data such as duration, the average number of hospitalizations per year, medications, complications (due to disease or treatment), and cumulative dose of glucocorticoid (CGCS) were specifically collected.
The final sample size included 60 NS patients, 81 healthy and 98 non-healthy controls selected based on fulfilling inclusion criteria. Chi-square or Fisher's exact tests were used to compare the categorical variables. Moreover, statistical differences among three groups were analyzed using analysis of variance (ANOVA) or Kruskal-Wallis test. P-values < 0.05 and confidence interval (CI) as %95 was considered statistically significant. Continues variables with normal distribution were expressed as the mean values, and standard deviation, and student's t-test and Mann-Whitney U-test were used to compare data with normal and abnormal distribution, respectively. Correlation among continuous variables related to demographic data, complications, clinical pictures, and HRQoL score was assessed for NS patients using correlation analysis. Statistical analysis was conducted using statistical package for social science (SPSS) software version 26.0 (SPSS Inc., Chicago, IL, USA).
4. Results
239 subjects, including 60 with NS, 98 with other chronic diseases, and 81 healthy children fulfilling inclusion criteria entered the study. The mean age of subjects was 9.8 ± 3.7, 9.7 ± 3.9, and 9.5 ± 2.7 years for the NS cohort, non-renal illness controls, and healthy controls, respectively. There was a male predominance in all three groups. The mean duration of NS was 48.3 ± 31.4. The number of medications taken by any patient with Ns was reported (1 to 10), and medications included prednisolone, cyclophosphamide, cyclosporine A, Tacrolimus, calcium, vitamin supplements, and anti-hypertensive medications. The cumulative dose of corticosteroid was calculated using patient information. Table 1, depicts demographic and clinical data of 3 groups.
| Parameter | Nephrotic Patients (N = 60) | Non-renal Illness Controls (N = 98) | Healthy Controls (N = 81) | P-Value |
|---|---|---|---|---|
| Age (y) | 9.8 ± 3.7 | 9.7 ± 3.9 | 9.5 ± 2.7 | 0.9 |
| Sex | 0.7 | |||
| Male | 35 | 56 | 51 | |
| Female | 25 | 42 | 30 | |
| Duration of illness (mo) | 48.3 ± 31.4 | - | - | - |
| Geographic location | 0.2 | |||
| Urban | 45 | 75 | 64 | |
| Rural | 4 | 6 | 1 | |
| Income | < 0.001 b | |||
| High | 2 | 1 | 0 | |
| Intermediate | 23 | 41 | 28 | |
| Low | 20 | 32 | 8 | |
| Weight (Kg) | 38.6 ± 19.6 | 32.5 ± 16.3 | 35.6 ± 14.2 | 0.1 |
| Length (Cm) | 135.7 ± 19.4 | 137.8 ± 22.7 | 135.5 ± 19.5 | 0.6 |
| Body mass index | 19.9 ± 6.5 | 18.5 ± 5.8 | 19.1 ± 5.3 | 0.4 |
| Clinical types of NS | - | - | - | |
| SDNS | 36 | |||
| SSNS | 8 | |||
| SRNS | 12 | |||
| Relapsing types of NS | - | - | - | |
| Frequent relapsing | 28 | |||
| Infrequent relapsing | 32 | |||
| Average number of hospitalizations per year | 0.95 ± 0.8 | - | - | - |
| CGCS | - | - | - | |
| Lesser than 1 gr/kg | 21 | |||
| More than 1 gr/kg | 24 | |||
| Number of medications, min -max | (1 - 103.3) ± 1.7 | - | - | - |
| CNIs receiving | - | - | - | |
| Yes | 18 | |||
| NO | 34 | |||
| Complications | - | - | - | |
| Blood pressure | 12 | |||
| Obesity | 15 | |||
| Gingival hyperplasia | 0 | |||
| Cushingoid manifestation | 13 |
Demographic and Clinical Data of Participants a
The mean scores of all PedsQL domains for patients and controls were compared with previously published normative data presented in Table 2. Patients with NS scored statistically significant values in comparison with normative subjects in physical, emotional as well as total domains (P < 0.05), but the differences in social and school functioning were not significant (P > 0.05) as opposed to non-healthy controls (NHC), whose difference of QOL scores with normative values were statistically significant in all domains, and difference among QOL scores for healthy controls and normative data were statistically significant in social and school functioning sectors (P < 0.05).
| Domains | Normative | Patients and Controls | P-Value |
|---|---|---|---|
| Total score | 5972 (82.9 ± 13.2) | ||
| NS | 60 (77.62 ± 15.8) | 0.048 b | |
| NHC | 98 (70.7 ± 17.4) | < 0.001 b | |
| HC | 81 (85.3 ± 8.5) | 0.1 | |
| Physical | 5962 (86.9 ± 13.9) | ||
| NS | 60 (80.65 ± 18.9) | 0.018 b | |
| NHC | 98 (70.1 ± 22.6) | < 0.001 b | |
| HC | 81 (86.5 ± 9.7) | 0.8 | |
| Emotional | 5961 (78.2 ± 18.6) | ||
| NS | 60 (67.9 ± 20.2) | < 0.001 b | |
| NHC | 98 (66.6 ± 20.1) | < 0.001 b | |
| HC | 81 (80.0 ± 14.4) | 0.3 | |
| Social | 5948 (84 ± 17.4) | ||
| NS | 60 (82.0 ± 15.9) | 0.3 b | |
| NHC | 98 (75.5 ± 20.2) | 0.011 b | |
| HC | 81 (88.6 ± 10.4) | 0.018 | |
| School | 5908 (79.9 ± 16.9) | ||
| NS | 51 (79.9 ± 18.6) | 0.9 | |
| NHC | 75 (72.9 ± 19.5) | 0.002 b | |
| HC | 70 (86.4 ± 12.6) | 0.007 b |
Comparison of PedsQL Scores and Normative Data
The mean scores for each domain were compared between the NS group and the controls and summarized in Table 3. The mean QOL score of the case cohort were lower than healthy controls and higher than non-healthy controls in all domains, with the difference being statistically significant for all sections (P < 0.05) except for emotional functioning of patients with NS compared to non-healthy controls (P > 0.05).
| Domains | Nephrotic Syndrome G. | Control Groups | P-Value |
|---|---|---|---|
| Total Score | 60 (77.62 ± 15.8) | ||
| NHC | 98 (70.7 ± 17.4) | 0.014 b | |
| HC | 81 (85.3 ± 8.5) | < 0.001 b | |
| Physical | 60 (80.65 ± 18.9) | ||
| NHC | 98 (70.1 ± 22.6) | 0.003 b | |
| HC | 81 (86.5 ± 9.7) | 0.017 b | |
| Emotional | 60 (67.9 ± 20.2) | ||
| NHC | 98 (66.6 ± 20.1) | 0.7 | |
| HC | 81 (80.0 ± 14.4) | < 0.001 b | |
| Social | 60 (82.0 ± 15.9) | ||
| NHC | 98 (75.5 ± 20.2) | 0.036b | |
| HC | 81 (88.6 ± 10.4) | 0.004b | |
| School | 51 (79.9 ± 18.6) | ||
| NHC | 75 (72.9 ± 19.5) | 0.048 b | |
| HC | 70 (86.4 ± 12.6) | 0.027 b |
PedsQL Scores in Patients and Controls a
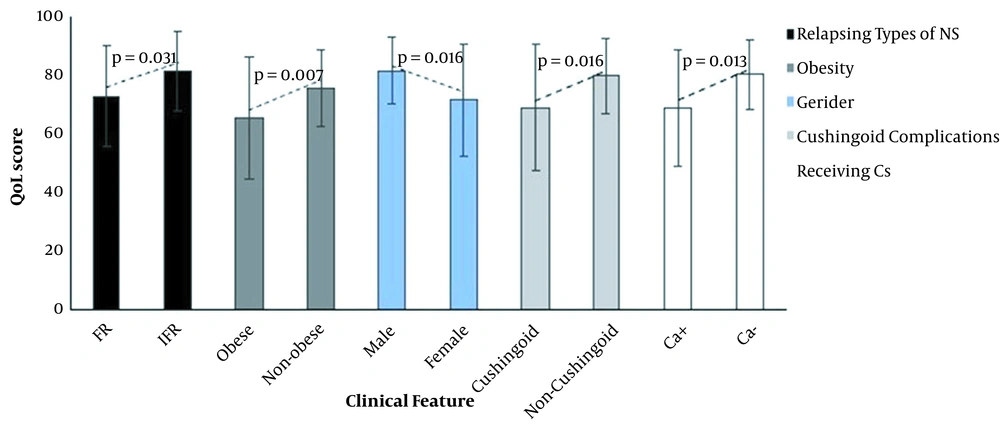
Comparing three clinical types of NS revealed that SRNS patients have the lowest QoL score compared to SDNS and SSNS, but differences were not statistically significant (P > 0.05). Analysis revealed that relapsing types of NS, Gender, Duration of illness, average hospital admissions per year, body weight and obesity, cushingoid complications, and receiving CNIs significantly affect the QoL score in patients with nephrotic syndrome (P < 0.05) (Figure 1) and also age, length, family income, geographical location, CGCS, number of medications received and blood pressure doesn't significantly influence the QoL score (P > 0.05). Pearson correlation demonstrated the duration of disease, average hospital admission per year and body weight were associated with the QOL total scores (Table 4).
| Parameter | PedsQL™ 4.0 Scores (Total); P Value (Pearson Correlation) |
|---|---|
| Gender (male/female) | 0.016 a |
| Duration (mo) | 0.004 (-0.4) a |
| Relapsing types of NS | 0.031 a |
| Average number of hospitalizations per year | 0.035 (-0.28) a |
| BMI | |
| Weight (kg) | 0.002 (-0.4) a |
| Length (cm) | 0.3 |
| Income | 0.06 |
| Geographical location | 0.6 |
| CGCS | 0.6 |
| Number of medications received | 0.5 (-0.085) |
| Receiving CNIs | 0.013 a |
| Complications | |
| Blood pressure | 0.6 |
| Obesity | 0.007 a |
| Gum hyperplasia | - |
| Cushingoid manifestation | 0.016 a |
Potential Predictors of QoL Scores in NS Patients
5. Discussion
Today, the focus of research on chronic diseases such as nephrotic syndrome is more on treatment and improvement of its clinical outcome, and it seems that the impact of this disease on the quality of life of these patients has been largely neglected. While the chronic nature of disease and exposure to corticosteroids and calcineurin inhibitors such as cyclosporine and tacrolimus and their complications, as well as the clinical features of the disease itself such as severe edema and treatment complications such as obesity, gingival hypertrophy, and hypertrichosis and frequent hospitalizations and absence from school to visit a doctor, on the other hand, can affect all aspects of a person's physical, emotional, psychological and school performance. In a way that its effects can extend to the next years of the child's life (7, 13). This issue can affect the patient's compliance with medical orders, especially in adolescence, and a better understanding of the HRQoL can improve the quality of clinical care and ultimately the disease management. "Ped`sQL4.0 Generic Core Scale" is a reliable, valuable and flexible tool that is widely used in pediatrics and fortunately its Persian translation is also published on the website of MAPI Research Institute. Its` reliability has been confirmed in Iranian children by the study of Amiri et al. (11).
In our cohort of patients with NS, there is a male predominance. Patients with steroid-resistant nephrotic syndrome accounted for 20% of the cohort, which was not reported in the study of Gheissari et al. (8). The results of studies on the effect of nephrotic syndrome on patients' HRQoL scores were different and sometimes contradictory in different studies. In 2004, Ruth et al. evaluated QOL in 45 children with steroid-sensitive nephrotic syndrome from the Netherlands and found that only social functioning was impaired (13). Similarly, QoL evaluation of 127 American children with the prevalent NS showed lower scores on social and school performance than those with incident NS (7). In India Mazahir et al. reported lower QoL scores for children with NS compared to healthy children, especially in school functioning (14). Surprisingly, Roussel and colleagues recently reported that children with SSNS and SRNS had high scores close to normal subjects (15). In the study of Gheissari et al., where the HRQoL score for 75 patients with nephrotic syndrome in Isfahan, Iran was compared with the score of 210 healthy individuals, the scores in all four sections were lower than their healthy counterparts (8). In our study, patients with nephrotic syndrome in physical, social, and educational fields and total HRQoL scores were lower than healthy controls and higher than controls with other chronic diseases. But the emotional HRQoL score was surprisingly low and close to that of the non-kidney control group, with the mean scores of 67.9 ± 20.2 and 66.6 ± 20.1, respectively (P > 0.05), which can be alarming and requires special attention from health care providers, including nephrologists and psychologists. These differences in the results among studies conducted in developed and developing countries can be attributed to differences in sample size, different inclusion and exclusion criteria, and differences in the quality of care provided in different countries.
This study is the first in Iran to examine the quality of life of children with nephrotic syndrome and compare with that of healthy people and people with other chronic diseases. In terms of the relationship of the clinical subgroup of disease concerning steroid response, our study did not show a relationship that in this respect, our findings were consistent with the study of Agrwal et al. and Selewski et al. (7, 16). These findings suggest that nephrotic syndrome, regardless of disease phenotype, can affect different aspects of a child's quality of life; though restricted sample size can be an obstacle here to make such a deduction.
Besides, a general evaluation was performed on the possible relationship between clinical features and disease complications and HRQoL scores. Based on our findings, the duration of disease and the number of recurrences had a negative effect on HRQoL scores, which was consistent with the findings of Rahman et al., who reported that longer disease duration and more recurrences were major variables associated with low HRQoL scores (17). The findings of Selewski et al. and Solarin et al. were also consistent (7, 18). Didsbury et al carried out a review article to assess the possible relationship between socio-economic variables an QoL scores of children with chronic diseases and found out a significant relationship, which is compatible with our findinges and findings of Mishra et al. in India (19, 20).
We examined other possible variables in relation to HRQoL scores. These include the number of medications, the cumulative dose of corticosteroids, complications of disease (such as obesity), complications associated with specific treatments (such as secondary gingival hypertrophy due to cyclosporine, and secondary cushingoid complications due to corticosteroids). There was a significant correlation between Cushingoid features and HRQoL scores. According to our study, the number of drugs received and the cumulative dose of steroids was not related to HRQoL, which was consistent with the findings of a study by Selewski et al. (7). The complications of gingival hypertrophy showed no association with quality of life, possibly due to a random error. In fact, we did not have any patients with this complication. Hypertension (HTN) did not show a correlation with HRQoL scores, which was consistent with the findings of Gheissari et al. In Isfahan (8). This may be due to the asymptomatic presentation of HTN in this age group.
Comparing HRQoL scores with published normal data showed that children with nephrotic syndrome had lower scores in terms of physical, emotional, and overall performance than the normative data. At the same time, the patients included in the study had higher emotional scores that did not differ significantly from the normal values. Surprisingly, patients of our cohort with the nephrotic syndrome had higher scores in terms of social and academic performance, though this difference was not statistically significant, this difference can be attributed to the different cultural and ethnic norms between different cultural backgrounds. Part of the reason for the low physical function scores of these patients can be attributed to the high prevalence of obesity in this population (2).
The present study is a different study with this design that has been performed among Iranian children with nephrotic syndrome and compared a relatively large group of patients with nephrotic syndrome with two control groups consisting of healthy counterparts and patients with other chronic diseases according to HRQoL. This study also tried to examine many demographic details, clinical characteristics and therapeutic aspects, and complications related to the disease itself, and complications resulting from treatment and their relationship with HRQoL which is also unique in this regard.
Weaknesses of this study include its being conducted in a single-center, lack of standard Iranian data for comparison, and lack of long-term follow-up for re-evaluation. We suggest that a study to be conducted to obtain normal data for the Iranian children's population to provide a basis for more detailed studies in the future.
5.1. Conclusions
This and similar studies show that although nephrotic syndrome is curable, it can physically, emotionally, socially, and academically affect all aspects of the patients` lives. Timely identification of the effects of nephrotic syndrome may be the first step in taking the necessary actions to reduce the devastating effects of this disease. Therefore, we suggest that the Ped’sQL 4.0 questionnaire and similar tools, which have shown high efficiency and reliability in assessing HRQoL in children, be routinely used in clinical practice, especially for patients with nephrotic syndrome. It is also recommended that the comprehensive care of these patients can be addressed in multidisciplinary teams consisting of pediatric nephrologists, psychologists, and psychiatrists.