1. Background
Five million children die annually due to preventable diseases across the world (1). In order to decrease preventable child deaths, a standard process is required to identify the exact causes of death (COD) (2). Research in well-developed health systems revealed that accurate data were unavailable for 10% of child deaths (3, 4). Misclassification has been reported in low- and middle-income countries, such as South Africa, Mexico, Thailand, China, and Tonga, ranging from 30% to 80%. Concerns also exist about the accuracy of mortality data in Iran (5-9). A study in Iran revealed misclassification in half of the cardiovascular disease cases and featured a noticeable discrepancy between actual and registered COD (10).
The World Health Organization (WHO) recommends that the international death certificate should include the direct COD (immediate and antecedent COD), the period between the onset of the COD and death, and the deceased's personal information and other significant circumstances contributing to death but not associated to the direct COD (11). Therefore, disease mechanisms or immediate and intermediate causes might be misclassified instead of the underlying COD (12). A trained physician or healthcare provider should provide a correct sequence of diseases for identifying exact causes based on the 10th edition of the International Classification of Diseases (ICD10) (13). An accurate death certificate as an essential source of mortality data is crucial for assessing needs, prioritizing activities, investing limited resources, monitoring public health interventions, and conducting epidemiological research (10, 14). The lack of valid estimates can challenge regional and global disease burden and management strategies at a large level (15).
2. Objectives
To our knowledge, this is the first study in Iran to highlight the importance of accurate COD targeting early childhood (1 - 59 months). The study aimed to measure the sensitivity and positive predictive value (PPV) of children's death certificates.
3. Methods
3.1. Sampling Plan and Study Sample
This cross-sectional hospital-based study was conducted in Motahari hospital, Urmia University of Medical Sciences, West Azerbaijan province, Iran. The hospital is a children's specialized hospital and the focal point for pediatric special and sub-special diagnostic and treatment services in Northwest Iran. Data were obtained from the hospital information system (HIS) for all deaths in children aged 1 - 59 months between 2011 and 2018. The exclusion criteria were a lack of complete information. Medical records needed to contain a fully reported clinical history, a medical examination report, and one of the following clinical aids for diagnosis: Radiology, electrocardiography, computerized tomography scan, or laboratory reports. Out of 594 deaths, adequate information was unavailable for 14 (2.36%). This study was approved under an ethical approval code (01-66-2606) by the Urmia University of Medical Sciences Ethics Committee. We used the STROBE cross-sectional reporting guidelines as the assessment tool (16).
3.2. Processing and Data Collection
Two trained pediatricians with more than 20 years of experience reviewed death certificates and identified the final CODs using ICD10 codes and clinical guidelines. If the COD was ambiguous, the general agreement of pediatricians was applied. Pediatricians were blinded to the registered COD in the HIS and death certificates.
3.3. Statistical Analyses
The agreement was measured between causes assigned by pediatricians as a gold standard and registered causes in HIS for 580 cases. Errors were classified using a misclassification matrix. Minor errors included using abbreviations, repeated and illegible expressions, and the absence of time intervals. Major errors included missed underlying COD, competing CODs, and inappropriate sequencing of COD. Certificates with no medical condition known as underlying COD were referred to as missing underlying COD. Competing causes occur when two or more factors could similarly be valid underlying CODs from a clinical standpoint. Inappropriate sequencing was referred to certificates that included several CODs without any medically acceptable sequences.
Sensitivity and PPV were calculated using multiple causes of death to evaluate the agreement between HIS and pediatricians. The sensitivity of a test is defined as the percentage of people with the disease who have a positive result. The PPV is the probability of patients who have a positive test result really having the disease. Sensitivity and PPV express delicately different meanings regarding the ability of the HIS to identify deaths due to a specific cause. Sensitivity evaluates, from an epidemiological viewpoint, the probability that the HIS correctly identifies actual deaths from the cause of interest, while PPV, from a clinical viewpoint, assesses the actual chance of death from this cause if diagnosed by the HIS. Cause-specific mortality fraction was estimated based on the final underlying CODs obtained from pediatricians' reviews.
4. Results
A total of 580 death certificates were investigated. Of them, 312 (53.79%) were male, and the mean age at death was 12.19 ± 12.7 months. The HIS registered 1,596 causes for 580 deaths. Each death certificate had 2.7 causes of death on average. The pediatricians identified 37.4% (n = 597) of codes as minor errors. The total number of codes decreased to 999 for 580 deaths. Next, the pediatricians identified 26% (419 of 1,596) of codes as major errors. Each certificate was assigned a single code as an underlying COD, and the total number of codes reached 580. The percentage agreement between the HIS and pediatricians was 40.54%. The total sensitivity of the HIS was 43.27% for underlying CODs, with a PPV of 39.37%. The sensitivity and PPV are represented in Table 1. As the most identified overestimations, "cardiac arrest, cause unspecified" had the highest prevalence in the HIS with 27% (429 of 1,596). This figure decreased to 4.9% (49 of 999) after identifying minor errors. By excluding major errors, cardiovascular diseases were the underlying CODs in a mere 5.7% of deaths (33 of 580) (Table 1).
| Variables | Crude Outcome of Hospital Information System (HIS); No. (%) | After Excluding Minor Errors; No (%) | Pediatricians (Multiple Causes Based on Matrix); No. (%) | After Excluding Major Errors (Single Cause); No. (%) | Sensitivity | PPV |
|---|---|---|---|---|---|---|
| Respiratory diseases and pneumonia | 198 (12.4) | 170 (17.0) | 162 (16.2) | 127 (21.9) | 48.77 | 46.47 |
| Congenital anomalies | 199 (12.5) | 158 (15.8) | 154 (15.4) | 91 (15.7) | 42.21 | 41.14 |
| Sepsis and other systemic infections | 171 (10.7) | 155 (15.5) | 135 (13.5) | 77 (13.3) | 40.0 | 34.84 |
| Neurological diseases and seizures | 134 (8.4) | 114 (11.4) | 118 (11.8) | 50 (8.6) | 34.75 | 35.96 |
| Metabolic and nutritional disorders | 109 (6.8) | 100 (10.0) | 112 (11.2) | 39 (6.7) | 25.0 | 28.0 |
| Cancers and blood diseases | 64 (4.0) | 56 (5.6) | 54 (5.4) | 38 (6.6) | 64.81 | 62.5 |
| Cardiovascular disease | 429 (26.9) | 49 (4.9) | 42 (4.2) | 33 (5.7) | 61.9 | 53.06 |
| Digestive and liver disease | 52 (3.3) | 42 (4.2) | 55 (5.5) | 29 (5.0) | 23.64 | 30.95 |
| RDS and prematurity | 85 (5.3) | 39 (3.9) | 61 (6.1) | 25 (4.3) | 27.87 | 43.59 |
| Prenatal problems | 41 (2.6) | 38 (3.8) | 28 (2.8) | 25 (4.3) | 32.14 | 23.68 |
| Accidents, injuries, and poisoning | 48 (3.0) | 32 (3.2) | 30 (3.0) | 21 (3.6) | 70.0 | 65.63 |
| Diarrhea and dehydration | 45 (2.8) | 29 (2.9) | 33 (3.3) | 18 (3.1) | 18.18 | 20.69 |
| Kidney and urinary tract infections | 21 (1.3) | 17 (1.7) | 15 (1.5) | 7 (1.21) | 73.33 | 64.71 |
| Total | 1596 | 999 | 999 | 580 | 43.27 | 39.37 |
Comparison of Underlying Causes of Death Between the Hospital Information System and Pediatrician Reviews, 2011 - 2018
The HIS assigned respiratory diseases in 170 death certificates, but based on further reviews, the pediatricians found that only 46.5% (n = 79) of them were accurately assigned. In this regard, the pediatricians assigned about 16.5% (n = 28) as neurological diseases and seizures, 12.4% (n = 21) as congenital anomalies, 7% (n = 12) as digestive and nutritional disorders, 4.7% (n = 8) as diarrhea and dehydration, 4.1% (n = 7) as cancers and blood diseases, 4.1% (n = 7) as cardiovascular disease, 2.35% (n = 4) as metabolic and liver diseases, and 2.35% (n = 4) as accidents, injuries, and poisoning (horizontal direction in Table 2). Notwithstanding, the most identified misclassification was the underestimation of respiratory disease and pneumonia by the HIS. Our pediatricians assigned 21.9% (7 of 32) to accidents, injuries, and poisoning, 21.1% (24 of 114) to neurological disease, 17.1% (27 of 158) to congenital malformations, 16% (16 of 100) to digestive and nutritional disorders, and 10.34% (3 of 29) to diarrhea and dehydration as respiratory disease and pneumonia (vertical direction in Table 2).
| Hospital Information System (HIS) Cause of Death | Causes of Death by Pediatricians; No. (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
| 1. Respiratory diseases /pneumonia | 170 | 79 (46.5) | 21 (12.4) | 0 | 28 (16.5) | 12 (7) | 7 (4.1) | 7 (4.1) | 4 (2.35) | 0 | 0 | 4 (2.35) | 8 (4.7) | 0 |
| 2. Congenital anomalies | 158 | 27 (17.1) | 65 (41.1) | 14 (8.9) | 8 (5.1) | 8 (5.1) | 0 | 6 (3.8) | 4 (2.5) | 12 (7.6) | 5 (3.2) | 0 | 7 (4.4) | 2 (1.3) |
| 3. Sepsis/other systemic infection | 155 | 0 | 27 (17.4) | 54 (34.8) | 13 (8.4) | 20 (12.9) | 9 (5.8) | 0 | 13 (8.4) | 17 (11.0) | 0 | 1 (0.6) | 0 | 1 (0.6) |
| 4. Neurological disease/seizure | 114 | 24 (21.1) | 9 (7.9) | 13 (11.4) | 41 (36.0) | 9 (7.9) | 0 | 3 (2.6) | 0 | 3 (2.6) | 4 (3.5) | 4 (3.5) | 4 (3.5) | 0 |
| 5. Digestive /nutritional disorders | 100 | 16 (16.0) | 6 (6.0) | 17 (17.0) | 12 (12.0) | 28 (28.0) | 3 (3.0) | 0 | 8 (8.0) | 2 (2.0) | 3 (3.0) | 0 | 4 (4.0) | 1 (1) |
| 6. Cancers/blood diseases | 56 | 4 (7.1) | 0 | 10 (17.9) | 0 | 7 (12.5) | 35 (62.5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7. Cardiovascu-lar disease | 49 | 0 | 6 (12.2) | 5 (10.2) | 4 (8.2) | 1 (2) | 0 | 26 (53.1) | 7 (14.3) | 0 | 0 | 0 | 0 | 0 |
| 8. Metabolic/liver disease | 42 | 2 (4.8) | 3 (7.1) | 7 (16.7) | 0 | 13 (3.95) | 0 | 0 | 13 (30.95) | 0 | 0 | 0 | 4 (9.5) | 0 |
| 9. RDS/prematurity | 39 | 0 | 7 (17.94) | 8 (20.52) | 0 | 0 | 0 | 0 | 0 | 17 (43.6) | 7 (17.94) | 0 | 0 | 0 |
| 10. Prenatal problems | 38 | 0 | 5 (13.15) | 7 (18.42) | 2 (5.26) | 5 (13.15) | 0 | 0 | 0 | 10 (26.32) | 9 (23.7) | 0 | 0 | 0 |
| 11. Accidents/poisoning | 32 | 7 (21.9) | 0 | 0 | 4 (12.5) | 0 | 0 | 0 | 0 | 0 | 0 | 21 (65.6) | 0 | 0 |
| 12. Diarrhea/dehydration | 29 | 3 (10.34) | 3 (10.34) | 0 | 6 (20.7) | 5 (17.22) | 0 | 0 | 6 (20.7) | 0 | 0 | 0 | 6 (20.7) | 0 |
| 13. Kidney/UTI | 17 | 0 | 2 (11.8) | 0 | 0 | 4 (23.5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 (64.7) |
| Total | 999 | 162 | 154 | 135 | 118 | 112 | 54 | 42 | 55 | 61 | 28 | 30 | 33 | 15 |
Diagnostic Misclassification Patterns for the Total Multiple Causes of Death, 2011 - 2018
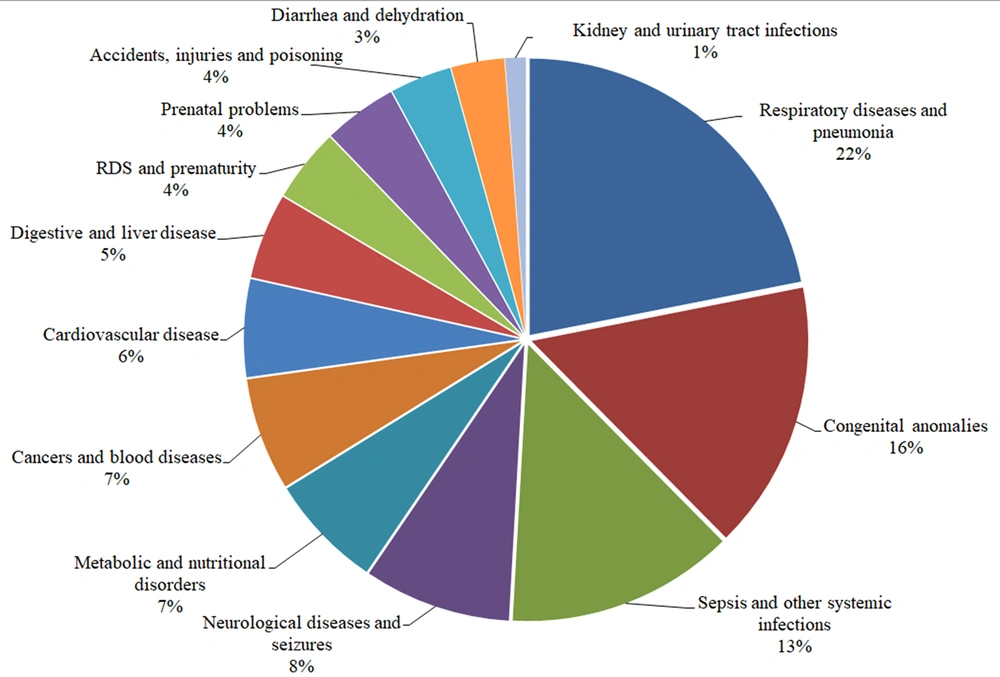
The most common causes of death, according to the pediatricians' decisions, were respiratory disease and pneumonia (n = 127, 21.9%), congenital anomalies (n = 91, 15.7%), and sepsis and other systemic infections (n = 77, 13.3%) (Figure 1). In terms of cause-specific mortality fraction, the proportionate mortality of congenital anomalies decreased, while the relative importance of pneumonia, respiratory disease, and sepsis increased.
5. Discussion
The overestimation of cardiovascular diseases and the underestimation of respiratory system diseases were the most frequent errors in this study. The sensitivity and PPV of the HIS were 43.27 and 39.37%, respectively. Approximately half of the death certificates were not valid. Like our study, a study by Khosravi in Iran showed that 25% of death certificates in hospitals were useless and consisted of vague or ill-defined causes of death 10. Other studies also presented errors concerning the recorded causes of death. A study in Saudi Arabia declared that 99.89% of death certificates in a hospital were erroneous (17). According to another study in the United Kingdom in 2002, 55% of death certificates were of the lowest standards (18). In India and Vermont state, 78.1% and 82% of death certificates contained errors, respectively (19, 20). The various reported rates can be due to the lack of a standard international methodology and framework for the critical appraisal of death certificates.
In line with studies in the Eastern Mediterranean, African, and Western Pacific regions, our study indicated pneumonia and respiratory diseases, congenital malformations, sepsis, and other systemic infections as the top three causes of death among children aged 1 - 59 months (21, 22) However, studies by Evazpoor and Rahbar in Iran contradicted our results, mainly due to the lower rates of respiratory system diseases and pneumonia (14, 23). Although the prevalence of non-infectious diseases has increased worldwide in children under five years of age, 40% of child mortalities in EMRO still lie with pneumonia and diarrhea, which cannot be disregarded (21, 24). Overall, our findings revealed that every death certificate included almost three competitive causes of death. Studies in Iran (25), India (26), and Palestine (27) reported a high percentage of competing causes in death certificates. Many of these errors can be due to the lack of training courses and failure to follow the principles of completing death certificates. In this study, "cardiovascular disease, unspecified" was registered as a competitive or leading cause of death in 75% of certificates. 17.1% of death certificates registered as congenital malformations, 21.1% of death certificates registered as neurological diseases, and 16% of death certificates registered as metabolic diseases were assigned as respiratory diseases and pneumonia by pediatricians. According to our pediatricians' decisions, the most common cause of death was respiratory disease and pneumonia. A previous study concluded that pneumonia could never be taken into account as the primary cause of death. In other words, if pneumonia is reported as the underlying cause, it is, in fact, a consequence of other ailments (28). Nonetheless, in line with our study, pneumonia was reported as the confirmed underlying cause in 77% of death certificates in a study in Sweden 4. The high capability of the current ICD instructions in identifying a valid cause of death could be considered an efficient method for identifying secondary pneumonia. Hence, pneumonia might be a perfectly valid underlying cause in certain cases.
Former research in different countries recognized several factors affecting the validity of DCs, such as the quality of undergraduate and postgraduate training, patient features and disease responsible for the death, hospital type and size, and rules administrating death certification (29, 30). Studies showed that the mean time spent recording COD and completing DCs in the medical school curriculum was insufficient. Also, more than two-thirds of students did not complete death certificates alone. In addition, a lack of adequate coding knowledge and its importance as a public health monitoring indicator could be a significant factor (31, 32). It has also been reported that physicians cannot reliably distinguish the cause of death from the state of death in patients. Sometimes coding responsibility is assigned to staff other than physicians, and physicians only supervise it. Training courses for completing death certificates are not held regularly (29). More training and effort are needed to heighten physicians' awareness of the importance of death certificate completion and coding. Based on previous studies, we need interventions consisting of training packages, workshops, professional development activities, and published materials (33). A systematic review recognized that interactive education and feedback for death certifiers should be considered the chief requirement for valid mortality (34). Standardizing instructions and methods for collecting COD data is recommended to achieve more significant harmonization in death certification and enhance the comparability of epidemiological data (31).
To the best of our knowledge, this is the first study in Iran reviewing death certificates and assigning the causes of death in children under five years of age to determine the causes of death, so it is a unique study at a regional level. However, the results should be interpreted concerning limitations such as selection bias due to a single-center population and retrospective design. Also, using different definitions, guidelines, and changes in national coding methods can affect the validity of our results (35). Classification of the causes in 13 broad diagnostic groups would not be efficiently discriminating. In order to achieve more reliable and accurate mortality statistics, classification should be based on more detailed and homogeneous groups of death causes. Given that the study was conducted in a single hospital, the inability to generalize the findings to the whole country can be another limitation of this study.
5.1. Conclusions
In our study, many deaths were registered inaccurately on death certificates. Therefore, there is an urgent need to improve the quality of death certificates and registration of death causes. The available data should be used with caution for planning and policy-making until reaching a desirable quality. Therefore, more extensive studies are strongly required in this field.