1. Background
Emergency medical services (EMS) are critical for identifying the condition of individuals experiencing an emergency, immediately performing the necessary first aid, and rapidly transferring patients to an appropriate medical institution (1). Since the quality of EMS is directly correlated with the prognosis of emergency patients, many countries strive to construct and maintain well-organized EMS (2-6). Understanding the clinical characteristics of patients transported to the emergency department (ED) by EMS and environmental factors that might affect their EMS use could assist authorities in properly arranging their facilities and personnel and help clinicians prepare for emergency patients. As a result, there have been increasing efforts to identify the clinical characteristics of patients transported to the ED by EMS (1, 7, 8). Although few, some researchers have also attempted to determine whether the characteristics of pediatric emergency patients are distinct from those of adult patients (9, 10).
Diseases or injuries that require urgent treatment can be caused by patient-related factors but can also be significantly affected by environmental factors. As interest in the impacts of climate change and environmental pollution on human health has increased, a growing number of studies addressing the influence of meteorological factors and air pollutants on human health and ED visits has been reported (11-16). However, there are few reports of the impacts of these environmental factors on ED visits among pediatric patients, especially concerning EMS usage patterns.
2. Objectives
In this study, we assessed the clinical characteristics of pediatric patients transported to the ED by EMS and analyzed the impacts of meteorological factors on EMS use in this population.
3. Methods
3.1. Study Population and Materials
A single-center, retrospective, observational study was designed to identify the factors affecting EMS use. We reviewed the medical records of pediatric patients younger than 19 years who visited the ED of Samsung Changwon Hospital between January 2005 and December 2019. Changwon is a city located on the southeast coast of Korea (35° 23'N, 128° 68'E), with an annual average temperature of 14.9°C and average annual precipitation of 1,545.4 mm. During this period, the annual average number of patients who visited the ED was 36,994, and that of pediatric patients younger than 19 years was 9,292, accounting for 25.12% of all patients who visited the ED. A total of 146,592 children visited the ED during the study period, of whom 139,383 were analyzed after excluding 7,209 who visited the ED repeatedly on the same day with the same symptoms (n = 1,497 patients; 1.0%) or for whom we were unable to confirm EMS use due to missing records (n = 5,712 patients; 3.9%). This study was approved by the Institutional Review Board (IRB) of Samsung Changwon Hospital (IRB No. SCMC 2020-08-004).
3.2. Clinical Characteristics and Meteorological Factors
Clinical characteristics of age; sex; Korean triage and acuity scale (KTAS); Glasgow Coma Scale (GCS); cardiopulmonary resuscitation (CPR); hospitalization; admission to intensive care unit (ICU); duration of hospitalization; use of ventilator; mortality; day of the week of visit; and disease classification according to the International Classification of Diseases, 10th revision (ICD-10) were included in the survey. Patient age was divided into five categories: younger than one year, one to four years, five to nine years, 10 to 14 years, and 15 to 18 years. The diagnosis determined at the ED was classified into 19 categories based on ICD-10 code(s). Severity of disease was estimated using the KTAS and GCS. The KTAS is a classification that categorizes the severity of emergency patients (17) into five levels, with lower levels corresponding to greater severity of disease. The GCS suggests a better neurological condition with higher scores.
Season, daily mean temperature, diurnal temperature range (DTR), precipitation, and mean concentrations of air pollutants (SO2, CO, O3, NO2, and PM10) were analyzed as meteorological factors. Meteorological data were obtained from the website of the Korean Metrological Administration (http://www.kma.go.kr), and the concentrations of air pollutants were acquired from the Korean Ministry of Environment (http://www.airkorea.or.kr). Spring, summer, autumn, and winter were defined as March-May, June-August, September-November, and December-February, respectively. The mean temperature and DTR were defined as the average value and difference between the maximum and minimum temperatures of the day, respectively. The DTR and precipitation were each divided into four categories (< 5°C, 5 - 9.9°C, 10 - 14.9°C, and ≥ 15°C and < 5 mm, 5 - 14.9 mm, 15 - 39.9 mm, and ≥ 40 mm, respectively). Air pollutants were measured hourly at a monitoring station located 0.4 km from the hospital, and the daily mean concentration of each pollutant was calculated from the recorded values.
3.3. Statistical Analysis
All statistical analyses were conducted using Stata 15.1 (Stata Corporation, College Station, TX, USA). Descriptive statistics were reported as mean and standard deviation or median and interquartile range (IQR) values for continuous variables and frequency and percentage values for categorical variables. An independent t-test, the Mann–Whitney U test, and Pearson’s chi-square test were used to compare differences between the EMS and non-EMS groups. For a comparison of the distribution of visit times to the ED, the Kolmogorov–Smirnov test was performed. We compared the EMS group and non-EMS group to investigate the impacts of clinical and meteorological factors on EMS use with a multivariable logistic regression model adjusted for sex; age; type of disease; KTAS and GCS scores; season; mean temperature; DTR; precipitation; and concentrations of SO2, CO, O3, NO2, and PM10. A statistically significant difference was defined as P < 0.05.
4. Results
4.1. Comparison of Clinical Characteristics Between the EMS and Non-EMS Groups
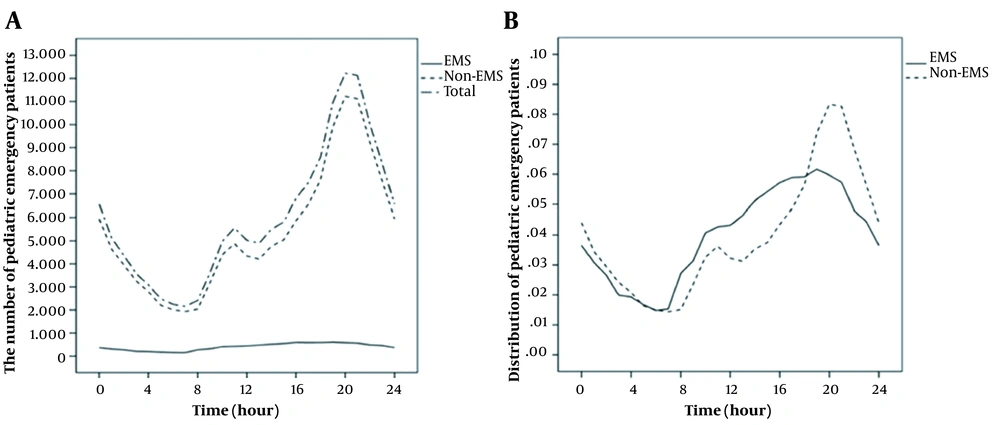
Of the 139,383 total patients, 9,770 (7.01%) were transported to the ED by EMS, while 129,613 (92.99%) arrived by other means such as private cars or public transportation (Table 1). Male patients totaled 62.10% of the EMS group and 57.52% of the non-EMS group (P < 0.001). The median age of the EMS group was eight years, while that of the non-EMS group was four years (P < 0.001). In particular, the percentage of patients older than 10 years was greater in the EMS group than in the non-EMS group (37.97% vs. 17.45%). The median KTAS scores of 3 in the EMS group and 4 in the non-EMS group showed a significant difference (P < 0.001), while the median GCS score was 15 in both groups. However, when this most frequent score in both groups (91.63% vs. 99.66%) was excluded, the median GCS score was lower in the EMS group (9 vs. 12; P < 0.001). The percentages of patients with adverse outcomes of CPR (0.98% vs. 0.02%; P < 0.001), hospitalization (45.34% vs. 16.98%; P < 0.001), admission to ICU (10.97% vs. 0.45%; P < 0.001), use of ventilator (4.24% vs. 0.07%; P < 0.001), median duration of hospitalization (5 days vs. 4 days; P < 0.001), death in the ED (0.87% vs. 0.01%; P < 0.001), and death during hospitalization (1.72% vs. 0.10%; P < 0.001) were all greater in the EMS group. The percentage of patients who visited the ED on holidays was higher in the non-EMS group (49.64% vs. 35.31%; P < 0.001). The distribution of visit times was significantly different between the two groups, with more visits occurring at night in the non-EMS group (Figure 1).
| Overall (N = 139,383) | Non-EMS (N = 129,613) | EMS (N = 9,770) | P-Value | |
|---|---|---|---|---|
| Sex | < 0.001 | |||
| Female | 58,767 (42,16) | 55,064 (42,48) | 3,703 (37.90) | |
| Male | 80,616 (57.84) | 74,549 (57.52) | 6,067 (62.10) | |
| Age, y (median, IQR) | 4 (2 - 9) | 4 (2 - 8) | 8 (3 - 15) | < 0.001 |
| < 1 | 25,858 (18.55) | 24,257 (18.71) | 1,601 (16.39) | < 0.001 |
| 1 - 4 | 63,688 (45.69) | 60,819 (46.92) | 2,869 (29.37) | < 0.001 |
| 5 - 9 | 23,502 (16.86) | 21,912 (16.91) | 1,590 (16.27) | 0.108 |
| 10 - 14 | 13,493 (9.68) | 11,994 (9.25) | 1,499 (15.34) | < 0.001 |
| 15 - 18 | 12,842 (9.21) | 10,631 (8.20) | 2,211 (22.63) | < 0.001 |
| KTAS a (median, IQR) | 4 (3 - 4) | 4(3 - 4) | 3(3 - 4) | < 0.001 |
| GCS b (median, IQR) | 15 (15 - 15) | 15 (15 - 15) | 15 (15 - 15) | < 0.001 |
| CPR | 124 (0.09) | 28 (0.02) | 96 (0.98) | < 0.001 |
| Hospitalization | 26,444 (18.97) | 22,014 (16.98) | 4,430 (45.34) | < 0.001 |
| Duration of hospitalization, d (median, IQR) | 4 (3 - 6) | 4 (3 - 6) | 5 (3 - 10) | < 0.001 |
| Admission to ICU | 1,660 (1.19) | 588 (0.45) | 1,072 (10.97) | < 0.001 |
| Use of ventilator | 501 (0.36) | 87 (0.07) | 414 (4.24) | < 0.001 |
| Death in ED | 100 (0.07) | 15 (0.01) | 85 (0.87) | < 0.001 |
| Death | 304 (0.22) | 136 (0.10) | 168 (1.72) | < 0.001 |
| Day of the week | < 0.001 | |||
| Monday | 17,468 (21.53) | 16,136 (12.45) | 1,332 (13.63) | |
| Tuesday | 15,604 (11.20) | 14,332 (11.06) | 1,272 (13.02) | |
| Wednesday | 15,533 (11.14) | 14,253 (11.00) | 1,280 (13.10) | |
| Thursday | 15,623 (11.21) | 14,255 (11.00) | 1,368 (14.00) | |
| Friday | 15,863 (11.38) | 14,451 (11.15) | 1,412 (14.45) | |
| Saturday | 23,645 (16.96) | 22,085 (17.04) | 1,560 (15.97) | |
| Sunday | 35,647 (25.57) | 34,101 (26.31) | 1,546 (15.82) | |
| Holiday c | 67,787 (48.63) | 64,337 (49.64) | 3,450 (35.31) | < 0.001 |
Abbreviations: EMS, emergency medical services; IQR, interquartile range; KTAS, Korean triage and acuity scale; GCS, Glasgow coma scale; CPR, cardiopulmonary resuscitation; ICU, intensive care unit; ED, emergency department.
a Beginning in 2016. Only 48,404 patients (34.73% of all patients) who visited an ED since 2016 were included in this analysis.
b Only 91,864 (65.91% of all patients) were analyzed due to missing records.
c Saturdays, sundays, and national holidays
Difference in distribution of ED visit times between the EMS group and the non-EMS group. (A) The number of patients who visited the ED by time. (B) In order to directly compare the two groups, we calculated the ratio of the number of patients who visited by time to the total number of patients in each group. The visit time of the EMS group was relatively more widely distributed, while that of the non-EMS group was concentrated at night. The difference in visit times between the two groups was statistically significant by the Kolmogorov–Smirnov test (P < 0.001).
4.2. Comparison of Disease Classifications Between the EMS and Non-EMS Groups
The overall distribution of disease among the included patients is shown in Table 2. The distribution of diseases in the non-EMS group was similar to the overall distribution of diseases in the study population. Although general symptoms and signs (ICD-10 code R, 38.5%) was the most common type of disease in both groups, the percentage of injury and poisoning (S/T) was about two-fold greater (37.65% vs. 18.96%) and that of respiratory disease (J) was about four times lesser (4.75% vs. 18.22%) in the EMS group. In addition, infectious disease (A/B) and digestive diseases (K), which occupied the fourth and fifth ranks (8.66% and 3.84%) in the non-EMS group, respectively, were the fifth- and seventh-ranked diseases (2.17% and 2.09%) in the EMS group. In contrast, perinatal problem (P) and neurologic disease (G), which accounted for only 0.56% and 0.51% in the non-EMS group, respectively, were ranked fourth (4.48%) and fifth (2.17%) in the EMS group.
| Code | ICD-10 | Overall (N = 139,383) | Non-EMS (N = 129,613) | EMS (N = 9,770) | P-Value |
|---|---|---|---|---|---|
| R | Symptoms, signs, and abnormal clinical and laboratory findings, NEC | 53,587 (38.5) | 49,593 (38.26) | 3,994 (40.88) | < 0.001 |
| S/T | Injury, poisoning, and certain other consequences of external causes | 28,259 (20.27) | 24,581 (18.96) | 3,678 (37.65) | < 0.001 |
| J | Diseases of the respiratory system | 24,077 (17.27) | 23,613 (18.22) | 464 (4.75) | < 0.001 |
| A/B | Certain infectious and parasitic diseases | 11,438 (8.21) | 11,226 (8.66) | 212 (2.17) | < 0.001 |
| K | Diseases of the digestive system | 5,176 (3.71) | 4,972 (3.84) | 204 (2.09) | < 0.001 |
| L | Diseases of the skin and subcutaneous tissue | 4,739 (3.40) | 4,699 (3.63) | 40 (0.41) | < 0.001 |
| H | Diseases of the eye, adnexa, ear, or mastoid process | 4,202 (3.01) | 4,158 (3.21) | 44 (0.45) | < 0.001 |
| P | Certain conditions originating in the perinatal period | 1,170 (0.84) | 732 (0.56) | 438 (4.48) | < 0.001 |
| G | Diseases of the nervous system | 871 (0.62) | 659 (0.51) | 212 (2.17) | < 0.001 |
| Other | 5,864 (4.21) | 5,380 (4.15) | 484 (4.95) | < 0.001 |
Abbreviations: ICD-10, International Classification of Diseases, 10th revision; EMS, emergency medical service; NEC, not elsewhere classified.
4.3. Comparison of Meteorological Factors Between the EMS and Non-EMS Groups
The percentage of patients in the EMS group increased in the summer (26.31%) and decreased in the winter (23.22%; Table 3). The opposite pattern was found in the non-EMS group (24.30% in summer and 25.18% in winter). The mean temperature on days the patients in the EMS group were transported to the ED was 15.03°C, while that in the non-EMS group was 14.74°C. The percentage of patients who visited the ED on rainy days was 31.32% in the EMS group and 32.39% in the non-EMS group. The mean concentrations of SO2, CO, NO2, and PM10 on the day of ED visit in the EMS group were greater than those of the non-EMS group.
| Overall (N = 139,383) | Non-EMS (N = 129,613) | EMS (N = 9,770) | P-Value | |
|---|---|---|---|---|
| Season | < 0.001 | |||
| Spring | 36,106 (25.90) | 33,574 (25.90) | 2,532 (25.92) | |
| Summer | 34,092 (24.46) | 31,516 (24.32) | 2,576 (26.37) | |
| Autumn | 34,281 (24.59) | 31,892 (24.61) | 2,389 (24.45) | |
| Winter | 34,904 (25.04) | 32,631 (25.18) | 2,273 (23.27) | |
| Mean temperature | 14.76 ± 8.76 | 14.74 ± 8.76 | 15.03 ± 8.70 | 0.002 |
| DTR (°C) | 8.64 ± 2.89 | 8.64 ± 2.89 | 8.67 ± 2.85 | 0.200 |
| < 5 | 16,656 (11.95) | 15,541 (11.99) | 1,115 (11.41) | 0.233 |
| 5 - 9.9 | 76,778 (55.08) | 71,404 (55.09) | 5,374 (55.01) | |
| 10 - 14.9 | 44,004 (31.57) | 40,854 (31.52) | 3,150 (32.24) | |
| ≥ 15 | 1,945 (1.40) | 1,814 (1.40) | 131 (1.34) | |
| Rain | 45,050 (32.32) | 41,989 (32.40) | 3,061 (31.33) | 0.030 |
| Precipitation (mm) | 0.903 | |||
| < 5 | 121,813 (87.39) | 113,294 (87.41) | 8,519 (87.20) | |
| 5 - 14.9 | 7,711 (5.53) | 7,159 (5.52) | 552 (5.65) | |
| 15 - 39.9 | 6,430 (4.61) | 5,979 (4.61) | 451 (4.62) | |
| ≥ 40 | 3,429 (2.46) | 3,181 (2.45) | 248 (2.54) | |
| Air pollutants | ||||
| CO (ppm) | 0.355 ± 0.147 | 0.354 ± 0.147 | 0.361 ± 0.152 | < 0.001 |
| O3 (ppm) | 0.028 ± 0.012 | 0.028 ± 0.012 | 0.028 ± 0.012 | 0.932 |
| NO2 (ppm) | 0.017 ± 0.008 | 0.017 ± 0.008 | 0.018± 0.008 | < 0.001 |
| SO2b (ppm) | 0.0037 ± 0.0017 | 0.0037 ± 0.0017 | 0.0038 ± 0.0019 | < 0.001 |
| PM10 (μg/m3) | 46.817 ± 25.193 | 46.769 ± 25.130 | 47.457 ± 26.001 | 0.009 |
Abbreviations: ED, emergency department; EMS, emergency medical services; SD, standard deviation; DTR, diurnal temperature range; CO, carbon monoxide; O3, ozone; NO2, nitric dioxide; SO2, sulfur dioxide; PM10, particulate matter less than 10 microns.
a Values are expressed as No. (%) or mean ± SD.
b These are indicated to the fourth decimal place to show the small difference in the concentration of SO2 between the two groups.
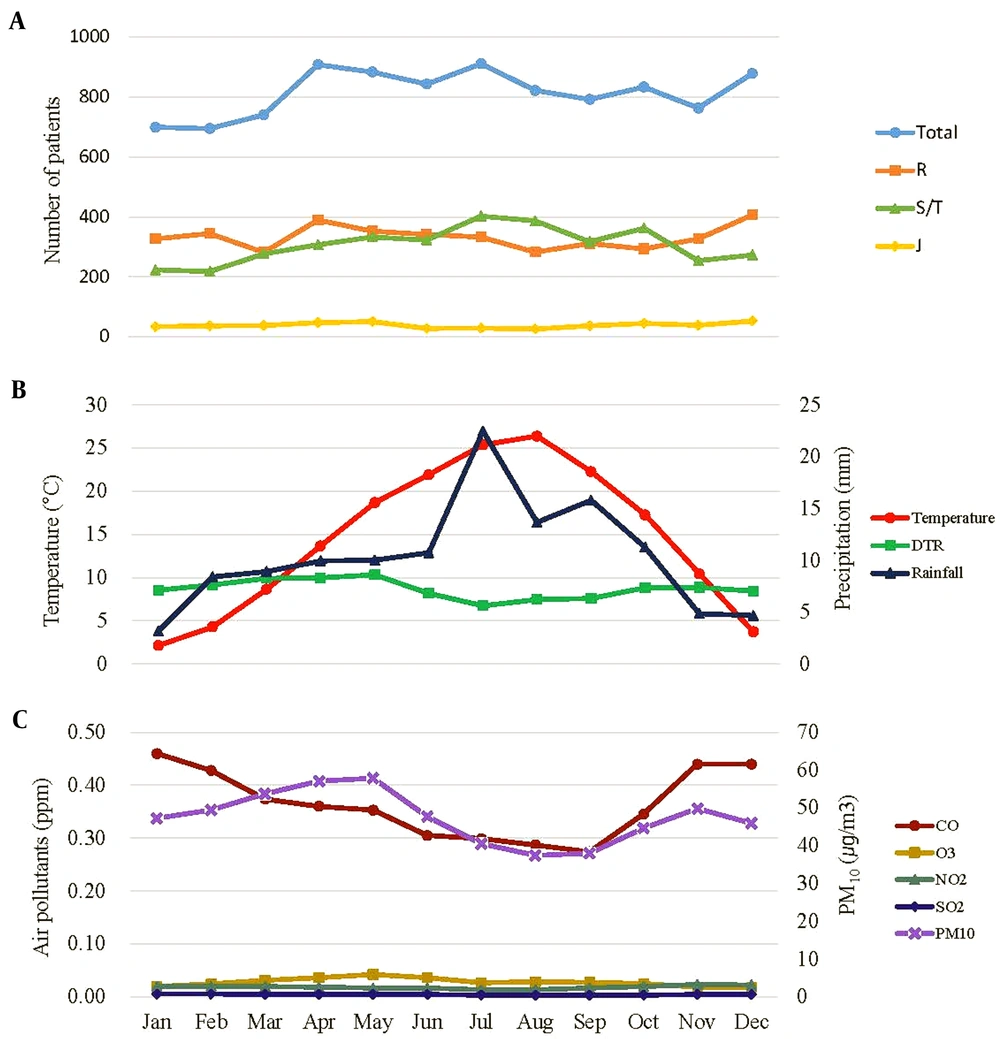
Figure 2 shows monthly patterns of the number of patients using the EMS and the monthly averages of meteorological factors and air pollutants. The number of patients in the S/T group increased from spring, peaked in July to August, and decreased through winter; the monthly average temperature and precipitation showed similar patterns. On the contrary, the number of patients in the J group was lowest from June to August, increased from late autumn, and remained high until spring. This pattern is consistent with the trend of the monthly averages of DTR and air pollutants except O3.
4.4. Influence of Clinical and Meteorological Factors on EMS Use
Table 4 shows the influence of clinical and meteorological factors on EMS use as obtained from logistic regression analysis. Male sex was a risk factor for EMS use in univariable analysis (OR: 1.21, 95% CI: 1.16 - 1.26; P < 0.001) but was no longer significant in multivariable analysis. Age had a positive correlation with EMS use (aOR: 1.12; 95% CI: 1.11 - 1.13; P < 0.001), while the KTAS and GCS scores had a negative correlation (aOR: 0.35, 0.73, respectively; 95% CI: 0.33 - 0.37, 0.70 - 0.77; P < 0.001, both). The rate of EMS use was significantly high in the S/T group compared with other disease groups (aOR: 3.47; 95% CI: 3.15 - 3.83; P < 0.001). The rate of EMS use was higher in summer than in winter (aOR: 1.36; 95% CI: 1.08 - 1.72; P < 0.001). Using precipitation less than 5 mm as a reference value, that greater than 40 mm increased the risk of EMS use (aOR: 1.31; 95% CI: 1.03 - 1.72; p = 0.048). Considering air pollutants, the probability of EMS use increased by 1.006 times for each 0.001-ppm increase in O3 (95% CI: 1.001 - 1.011; P < 0.014) and by 1.02 times for each 0.001-ppm increase in NO2 (95% CI: 1.001 - 1.03; P < 0.001), while it decreased by 0.91 times for each 0.001-ppm increase in SO2 (95% CI: 0.87 - 0.96; P < 0.001) and by 0.9973 times for each 1-µg/m3 increase in PM10 (95% CI: 0.9947 - 0.9998; P < 0.036). The whole population was divided into two groups of injury or disease based on ICD-10 code, which was revealed as the strongest risk factor for EMS use in multivariate analysis. A subgroup analysis was performed with the same variables to identify risk factors for EMS use in each group. Age, KTAS score, and GCS score had significant effects on EMS use in both groups. However, the meteorological factors had no effects on EMS use in the injury group, while they showed similar effects in the disease group to those in the whole population.
| Total (N = 139,383) | Injury (N = 28,259) | Disease (N = 111,124) | ||||||
|---|---|---|---|---|---|---|---|---|
| Crude | Adjusted | Adjusted | Adjusted | |||||
| OR (95% CI) | P-Value | aOR (95% CI) | P-Value | aOR (95% CI) | P-Value | aOR (95% CI) | P-Value | |
| Sex | < 0.001 | 0.397 | 0.382 | 0.676 | ||||
| Male | 1.21 (1.16 - 1.26) | 1.04 (0.95 - 1.12) | 1.07 (0.92 - 1.26) | 1.02 (0.93 - 1.12) | ||||
| Female | Reference | Reference | Reference | Reference | ||||
| Age | 1.090 (1.086 - 1.094) | < 0.001 | 1.12 (1.11 - 1.13) | < 0.001 | 1.11 (1.10 - 1.13) | < 0.001 | 1.12 (1.11 - 1.13) | < 0.001 |
| KTAS | 0.48 (0.46 - 0.51) | < 0.001 | 0.35 (0.33 - 0.37) | < 0.001 | 0.37 (0.33 - 0.42) | < 0.001 | 0.34 (0.31 - 0.36) | < 0.001 |
| GCS | 0.59 (0.57 - 0.61) | < 0.001 | 0.73 (0.70 - 0.77) | < 0.001 | 0.61 (0.48 - 0.77) | < 0.001 | 0.75 (0.71 - 0.79) | < 0.001 |
| Type of condition | < 0.001 | < 0.001 | - | - | ||||
| Injury | 2.58 (2.47 - 2.69) | 3.47 (3.15 - 3.83) | - | - | ||||
| Disease | Reference | Reference | - | - | - | - | ||
| Season | ||||||||
| Spring | 1.08 (1.02 - 1.15) | 0.008 | 1.14 (0.97 - 1.35) | 0.110 | 0.97 (0.72 - 1.32) | 0.866 | 1.20 (0.99 - 1.46) | 0.061 |
| Summer | 1.17 (1.07 - 1.24) | < 0.001 | 1.36 (1.08 - 1.72) | 0.009 | 1.04 (0.68 - 1.61) | 0.844 | 1.52 (1.16 - 2.01) | 0.003 |
| Autumn | 1.08 (1.01 - 1.14) | 0.017 | 1.09 (0.92 - 1.30) | 0.315 | 0.80 (0.58 - 1.12) | 0.190 | 1.24 (1.01 - 1.52) | 0.044 |
| Winter | Reference | Reference | Reference | Reference | ||||
| Mean temperature, DTR (°C) | 1.00 (1.00 - 1.01) | 0.994 (0.984 - 1.004) | 1.017 (0.998 - 1.035) | 0.98 (0.97 - 1.00) | ||||
| < 5 | Reference | 0.002 | Reference | 0.228 | Reference | 0.085 | Reference | 0.01 |
| 5 - 9.9 | 1.05 (0.98 - 1.12) | 0.160 | 1.10 (0.93 - 1.30) | 0.265 | 1.09 (0.79 - 1.49) | 0.616 | 1.11 (0.91 - 1.35) | 0.293 |
| 10 - 14.9 | 1.07 (1.00 - 1.15) | 0.046 | 1.15 (0.96 - 1.39) | 0.132 | 1.27 (0.90 - 1.80) | 0.178 | 1.12 (0.90 - 1.40) | 0.3 |
| ≥ 15 | 1.01 (0.83 - 1.21) | 0.946 | 1.04 (0.75 - 1.43) | 0.816 | 1.03 (0.57 - 1.85) | 0.923 | 1.08 (0.73 - 1.58) | 0.709 |
| Precipitation (mm) | ||||||||
| < 5 | Reference | Reference | Reference | Reference | ||||
| 5 - 14.9 | 1.03 (0.94 - 1.12) | 0.582 | 1.10 (0.90 - 1.34) | 0.375 | 1.01 (0.69 - 1.49) | 0.942 | 1.14 (0.90 - 1.44) | 0.282 |
| 15 - 39.9 | 1.00 (0.91 - 1.11) | 0.950 | 1.08 (0.87 - 1.34) | 0.474 | 1.03 (0.68 - 1.55) | 0.905 | 1.11 (0.86 - 1.43) | 0.438 |
| ≥ 40 | 1.04 (0.91 - 1.18) | 0.589 | 1.31 (1.03 - 1.72) | 0.048 | 0.77 (0.42 - 1.39) | 0.382 | 1.53 (1.13 - 2.07) | 0.006 |
| Air pollutants | ||||||||
| CO (0.1 ppm) | 1.03 (1.02 - 1.04) | < 0.001 | 1.01 (0.97 - 1.05) | 0.740 | 1.07 (0.99 - 1.15) | 0.071 | 0.98 (0.93 - 1.03) | 0.439 |
| O3 (0.001 ppm) | 1.000 (0.998 - 1.002) | 0.932 | 1.006 (1.001 - 1.011) | 0.014 | 0.996 (0.998 - 1.005) | 0.361 | 1.01 (1.00 - 1.02) | < 0.001 |
| NO2 (0.001 ppm) | 1.011 (1.008 - 1.013) | < 0.001 | 1.02 (1.01 - 1.03) | < 0.001 | 1.01 (1.00 - 1.03) | 0.109 | 1.03 (1.02 - 1.04) | < 0.001 |
| SO2 (0.001 ppm) | 1.02 (1.01 - 1.04) | < 0.001 | 0.91 (0.87 - 0.96) | < 0.001 | 0.94 (0.86 - 1.02) | 0.144 | 0.90 (0.85 - 0.95) | < 0.001 |
| PM10 (1 µg/m3) | 1.001 (1.000 - 1.002) | 0.008 | 0.9973 (0.9947 - 0.9998) | 0.036 | 1.000 (0.996 - 1.005) | 0.817 | 1.00 (0.99 - 1.00) | 0.01 |
Abbreviations: EMS, emergency medical services; KTAS, Korean triage and acuity scale; GCS, Glasgow coma scale; DTR, diurnal temperature range; CO, carbon monoxide; O3, ozone; NO2, nitric dioxide; SO2, sulfur dioxide; PM10, particulate matter less than 10 microns; OR, odds ratio; aOR, adjusted odds ratio.
5. Discussion
5.1. Clinical Characteristics of the EMS Group Distinct from Those of the Non-EMS Group
The proportion of male patients older than 10 years was significantly greater in the EMS group. The differences in the distributions of age and sex in the two groups might be due to the greater incidence of trauma among male adolescents than females and the more frequent suicide attempts among adolescents than younger children. Several previous studies have reported similar trends (18, 19). There was a higher proportion of children younger than four years in the non-EMS group, which might be associated with their light body weight and mild symptoms caused by respiratory infection. Attendance at a daycare center at a young age with an immature immune system can lead to frequent respiratory viral infections. The distribution of disease types for each age group produced such a trend (Appendix 1 in Supplementary File).
We also noted that the severity of disease evaluated by the KTAS and GCS was greater in the EMS group. The prognosis represented by CPR, hospitalization, ventilator use, and mortality rates also was worse in the EMS group. Corrado et al. classified pediatric trauma patients who visited the ED into three groups based on means of transportation: non-EMS, ground ambulance, and air ambulance (19). The percentages of patients in moderate to severe conditions were 8.3%, 13.3%, and 26.7% in each group, while the mortality rates and average length of hospitalization were 1.1%, 11.5%, and 12.3% and 2.8 days, 6.6 days, and 9.5 days, respectively. These results indicate that pediatric patients transported by EMS had more severe trauma and a poorer prognosis than those not using EMS, consistent with the results of our study.
There was a clear difference between the two groups regarding not only severity but also type of disease. In the EMS group, the percentage of trauma was significantly higher, and that of respiratory disease was lower than in the non-EMS group. This result is consistent with several previous studies on the relationship between type of disease and EMS use. Shah et al. conducted a study to analyze the factors associated with EMS use in pediatric patients (10). In their study, the distribution of patients by disease showed a significant difference between the EMS and non-EMS groups. In the EMS group, musculoskeletal, trauma, and poisonings occurred in 54% of the patients, and respiratory disorders in 8%. However, in the non-EMS group, these respective percentages changed to 35% and 19%, reducing the difference between them. In addition, Dayal et al. analyzed pediatric patients younger than 14 years who visited seven EDs in northern California in 2013 (20). In their research, trauma and respiratory disorders accounted for 44.7% and 8.4% of respective cases in the EMS group and 27.8% and 14.3% in the non-EMS group. In multivariable analysis, the risk factor having the greatest influence on EMS use was type of disease, with the rate of EMS use tending to be higher when patients visited the ED due to injury rather than disease. The frequency of trauma caused by vigorous physical activities or use of transportation such as bicycles or motorcycles is likely high in adolescents compared to young children. In addition, adolescents are more difficult to move quickly due to their heavier body weights than young children. Furthermore, injured patients should not be moved without stabilization to avoid additional damage. We speculate these reasons for the more frequent EMS use in pediatric patients with injury than with disease. When subgroup analysis was performed within the injury group, only age and disease severity significantly affected EMS use. This suggests that EMS use of pediatric patients who visit the ED due to injury is little affected by environmental factors but only injury severity.
5.2. Meteorological Factors Affecting EMS Use Among Pediatric Patients
In our study, the utilization rate of EMS among pediatric patients was greater in the summer than in the winter. Increased outdoor activities during warm seasons is a possible explanation for this trend. Park et al. investigated the incidence patterns of orthopedic fractures according to age and seasons among children and adolescents (21). In their study, fractures of the clavicle, distal humerus, and distal radius were significantly more frequent in summer than in winter. They attributed this to more frequent participation in outdoor activities in summer. In addition, respiratory infections due to viral agents, such as respiratory syncytial virus or influenza, are more prevalent in winter. Patients who visited the ED with respiratory viral infections were less likely to use EMS since they tended to have relatively mild symptoms.
Several previous studies have reported that temperature-related factors can affect ED visit rates (22, 23). According to Ramgopal et al., there is a positive correlation between temperature and hourly EMS use regardless of seasonality (24). As the weather becomes warmer, more people go outside and enjoy physical activities that can increase the risk of trauma. In addition, during heatwaves, when temperatures are extremely high, the number of patients visiting the ED with direct heat-related or renal diseases can increase (25, 26). According to our data, the mean temperature on the day of ED visit was slightly greater in the EMS group than in the non-EMS group; however, the difference was not significant in multivariable analysis.
In contrast to the mean daily temperature, DTR was identified as a significant risk factor for EMS use, except when it is greater than or equal to 15°C. The rate of EMS use tended to be greater on days with higher DTR values than on days with lower DTR values. It has been previously reported that DTR could affect mortality and morbidity associated with cardiovascular and respiratory diseases, especially in children and the elderly (27). This correlation was explained by a mechanism in which the rapid change of temperature increases cardiac output and heart rate, resulting in elevated cardiovascular workload and damage to the respiratory epithelium, leading to bronchospasm and airway inflammation (28, 29).
Recently, as interest in the environment has increased, many studies have been conducted on the effects of air pollutants on human health. In particular, the associations between air pollutants and respiratory diseases, such as asthma and respiratory infections, have drawn great attention (30-35). Zheng et al. reported that short-term exposure to air pollutants, including O3, CO, NO2, SO2, PM10, and PM2.5, accounts for increased risks of asthma-related ED visits and hospitalizations (30). In another recent study, elevated concentrations of SO2, NO2, PM10, and PM2.5 but not O3 were associated with increased emergency ambulance calls (35). However, when subgroup analysis was conducted on patients younger than 15 years, only PM2.5 showed statistically significant associations. In our study, concentrations of CO and NO2 were risk factors for EMS use. To the best of our knowledge, few previous studies have evaluated the impacts of air pollutants on patterns of EMS use among pediatric emergency patients.
5.3. Conclusions
Clinical factors of older age, injury rather than disease, and high disease severity are risk factors for EMS use in pediatric patients. We also found that meteorological factors of summer season, heavy rain, and concentrations of O3 and NO2 can increase the rate of EMS use among pediatric patients. Through an additional subgroup analysis, we showed that several meteorological factors can be risk factors for EMS use in pediatric patients who visited the ED due to disease rather than injury. Further research on factors affecting EMS use is needed to improve the quality of EMS.
5.4. Limitations
This study was designed as a retrospective review of patient records. A considerable amount of missing data for KTAS and GCS might have led to bias. Since this was a single-center study, our results might have limited generalizability to other regions or countries. We also did not consider lag effects to reflect the time taken for the meteorological factors to affect disease exacerbation or the incidence of trauma.