1. Introduction
Ventriculoperitoneal (V-P) shunt is a common surgery for patients with hydrocephalus. Complications vary after V-P shunt implantation. They include shunt obstruction, shunt infection, shunt disruption, etc. Migration of the V-P shunt to the chest wall frequently happens in children when they grow up, and the function of the shunt may be compromised. Migration of the shunt to the scrotum is a rare but reasonable complication due to the natural history of closure of the processus vaginalis (1). It may present with open status when a V-P shunt is implanted. Its clinical presentation may be silent if the shunt keeps patent. Delayed closure of processus vaginalis (PV) in infants makes this condition unique among numerous V-P shunt complications.
We describe the case of a 28-week-old boy who, following the implantation of a V-P shunt, presented scrotal migration of the peritoneal catheter, with the tip still kept in the peritoneal cavity with patent function. Unlike most cases presented in the literature, directly with obvious scrotum swelling as hydrocele, shunt malfunction causing hydrocephalus in progression, the clinical presentation with drowsiness, poor appetite, and even consciousness change. We present this case of a shunt with a patent drainage function but a catheter loop in the scrotum, causing hydrocele. The clinical management and therapeutic plan require careful assessment. We will discuss this rare complication and review the literature.
2. Case Presentation
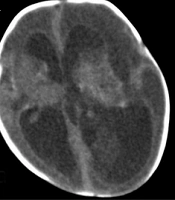
A 28-week-old boy presented pre-termed related complications (low body weight, spontaneous pulmonary hemorrhage, thrombocytopenia, and patent ductus arteriosus). He had a low heart rate of 60 beats/min on admission. Brain ultrasound revealed spontaneous intraventricular hemorrhage (grade IV in the left lateral ventricle and grade III in the right lateral ventricle) and hydrocephalus. Follow-up brain computed tomography indicated progression (Figure 1A and B). The patient underwent surgery via V-P shunt implantation. Postoperatively, his vital signs and general condition improved gradually (Figure 1C and D).
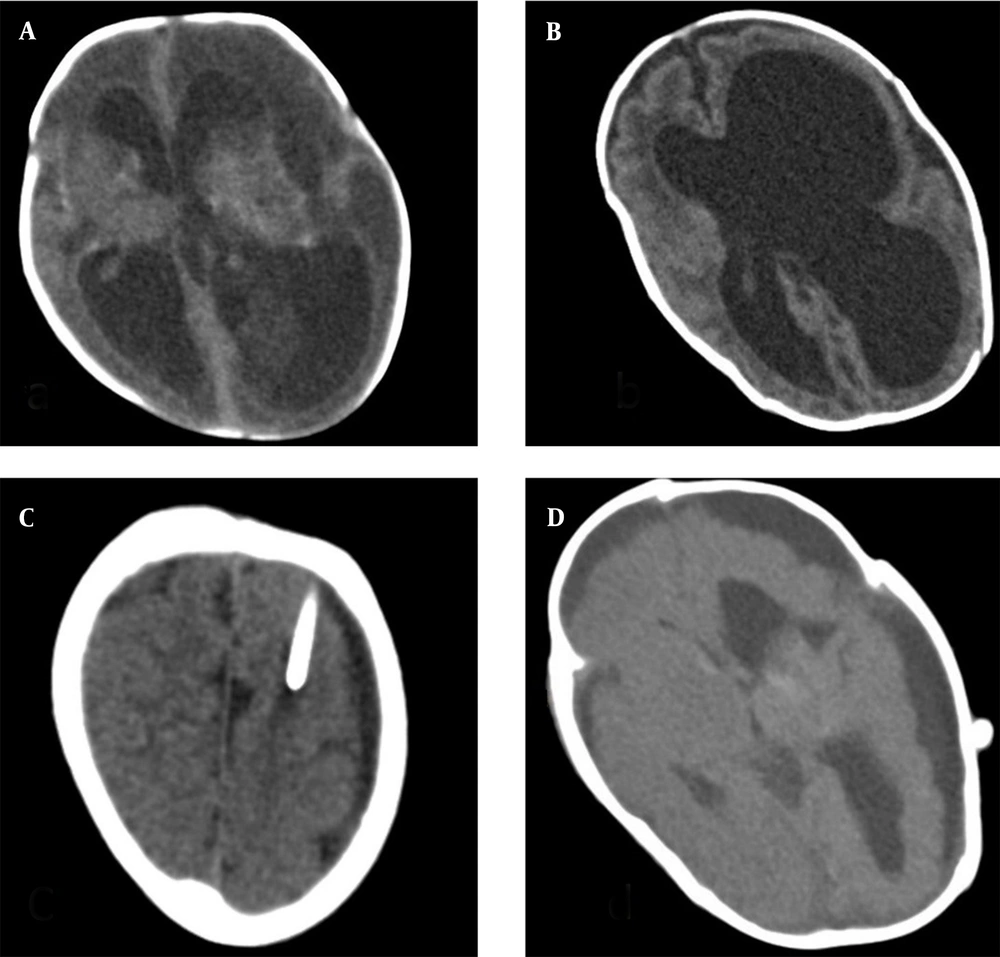
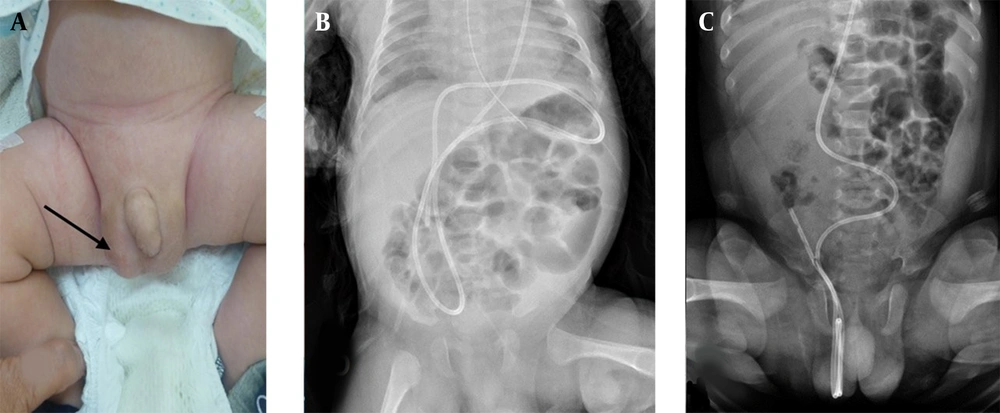
A palpable soft mass in the right scrotum was found one month after the operation, which enlarged and became more obvious while crying (Figure 2A). Scrotum hydrocele was suspected. The size did not subside at post-close monitoring. Post image survey, V-P shunt migration with right hydrocele was diagnosed (Figure 2). Surgical intervention of hydrocele repair and shunt repositioning was considered. After discussion with the pediatric surgeon and the family, we adopted a watch-and-wait approach in which outpatient follow-up would be continued until the patient was 1.5 years old, when we would decide whether to perform hydrocele repair and correct the drainage tube malposition or continue follow-up. Clinical presentation of the patient should be the key point during conservative treatment, especially symptoms connected with hydrocephalus. Drowsiness, sleepy, poor appetite and even consciousness change indicated hydrocephalus in progression.
Clinicians should be alert and arrange aggressive evaluation. Pediatric patients in this young age have relatively limited, imprecise expression. Symptoms with hydrocephalus mimic acute infections like upper airy way infection, urinary tract infection, fever period, etc. In the clinic, we should be more cautious in history taking and physical examination, neurological evaluation for pupil sizes, and sunset eyes. For image study, X-ray would be straightforward. However, sonogram would be beneficial and feasible to reduce radiation exposure for young-age patients. The patient was alert with good activity and was noted to be premature with delayed development during rehabilitation at the early intervention center.
3. Discussion
Ventriculoperitoneal shunt complications include shunt infection, colon and bladder perforation, peritoneal cerebrospinal fluid cyst formation, and small intestinal volvulus. Scrotal migration of the V-P shunt was a rare complication (1, 2). The literature reported that the incidence of V-P shunt migration to the scrotum in the pediatric group was 0.9% (3). It is usually accompanied by an inguinal hernia or hydrocele (1, 3). Kita et al. described a 5-year-old boy with scrotal migration of a V-P shunt catheter four months after implantation (4). Surgical obliteration of the patent PV was performed and allowed the abdominal catheter back into the abdominal cavity. Kita et al. analyzed 26 cases. The migration tended to occur within six months after implantation (mean, 3.8 months; median, 1.0 months). Involvement of the right-side scrotum was prevalent (23 of 26 cases), compatible with the distribution of inguinal hernia in children as right side predominant (4). A possible etiology that causes the migration to the scrotum is patent PV at the time of shunt insertion, with an incidence of about 63% in the first two months of life which then decreases until two years old (5).
In embryology, the closure of the left-side PV is earlier than that of the right side. Therefore, 60% of congenital inguinal hernias are found over the R't side. The incidence of inguinal hernia was higher in male patients than in the female group (male-to-female ratio of inguinal hernia 6:1) (6). The increased abdominal pressure after V-P shunt implantation and the inflow of cerebrospinal fluid may also cause prolonged patency of the PV. Therefore, the V-P shunt catheter may be more easily migrated into the scrotum in younger children with more potential for patent PV and a smaller peritoneal cavity (7).
Prompt surgical obliteration of the PV and catheter repositioning are recommended to prevent the incarceration of the catheter and V-P shunt malfunction, in which shunt revision is rarely required (8, 9). Intra-abdominal pseudocyst might be seen due to adhesion or infection after shunt tip repositioning, which required re-operation (10). However, gut peristalsis may help pull back the coiled shunt tube and resolve the hydrocele (11, 12). The inguinal hernia incidence may increase after VP shunt implantation (13). On the other hand, many studies show that communicating hydroceles may be resolved spontaneously with conservative medical treatment and regular follow-up in patients before 18 months old, and it is safe and effective (7, 14). The complete resolution rate for patients younger than 18 months was 62.7% (7) and 60.2% (14). In other words, more than half of those patients require no operation. Major complications, such as incarceration hernia, were not noted during the observation period.
In our case, the catheter circled in the scrotum with the tip remaining in the peritoneal cavity. Regular follow-up was the treatment of choice for this patient because the boy would grow up and the peritoneal cavity would enlarge. The shunt can migrate back to the peritoneal cavity from the scrotum, as the communicating hydroceles may recover in 1.5 years (7). The major complications for the watch-and-wait plan include hydrocephalus in progression. Complications related to the intra-abdominal catheter may include hydrocele in progression, hernia, or even hollow organ perforation, in extreme status. According to previous studies, the complication rate is low, and the conservative strategy is acceptable and safe for patients (7, 14). We suggest medical treatment with close monitoring and follow-up for the cases with patent shunt function and no severe adhesion to the scrotum. We emphasize the importance of observing clinical symptoms during the "watch and wait" period, especially for symptoms associated with hydrocephalus. Besides, adequate image study should be applied if clinical symptoms are ambiguous. An abdominal X-ray and sonogram could be applied to check the location of shunt tip, evaluate if the kinking catheter is still in the scrotum, and evaluate the hydrocele.
In the cases with the tip in the scrotum, shunt malfunction with hydrocephalus in progression, and remarkable hydrocele, we suggest arranging surgical intervention to solve the problem.
3.1. Conclusions
Ventriculoperitoneal shunt migration with hydrocele in young children is a rare complication after surgery. Regular follow-up to 1.5 years old is recommended for patients with the tip in the peritoneal cavity and patent shunt function. Surgical intervention is suggested for cases with tip in the scrotum, shunt kinking, remarkable hydrocele, or hydrocephalus progression. Although V-P shunt migration is uncommon, we should take care of it to find out and solve the problem.