1. Background
Inguinal hernia and hydrocele are common diseases in pediatric urology, with an incidence of about 1% - 4% in children (1). Congenital patent processus vaginalis (PPV) is the anatomical basis of inguinal hernia and hydrocele in children (2). A study (3) has pointed out that those who have PPV but do not present clinical symptoms are called occult hernias. Clinical symptoms may appear in the later stage, which requires re-surgery, bringing greater economic burden and surgical risk to patients (4). Therefore, it is particularly important to scientifically explore whether the children with unilateral inguinal hernia and unilateral hydrocele are complicated by contralateral patent processus vaginalis (CPPV). The imaging diagnosis of inguinal hernia and hydrocele is mainly based on ultrasound, but preoperative ultrasound examination often cannot detect CPPV due to its small lesion (5). With the continuous development and maturity of minimally invasive technology, laparoscopy is more and more widely used in pediatric urology. Compared with open surgery, laparoscopy has the advantages of simultaneous exploration of CPPV, reduction of postoperative pain, improvement of beauty, rapid recovery, and fewer complications in processus vaginalis ligation (6).
2. Objectives
We treated children with unilateral inguinal hernia and hydrocele using laparoscopic high ligation of the processus vaginalis, during which the factors related to CPPV were analyzed and individualized treatment was performed. In addition, the long-term effect on the children was followed up.
3. Methods
3.1. Patient Data
Inclusion criteria were: (1) children with unilateral inguinal hernia or unilateral hydrocele diagnosed by physical examination and imaging examination (7); (2) age ≤ 14 years; (3) no complicated heart and lung diseases or other surgical contraindications; (4) accepting the study and signing informed consent; (5) complete clinical data; and (6) ability to cooperate with the study, with high treatment compliance. This research was reviewed by the Medical Ethics Committee, and there was no ethical or moral hazard.
Exclusion criteria were: (1) contralateral inguinal hernia or hydrocele; (2) history of surgery for contralateral inguinal hernia or hydrocele; and (3) abnormal cardiopulmonary function, coagulation disorders, or impossible surgery for other reasons.
A total of 300 children with unilateral inguinal hernia or unilateral hydrocele treated in our hospital were selected and randomly divided into two groups, with 150 children in each group. In the study group, there were 145 males and five females aged 1.3 - 13.5 years (average age: 4.57 ± 1.26 years). The control group included 143 males and seven females, with an age of 1.5 - 12.0 years (average age: 4.72 ± 1.33 years). During surgery, CPPV was not detected in 120 children in the study group and 114 children in the control group. The children with CPPV in the control group were all treated with high ligation, while some children in the study group received high ligation according to intraoperative conditions. General data showed no significant differences between the two groups suggesting comparability (Table 1).
| Index | Study Group | Control Group | t/χ2 | P |
|---|---|---|---|---|
| Gender (male, %) | 145 | 143 | 0.35 | 0.56 |
| Age (y) | 4.57 ± 1.26 | 4.72 ± 1.33 | 0.97 | 0.32 |
| Classification | 1.20 | 0.27 | ||
| Hydrocele | 76 | 85 | ||
| Inguinal hernia | 74 | 65 | ||
| Lesion site | 0.22 | 0.64 | ||
| Left | 64 | 60 | ||
| Right | 86 | 90 | ||
| Contralateral patent processus vaginalis (No. (%)) | 58 (39) | 53 (35) | 0.47 | 0.50 |
Comparison of General Data Between the Two Groups (
3.2. Surgical Method
Under general anesthesia, children were in the supine position, with the affected side elevated. After routine disinfection and sheet laying, a 5-mm Trocar channel was made through the lower edge of the umbilicus to establish a pneumoperitoneum (the pressure was maintained at 8 - 10 mmHg). Then, instruments for abdominal surgery were inserted to explore the contents and adhesion of the processus vaginalis on the affected side. A small incision was made at the body surface projection of the internal ring on the affected side and pierced by a puncture needle (movable retractor) with a double No. 0 mousse thread. Subsequently, blunt separation was performed extraperitoneally on the inner side of the internal ring of the affected side, and the abdominal cavity was punctured crossing the vas deferens and spermatic vessels. One end of the thread was left in the abdominal cavity, and the needle was withdrawn to the extraperitoneal needle entry point through the original route. Afterward, the needle sneaked extraperitoneally along the outer side of the internal ring, reached the same puncture point, entered the abdominal cavity, hooked up the thread head left in the abdominal cavity and guided it out of the body, and then was withdrawn. Double knotting of the thread and high ligation of the processus vaginalis on the affected side was conducted. When knotting, the testis on the affected side was pulled to reduce the possibility of overlapping of the spermatic vessels or vas deferens on the affected side.
The method for exploring and determining CPPV is as follows. Under laparoscopy, the contralateral processus vaginalis was found open, and the bottom could not be seen. The edge of the internal ring was lifted with dissecting forceps, and it was found that there was a small foramen at the bottom extending to the inguinal canal, with obvious depression of the internal ring. In the control group, CPPV was found, and the same method was used for high ligation of the internal ring. Exploration of the abdominal cavity showed no obvious active bleeding or blood oozing, and then Trocar was withdrawn. The subcutaneous tissue of each incision was sutured with absorbable suture, and the skin edge was glued using biological glue and applied externally with auxiliary materials. Finally, the surgery ended. The study group was treated in the following cases: (1) the size of the scrotum changed after pneumoperitoneum compression, and the pneumoperitoneum pressure was limited to 8 - 10 KP; (2) laparoscopy could reach the bottom of the scrotum from the internal ring; (3) when squeezing the scrotum, there was gas or liquid discharged from the internal ring; and (4) laparoscopic exploration presented that CPPV was spongy (8). Without such conditions, treatment was not carried out.
3.3. Observation Indices
During surgery, the occurrence of CPPV was recorded in all children. Then, (1) the prevalence of CPPV between children with unilateral indirect inguinal hernia and unilateral hydrocele was compared; (2) the prevalence of CPPV between left and right PPV was compared (PPV = indirect inguinal hernia + hydrocele); (3) the prevalence of CPPV was compared among different ages; (4) in the follow-up comparison, both groups were followed up for one year after surgery; then, the incidence of transformation of CPPV to indirect inguinal hernia or hydrocele was compared. Significant differences between the two groups receiving different treatments were examined.
3.4. Statistical Analysis
All data were statistically analyzed using SPSS 20.0. The measurement data were expressed as (
4. Results
4.1. Prevalence of Contralateral Patent Processus Vaginalis Between Children with Unilateral Indirect Inguinal Hernia and Unilateral Hydrocele
The prevalence of CPPV was 23% in children with unilateral indirect inguinal hernia and 49% in children with unilateral hydrocele. The prevalence of CPPV in children with unilateral hydrocele was significantly higher than that in children with inguinal hernia (P = 0.00), as shown in Table 2.
| Group | n | Contralateral Patent Processus Vaginalis | Prevalence a |
|---|---|---|---|
| Indirect inguinal hernia | 139 | 32 | 23% |
| Hydrocele | 161 | 79 | 49% |
| χ2 | 14.67 | ||
| P | 0.00 |
Comparison in the Prevalence of Contralateral Patent Processus Vaginalis Between Children with Unilateral Indirect Inguinal Hernia and Unilateral Hydrocele (
4.2. Prevalence of Contralateral Patent Processus Vaginalis Between Left and Right Patent Processus Vaginalis
The prevalence of CPPV was 42% in children with left PPV and 33% in children with right PPV, without a statistically significant difference (P = 0.19), as seen in Table 3.
| Site of Onset | n | Contralateral Patent Processus Vaginalis | Prevalence b |
|---|---|---|---|
| Left | 124 | 53 | 42% |
| Right | 176 | 58 | 33% |
| χ2 | 1.73 | ||
| P | 0.19 |
Comparison in the Prevalence of Contralateral Patent Processus Vaginalis Between Left and Right Patent Processus Vaginalis (
4.3. Prevalence of Contralateral Patent Processus Vaginalis Among Different Ages
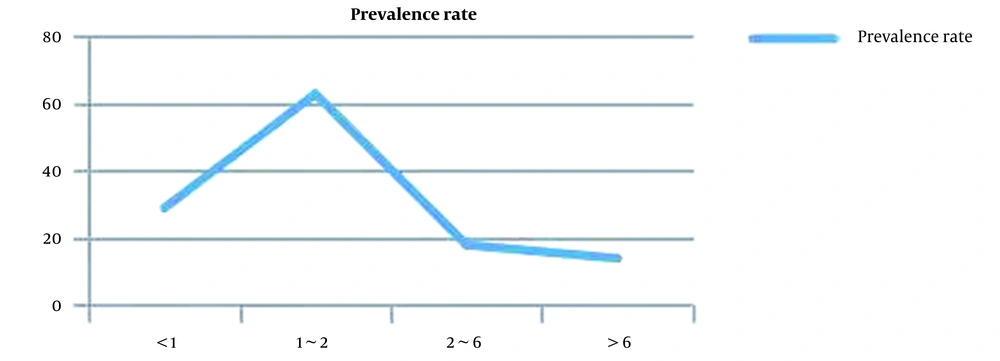
The prevalence of CPPV was 63% in children aged 1 - 2 years, which was significantly higher than that in other age groups (χ2 = 7.46, P = 0.01). The prevalence of CPPV was 14% in children aged > 6 years, which was significantly lower than that in other age groups (χ2 = 4.43, P = 0.04) (Table 4 and Figure 1).
Comparison in the Prevalence of Contralateral Patent Processus Vaginalis at Different Ages (
4.4. Follow-up of Different Treatments
A total of 58 children were included in the study group, among whom 11 met surgical conditions and received high ligation of the internal ring. All 53 CPPV children in the control group underwent high ligation of the internal ring. Postoperatively, both groups were followed up for one year, revealing that the recurrence rate of inguinal hernia or hydrocele was 9% (n = 5) in the study group and 1% (n = 1) in the control group, without a statistically significant difference (P = 0.25).
5. Discussion
Congenital PPV in children is a common disease in pediatric urology, which can lead to an indirect inguinal hernia and a spermatic cord or testicular hydrocele in children (9). Rothenberg and Barnett reported for the first time that unilateral inguinal hernia exploration detected CPPV, with an incidence of 20.0% to 39.7% (10). Surgical exploration and repair is the most common treatment method for inguinal hernia and hydrocele (11). With the continuous development of minimally invasive surgery, laparoscopy has been widely used in this field. Compared with open surgery, laparoscopic surgery has the advantages of a small incision, less trauma to the body, less pain, less bleeding, rapid postoperative recovery, fewer complications, and beautiful incision healing (12).
Because of the hidden existence of CPPV, most cannot be accurately evaluated by physical examination or imaging before surgery (13). There also are different opinions on whether CPPV detected during surgery should be treated simultaneously. Jo et al. (14) believe that early intervention in CPPV in the first surgery can reduce the incidence of surgical complications and avoid secondary surgery. However, Muensterer and Gianicolo (15) hold that with the increasingly mature diagnosis and treatment technology, it is not necessary to intervene in CPPV without obvious clinical symptoms, so as to reduce the invasive risk in the contralateral inguinal region of children.
Laparoscopy can enlarge the visual field and observe CPPV more intuitively. It has become an ideal tool for intraoperative diagnosis of CPPV with its high sensitivity and specificity (16). We intraoperatively explored the contralateral side of 300 children and found 111 cases of CPPV. After analysis, the prevalence of CPPV showed no significant difference between children with left and right PPV. Additionally, the prevalence of CPPV was 63% in children aged 1 - 2 years, which was significantly higher than that in other age groups. The prevalence of CPPV was 14% in children aged > 6 years, which was significantly lower than that in other age groups. The above data are consistent with the reported results (17). However, the prevalence of CPPV in children with unilateral hydrocele was higher than that in children with inguinal hernia, at about 49%. The reason may be that our center focuses on pediatric urology, so the number of children with hydrocele is larger than that of children with inguinal hernia.
There are generally two types of endoscopic morphology of CPPV: Cavernous type, which is readily detected, and fissure type, which is hidden and prone to miss the diagnosis. Usually, the chance of CPPV transforming into a hydrocele or inguinal hernia is small. The probability of recurrent hydrocele or inguinal hernia after routine repair and ligation for CPPV is 1/21 (18). Therefore, McClain et al. (19) believe that routine repair is not recommended for asymptomatic or hidden contralateral defects so as to potentially reduce the risk of contralateral injury caused by surgery. Zhu et al. (20) hold that when CPPV coexists, the scrotum changes after increasing intra-abdominal pressure, the internal ring can pass through the laparoscopic lens (5 mm), CPPV is spongy, and the internal ring has gas or liquid discharge when squeezing the scrotum, there is more likelihood of developing hydrocele or inguinal hernia in the future, which needs to be ligated and repaired during surgery. In our study, the above conditions were detected intraoperatively and then treated, and the recurrence rate was 9% in one-year follow-up postoperatively. In the control group, all detected CPPV cases were treated, and the recurrence rate was 1% in postoperative one-year follow-up. No statistically significant difference was found in the recurrence rate between the two groups (P = 0.25), as shown in Table 5. It is confirmed that the treatment of CPPV meeting the requirements and the treatment of all detected CPPV cases have a similar therapeutic effect.
| Group | n | Number of Ligations (n) | Number of Recurrent Cases | Recurrence Rate a |
|---|---|---|---|---|
| Study group | 58 | 11 | 5 | 9% |
| Control group | 53 | 53 | 1 | 1% |
| χ2 | 1.33 | |||
| P | 0.25 |
Follow-up Comparison Between Different Treatments (
5.1. Conclusions
In conclusion, the prevalence of CPPV decreases with age. Hydrocele combined with CPPV is more common. For younger children with hydrocele, it is very important to explore the contralateral side during surgery. Moreover, the transformation of CPPV to indirect inguinal hernia or hydrocele rarely occurs, and only eligible children can receive simultaneous treatment during surgery.
The limitations of this study lie in the small sample size and short follow-up. Because it takes some time for CPPV to transform into an indirect inguinal hernia or hydrocele, a longer follow-up is particularly important. In the future, we will continue to enlarge the sample size and prolong the follow-up duration so as to further evaluate the long-term efficacy of individualized treatment for CPPV detected during surgery.