1. Background
There are many challenges facing pediatric anesthesiologists, including frequent oral and pharyngeal secretions that increase as some anesthetic agents are prescribed (1). On the other hand, considering the predominant parasympathetic effect in children, the administration of anesthetic agents and even laryngoscopy may cause bradycardia in children (2).
One of the solutions that have been used for years to solve the above two problems is the atropine administration before induction of anesthesia, which, considering its anticholinergic and vagolytic effects, reduces secretions and prevents bradycardia in children during anesthetic induction (2, 3).
Delirium and agitation are commonly seen in children after waking up from anesthesia (3, 4), which are more likely to occur considering anticholinergic properties of atropine. The incidence of delirium in post-anesthesia care unit (PACU) increases restlessness, crying, as well as the risk of injury to the child, delayed hospital secretions, the need for more nursing care, and increased treatment costs (4, 5).
So far, various studies have been conducted to find methods of prevention and treatment of pediatric delirium in PACU, and it is recommended to use a single dose of propofol, midazolam, dexmedetomidine, or fentanyl before induction of anesthesia or to use propofol-based total intravenous anesthesia (TIVA) to prevent delirium in PACU (6-10).
2. Objectives
Since there has been no study on the relationship between atropine administration before induction of pediatric anesthesia and delirium incidence in PACU, the present study aimed to determine the effect of atropine administration on delirium incidence and complications in children aged 1 - 6 years old undergoing lower abdomen surgery compared with the control group.
3. Methods
This is a double-blind, randomized clinical trial that was performed in Pediatric Clinic of Imam Hossein Hospital, Isfahan, Iran, from 2020 to 2021. The target population included children aged 1 - 6 years undergoing lower abdominal surgery. The study was approved by and registered in the Ethics Committee of Isfahan University of Medical Sciences (IR.MUI.REC.1396.3.855) and also approved by the Iranian Registry of Clinical Trials (IRCT20200825048515N33). Inclusion criteria included age range of 1 - 6 years, candidates for lower abdominal surgery, American Society of Anesthesiologists (ASA) score I or II patients, and no psychiatric problems, including attention deficit hyperactivity disorder (ADHD), depression, and other behavioral disorders. Exclusion criteria comprised the prolongation of surgery or complication of surgery (such as bleeding).
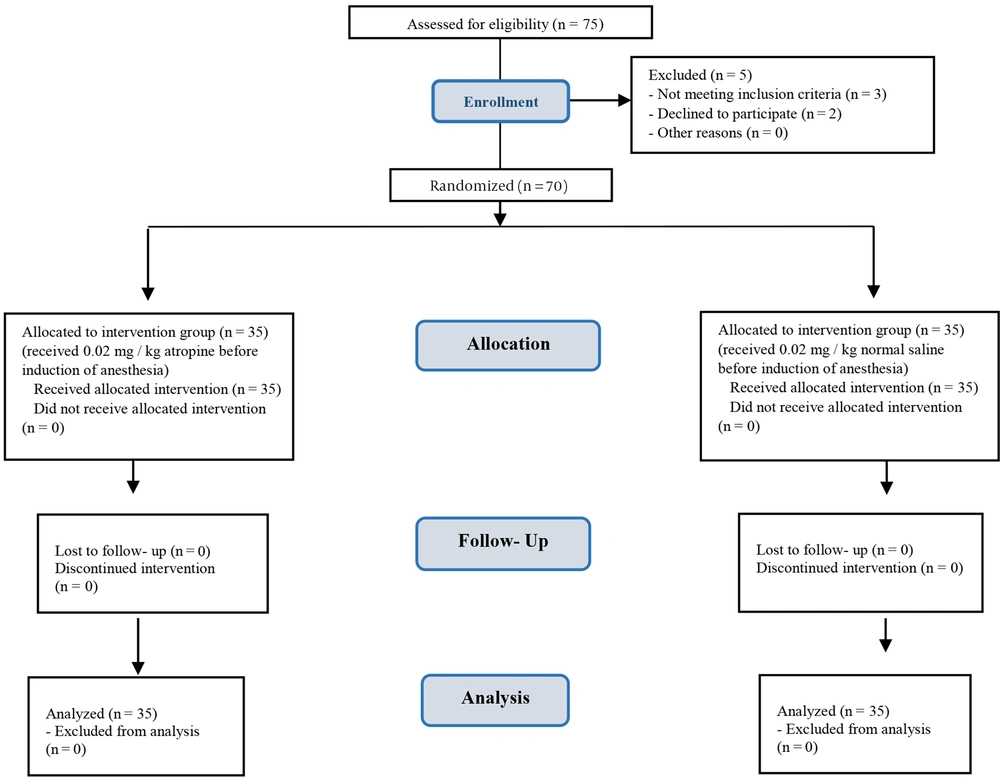
The sample size was estimated at 35 in each group using the sample size formula with 95% confidence level, test power 80%, the incidence of postoperative delirium (30%) (9), and the least significant difference between the two groups to be equal to 0.3. After obtaining written informed consent from the children’s parents, 70 eligible children were included using convenience sampling and divided into two groups using the random allocation software (Figure 1). At the beginning of the study, the children’s age and gender were recorded. Before induction of anesthesia, 0.02 mg/kg of atropine (after being diluted with a volume of 0.1 mg per cc) was administered intravenously in the first group (atropine group), and 0.02 mg/kg of normal saline (after being diluted with a volume of 0.1 mg per cc) was administered intravenously in the second group.
It is necessary to mention that the nurse who injected the drug, the researcher who registered the group allocation, and the patients were unaware of the type of medication and group allocation. Patients were separated from their parents after receiving 0.01 mg/kg midazolam +1 mg/kg ketamine as a premedication, and anesthetic induction was performed in the operating room using 2 mg/kg propofol, 2 mcg/kg fentanyl, and 0.5 mg/kg atracurium. Anesthesia was maintained with 50% O2 in air plus propofol (200 mcg/kg/min). Mean arterial blood pressure (MAP) and heart rate (HR) were measured and recorded before drug administration, before induction of anesthesia, 5 minutes after induction of anesthesia, and every 15 minutes during surgery. Salivary secretions during surgery and extubation were suctioned and recorded in cubic centimeter (cc). After the surgery and extubation, the patients were transferred to PACU, and the pain score was recorded according to face, legs, activity, cry, and consolability (FLACC) scale every 15 minutes, and in case of pain score ≥ 3, fentanyl (1 mcg/kg) was administrated.
Delirium score was recorded according to the pediatric anesthesia emergence delirium scale (PAED). A delirium score ≥ 10 was considered emergence delirium, and the patient was treated with 1 mg/kg propofol. The length of stay in PACU was recorded according to the modified Aldrete score tool in two groups. The frequency of complications such as laryngospasm, bronchospasm, SPO2 < 90%, nausea, and vomiting were evaluated and recorded in both groups.
3.1. Statistical Analysis
Finally, the data were entered into SPSS ver. 25. The data were shown with indicators such as means, standard deviation (SD), frequency, and percentage frequency. The independent samples t-test, repeated measures ANOVA, and chi-squared test were used to compare the mean of quantitative variables between two groups, the change of the mean of quantitative variables over time in each of the groups, and the frequency distribution of qualitative variables, respectively. P-value < 0.05 was considered significant.
4. Results
In this study, there were 27 and 29 boys in the atropine and control groups (77.1% vs. 82.9%), respectively, and the rest of the patients were girls (P = 0.551). The mean age of the atropine and control groups was 4.11 ± 1.13 and 4.2 ± 1.28 years, respectively (P = 0.770). There was no significant difference between the two groups in terms of mean age and sex frequency distribution (Table 1).
a Values are expressed as No. (%) or mean ± standard deviation (SD).
b The significance level of the independent samples t-test, comparing the mean of the variable between the two groups.
c The significance level of the chi-Square test, comparing the frequently distribution of the variables between the two groups.
The mean MAP did not differ between the two groups at any of the follow-up times (P-value > 0.05), but the atropine group had a higher intraoperative HR (P-value < 0.05). Intragroup comparison showed significant changes in intraoperative MAP and HR in the atropine group; however, there were significant changes only in intraoperative HR (P-value < 0.05), but not in the MAP of the control group (P-value > 0.05) (Table 2).
| Parameter | Atropine Group (n = 35) | Control Group (n = 35) | P b |
|---|---|---|---|
| MAP; mmHg | |||
| Upon entering the operating room | 65.58 ± 7.30 | 66.4 ± 7.51 | 0.600 |
| Before induction of anesthesia | 67.62 ± 7.41 | 66.4 ± 7.90 | 0.501 |
| 5 minutes after surgery | 67.55 ± 7.53 | 65.8 ± 7.36 | 0.360 |
| 15 minutes after surgery | 67.43 ± 7.49 | 65.7 ± 7.61 | 0.341 |
| 30 minutes after surgery | 67.80 ± 7.67 | 65.9 ± 7.22 | 0.282 |
| 45 minutes after surgery | 70.81 ± 6.44 | 62.00 ± 6.30 | 0.064 |
| Change mean | 5.30 ± 1.36 | -4.40 ± 3.16 | 0.533 |
| P c | < 0.001 | 0.11 | |
| HR; bpm | |||
| Upon entering the operating room | 119.40 ± 8.60 | 118.00 ± 9.28 | 0.513 |
| Before induction of anesthesia | 125.31 ± 10.11 | 121.4 ± 8.63 | 0.085 |
| 5 minutes after surgery | 139.32 ± 10.25 | 122.1 ± 9.36 | < 0.001 |
| 15 minutes after surgery | 140.27 ± 11.10 | 122.4 ± 9.16 | < 0.001 |
| 30 minutes after surgery | 140.88 ± 11.56 | 122.3 ± 9.55 | < 0.001 |
| 45 minutes after surgery | 143.30 ± 7.68 | 126 ± 12.41 | 0.024 |
| Change mean | 23.90 ± 4.16 | 8.00 ± 2.60 | < 0.001 |
| P c | < 0.001 | < 0.001 |
Abbreviations: MAP, mean arterial blood pressure; HR, heart rate.
a values are expressed as mean ± standard deviation (SD).
b Significance level of difference between the two groups in each time follow-up according to t-test.
c Significance level of the trend of intra-group changes according to repeated measures ANOVA.
In addition, the delirium severity was higher upon entering PACU and 15, 30 and 45 minutes after entering PACU in the atropine group; however, there was no significant difference between the two groups at any time follow-up (P-value > 0.05). Also, changes in delirium severity in the atropine group were higher than the control group during stay in the PACU; however, this difference was not statistically significant (P-value = 0.163). Intragroup investigation showed a significant reduction in delirium severity in both atropine and control groups in PACU (P-value = 0.042 and P-value < 0.001, respectively). On the other hand, there was no significant difference between the two groups in terms of the incidence of delirium cases requiring treatment (scores > 10) at any time period (P-value > 0.05) (Table 3).
| Delirium | Atropine Group (n = 35) | Control Group (n = 35) | P b |
|---|---|---|---|
| Severity of delirium | |||
| Upon entering PACU | 7.17 ± 3.19 | 5.45 ± 2.88 | 0.061 b |
| 15 minutes | 5.9 ± 2.56 | 5.66 ± 2.17 | 0.654 b |
| 30 minutes | 5.14 ± 1.83 | 5.03 ± 1.65 | 0.790 b |
| 45 minutes | 4.71 ± 1.72 | 4.34 ± 1.63 | 0.371 b |
| Change mean | 3 ± 0.86 | 1.11 ± 0.69 | 0.163 b |
| P d | 0.042 | < 0.001 | |
| Delirium incidence | |||
| Upon entering PACU | 6 (17.1) | 3 (8.6) | 0.281 c |
| 15 minutes | 5 (14.3) | 1 (2.9) | 0.090 c |
| 30 minutes | 1 (2.9) | 0 (0) | 0.998 c |
| 45 minutes | 1 (2.9) | 0 (0) | 0.998 c |
a Values are expressed as No. (%) or mean ± standard deviation (SD).
b Significance level of difference between the two groups in each time of follow-up according to t-test.
c Significance level of difference between the two groups in each time of follow-up according to chi-square.
d Significance level of intragroup changes according to repeated measures ANOVA.
The mean volume of suctioned secretions in the atropine and the control groups was 6.26 ± 2.47 and 14.57 ± 4.27 cc, respectively (P-value < 0.001). There was no significant difference between the two groups in terms of pain severity during their stay in PACU (P-value > 0.05). The mean length of stay in PACU in the atropine and control groups was 39.14 ± 9.03 and 40.86 ± 9.35 hours (P-value >0.05). In general, the incidence of postoperative complications in the atropine group, with 5.7%, was significantly lower than the control group, with 22.9% (P-value = 0.041). Among these complications, six patients had a decrease in SPO2 (two patients in the atropine group and four patients in the control group). Moreover, although there were two cases of vomiting and two cases of laryngospasm in the control group, there was no statistically significant difference between the two groups in terms of incidence of complications (P-value > 0.05). Propofol was given to eight patients in the atropine group and four patients in the control group (22.9% vs. 11.4%) (P-value > 0.05). There was no significant difference in the prescribed dose of fentanyl between the two groups (20.00 ± 4.08 vs. 18.75 ± 2.5 mg; P-value > 0.05). Also, the need for fentanyl was reported to be 31.4% in both groups. There was no significant difference in the prescribed dose of fentanyl between the two groups (15.38 ± 4.31 vs. 18.15 ± 3.78 mg; P-value > 0.05) (Table 4).
| Variable | Atropine Group (n = 35) | Control Group (n = 35) | P b |
|---|---|---|---|
| Volume of suctioned secretions; cc | 6.26 ± 2.47 | 14.57 ± 4.27 | < 0.001 |
| Postoperative pain intensity | |||
| Upon entering PACU | 2.06 ±.97 | 1.54 ± 1.22 | 0.068 |
| 15 minutes | 1.63 ± 0.69 | 1.77 ± 1.11 | 0.520 |
| 30 minutes | 1.40 ± 0.6 | 1.54 ± 0.7 | 0.361 |
| 45 minutes | 1.20 ± 0.42 | 1.45 ± 0.52 | 0.245 |
| Changes | 0.86 ± 0.36 | 0.09 ± 0.28 | 0.411 |
| P c | < 0.001 | 0.590 | |
| Incidence of postoperative complications | |||
| Total | 2 (5.7) | 8 (22.9) | 0.041 |
| Drop in SPO2 | 2 (5.7) | 4 (11.4) | 0.395 |
| Vomiting | 0 (0) | 2 (5.7) | 0.152 |
| Laryngospasm | 0 (0) | 2 (5.7) | 0.152 |
| Need for propofol | 8 (22.9) | 4 (11.4) | 0.211 |
| Propofol dose; mg | 20 ± 4.08 | 18.75 ± 2.5 | 0.601 |
| Need for fentanyl | 13 (37.1) | 13 (37.1) | 1.00 |
| Fentanyl dose; mg | 15.38 ± 4.31 | 18.15 ± 3.78 | 0.116 |
| Length of stay in PACU; min | 39.14 ± 9.03 | 40.86 ± 9.35 | 0.442 |
a Values are expressed as No. (%) or mean ± standard deviation (SD).
b Significance level of difference between the two groups in each time period according to t-test or chi-square.
c Significance level of intragroup changes according to repeated measures ANOVA.
5. Discussion
Pediatric anesthesiologists face many challenges, including the problems of frequent oral and pharyngeal secretions, which increase with the prescription of a number of anesthetic drugs (1). Anesthesia and even laryngoscopy may cause bradycardia in the child (2). One solution that has been used for years to solve the above two problems is the atropine administration before induction of anesthesia. It reduces secretions and prevents bradycardia in children during anesthetic induction considering its anticholinergic and vagolytic effects (2, 3). The risk of delirium is theoretically increased with atropine considering the anticholinergic effects; therefore, atropine administration is limited (4, 5).
The aim of the present study was to determine the effect of atropine administration on the incidence of delirium and other complications in children aged 1 - 6 years undergoing lower abdominal surgery compared with the control group. Examination of patients’ hemodynamic parameters showed that atropine recipients had a higher mean HR and overall, the trend of changes in HR was significantly different between the two groups. Considering that bradycardia is a serious complication in pediatric surgeries and the administration of atropine in this study increased children’s HR and caused mild tachycardia, it seems that its prescription will be beneficial due to the slight increase in HR and its acceptable tolerance by children, as well as its positive effects on respiratory complications and reduction of secretions after surgery.
Hudek reported that atropine administration in pediatric surgeries was associated with greater hemodynamic stability and reduced bradycardia (11). Prugh et al. also used atropine to reduce the incidence of agitation and delirium in pediatric surgery. They found that atropine administration was associated with a reduction in the incidence of hemodynamic disorders, especially bradycardia (12). Another study showed that the pre-emptive administration of atropine (dose of 0.02 - 0.5 mg/kg) could reduce the incidence of bradycardia during the intubation procedure (13). Therefore, according to the above findings, it seems that atropine administration is safe and beneficial in pediatric abdominal surgery.
The findings of the present study showed that preoperative atropine injection is associated with a reduction in oral and pharyngeal secretions during surgery and stay in PACU. Also, since high volume of secretions during surgery and stay in PACU can be associated with complications such as aspiration and coughing, atropine administration can reduce the volume of secretions. Wilmott et al. also showed that preoperative atropine injection in children was associated with a decrease in airway secretions (13). In fact, atropine can be classified as an anticholinergic agent (14). Anticholinergic agents reduce the effect of the parasympathetic nervous system and, in doing so, block the effects of the vagus nerve. Atropine allows for increased stimulation of the sinoatrial node by blocking vagal activity and conduction through the cardiac electrical system resulting in the contraction of the cardiac muscle. Because bradycardia is related to anesthesia, paralysis, and direct laryngoscopy is thought to be predominantly vagally mediated, atropine is a natural choice for counteracting these effects (13-17).
The findings of the present study showed no significant difference between the atropine and control groups in terms of the incidence of delirium during stay in PACU. On the other hand, as the length of stay in PACU increased, the delirium severity decreased in both groups, but there was no significant difference between the two groups in terms of changes in the severity of delirium. Hudek (11) and Prugh et al. (12) found that preoperative atropine administration was associated with decreased delirium severity and postoperative agitation. In the meantime, Asadi et al. showed that adding atropine to ketamine can significantly reduce excessive salivation without causing adverse effects on treatment success and length of stay in the emergency department (2).
The results of the current study showed that preoperative atropine administration is associated with a reduction in postoperative complications. Atropine is an anticholinergic drug that increases HR, reduces gastrointestinal, urinary, and biliary motility, and has anti-secretory effects by blocking acetylcholine receptors, and is therefore used in various cases such as bradycardia, antidote for organophosphate poisoning, and inhibition of salivation (13). It should be noted that evaluating the effect of atropine on respiratory complications and hemodynamic parameters in pediatric surgeries can be considered the strong point of this study; however, the small sample size and the non-evaluation of different doses of its administration can be some of the limitations of the present study. Therefore, it is suggested to conduct similar studies in the future addressing different doses of this drug and different types of pediatric surgeries so that the obtained results can be more reliably generalized to the target population.
5.1. Conclusions
The findings of the present study indicated that although the administration of atropine results in not only higher HR but also a slightly higher incidence of delirium in the atropine group compared to the control group, it may reduce the incidence of respiratory complications and the volume of secretions after surgery. In fact, in spite of a slight change in HR and a slight increase in the incidence of delirium, it can be stated that administration of atropine can be useful in the reduction of complications and secretions of volume after surgery. However, more studies are needed to make a more definitive conclusion in this regard.