1. Introduction
Renovascular hypertension (RVH), as a major cause of severe hypertension in children, mostly develops following impaired renal blood supply (1). Preliminary diagnostic work-up includes renal scintigraphy and intravenous pyelography (IVP) to evaluate the function of the relative kidney, and duplex ultrasonography is scheduled to assess the renal vessels status. The presence of numerous factors that impair kidney function can lead to misdiagnosis-related unnecessary nephrectomies, as they represent the compromised kidney as a non-functioning organ in such modalities (2).
First-line treatment of RVH is drug therapy, which is almost ineffective in the majority of cases, mostly leading to the need for further interventions. Angioplasty is the surgical treatment of choice in children with RVH; however, it is not always feasible, and its effectiveness is variable among patients (1, 3). Among various treatments available for the management of RVH, renal auto-transplantation (RAT) seems to be effective with acceptable results (4).
In this report, we showed that while angioplasty is failed or not feasible, RAT can be a safe promising alternative; subsequently, we advocated that absence of renal activity in routine diagnostic modalities may not always be equivalent to the presence of a non-functioning kidney that requires nephrectomy, and performing RAT can restore the function of the kidney in such cases.
2. Case Presentation
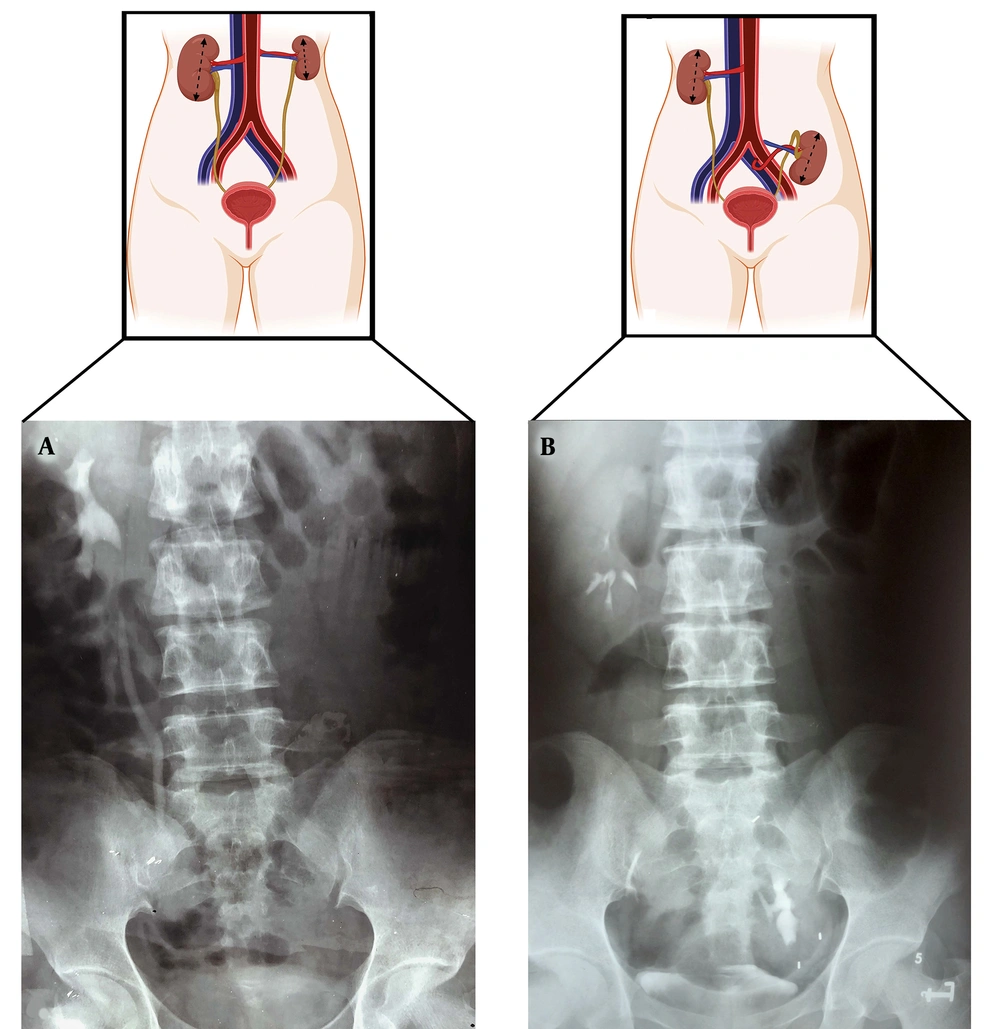
A 14-year-old girl was referred to our outpatient clinic with visual impairment, severe headache, and blood pressure of 220/150 mmHg. Before school, she was diagnosed with hypertension and migraine headaches. Although she was under medical treatment for almost seven years, her blood pressure was not controlled. Due to reduced urine output and previous history of lower urinary tract symptoms, she was referred to the urology department. On examination, blood pressure had decreased to 170/120 mmHg (controlled with anti-hypertensive agents). Abdominal thrill could be felt while renal bruit was also present on auscultation. Unfortunately, at that time, echocardiography was not available in our center, and cardiac assessment in our case was mostly based on the physical examination. Grade 4 hypertensive retinopathy was diagnosed based on her ophthalmology consultation. Chest X-ray showed left-sided cardiomegaly without cardiac or pulmonary failure. There was no flow in the left renal vein on 24-hour renal venography, and the right kidney was enlarged. The left kidney did not appear on IVP. Renal angiography depicted severe stenosis in the left renal artery ostium, while internal vasculature had remained normal and sufficient perfusion to the kidney was observed, pointing out the possibility of preserved renal function. The size of the left kidney was approximately 50% of the contralateral side, and renal scintigraphy depicted negligible function. Accordingly, RVH was diagnosed as a result of renal artery stenosis. During a cardiovascular consultation, the cardiologist refused to perform the per-cutaneous angioplasty, which was the only angioplasty option available at our center, due to non-availability of proper size vascular balloon dilator and possibility of damage to the vascular intima. In addition, renal artery bypass was strongly discouraged based on the surgeon opinion with the possible higher risk of thrombosis formation in the such hypertensive state. Although the involved kidney appeared non-functional, preserved vasculature and perfusion on angiography made us decide to restore its function instead of performing a nephrectomy. Therefore, RAT was performed. After clamping the renal artery, a left nephrectomy was performed, leaving the ureter intact. The kidney was thoroughly washed with cold ringer’s lactate solution and heparin, and was held in ice during the rest of the procedure. The left renal artery and vein were anastomosed end-to-side to the left main iliac artery and vein, respectively. Then the kidney was planted in the left iliac fossa. Post-operative recovery was uneventful, with acceptable perfusion and function of the autotransplanted kidney. Blood pressure was controlled well with oral anti-hypertensive agents. During her follow-up, she remained normotensive. Left kidney calyces are perfectly visualized in IVP in the left pelvis with excellent excretion (Figure 1). Renal function, in this case, was evaluated by comparing pre- to post-operation IVP. In spite of having a nuclear renal scan before the operation, patient refused to repeat the scan after surgery due to high expenses and repeated gamma radiation exposure regardless of our recommendations on enhanced comparison during follow-up. Lastly, the anti-hypertensive regimen was discontinued one year later. She was followed up for twenty years after surgery. Until her last visit, she had normal blood pressure following three normal pregnancies without any cardiac or visual sequelae.
Anatomical diagram of pre-operative versus post-operative status of the left kidney following renal auto-transplantation along with their relevant intravenous pyelography. A, The left kidney is reduced in size, while the right kidney is enlarged and is almost twice the size of the left kidney; B, The autotransplanted kidney is rehabilitated and increased in size to normal ranges, and the right kidney is reduced to normal ranges after six months.
3. Discussion
In this study, we presented a 14-year-old patient with hypertension who was irresponsive to oral therapy for several years. The presence of abdominal thrill and left renal bruit accompanied by malignant hypertension was suggestive of an existing renal artery stenosis and RVH. Although renal venography, IVP, and renal scintigraphy showed diminished left renal perfusion with an apparently non-functional kidney, there was preserved blood supply in the involved kidney on angiography. We decided to perform RAT based on evidence of remaining blood circulation and demonstrated the restoration of kidney function by IVP following the surgery, and blood pressure lowered to normal range.
Late diagnosis and management of RVH in children may lead to harmful consequences, including retinopathy, seizure, or growth retardation (5). Similar to what happened to our patient with multi-organ dysfunction regarding a seven-year diagnostic delay. Thus, A thorough physical examination is highly recommended when RVH is suspected, and as a clinically significant finding, auscultation of an abdominal bruit, as in the presented patient, may indicate renal artery stenosis (6).
Subsequently, imaging modalities help evaluate the kidney. Duplex ultrasonography is a non-invasive and safe method. Irrespective of the operator dependency on the findings, this modality may be unable to detect hemodynamic disturbance severity and is less applicable in obese patients (2, 7). Computed tomographic angiography and magnetic resonance angiography can be used to evaluate renal functional information; however, nuclear imaging provides more accurate parameters of renal function (8). Renal scintigraphy is a conventional modality used to estimate renal function, and its findings are highly decisive in determining the therapeutic approaches (1, 7). Different factors influence the renal uptake of the mapping agents, including the presence of severe renal artery stenosis or glomerulopathies and tubulopathies, mimicking a completely non-functioning kidney (2). Hence, Tse et al. advocated that the absence of radiotracer uptake should not be interpreted as a "non-functioning" kidney; otherwise, it may lead to redundant nephrectomies for the kidneys surviving with collateral blood supply, with the potential to be rehabilitated (2). Angiography has been utilized as the standard gold test in the detection of RVH. Even though this modality is time-consuming and invasive, that increases the probability of further dissection of the arteries, it provides a precise depiction of renal arteries and measure of the transluminal pressure for better decision-making when other modalities are indeterminate or risky (3, 9).
Drug therapy is the first-line treatment in patients with RVH. Combination of various anti-hypertension drugs is usually used; however, RVH is often resistant to drug therapy (1, 3). It has been demonstrated that severe complications that developed following the use of anti-hypertensive agents led to surgical intervention (2). In patients with failure in medical therapy, percutaneous angioplasty is less invasive among other options (10). Determining the most effective therapeutic approach for each patient depends on numerous factors, including age, etiology, and availability of facilities in the healthcare center (1, 3). It has been shown that in atherosclerotic-related RVH, revascularization has not been useful enough to decrease blood pressure or compensate the kidney damages. In addition, Zhu et al. have suggested that the effectiveness of drug therapy and angioplasty is similar in atherosclerotic patients and the treatment of choice is still the drug therapy (11). It is reported that children with congenital renal artery disorders or fibrotic lesions are more likely to be resistant to angioplasty and stenting owing to structural difficulties accompanied by poor results (12). Moreover, serious complications such as arterial spasm, dissection, and rupture are not unlikely and increase the rate of mortality and morbidity among the patients who undergo angioplasty procedures. Aneurysms are also a contraindication for angioplasty (13). Lastly, the success rate of angioplasty has been reported to be 28 - 94% (1), which has declined in longer follow-ups (13).
Although renal bypass surgery provides autologous vascular connection, it has various complications, particularly in pediatrics, including poor outcomes accompanied by the splenorenal bypass, probability of further expansion of saphenous vein graft aneurysms, and limited application of hypogastric artery due to its short length (5). In addition, patients’ circumstances and the preferences of the surgeon influence the feasibility of this procedure. Nephrectomy is the last option, as the kidney is not reconstructible. It is an invasive method with permanent loss of kidney function and greater risk of cardiovascular disease and hypertension in the future (14). When other strategies are not suitable, RAT can be performed to avoid nephrectomy. Duprey et al. have shown that ex vivo reconstruction of renal artery aneurysms can save even small branches while preventing unplanned nephrectomies (15).
Given the hypothesis that the apparently non-functional kidney distal to the arterial stenosis was the only organ protected from the devastating effects of severe hypertension attacks, and considering the existing collateral blood supply (2), the kidney has the potential of recovery following a blood supply restoration. Moreover, by considering the feasibility and complications of other revascularization methods, we performed RAT so that we could rehabilitate the kidney by restoring the blood flow to the kidney, and it was completely successful. Therefore, RAT is not only a technique to control the patients’ blood pressure, but also may have the potential to recover the function of the kidney, based on our experience and twenty years of follow-up.
There are limitations to this study. This study is a case presentation which may lead to bias. There is no appropriate comparison among different imaging modalities or management techniques. We were not able to assess the renal function before and after the surgical intervention efficiently. We recommend that when confronting a child with RVH and renal artery stenosis with an apparently non-functioning kidney on renal scintigraphy, IVP, or duplex ultrasound, angiography should be performed to confirm the lack of perfusion. It should be noted that there is still an opportunity to restore the kidney function, and RAT can be effective in this manner.