1. Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new strain of the Coronaviridae family. On December 31, 2019, the first infection case with his virus was identified in Wuhan, China, and then COVID-19 infection rapidly spread worldwide. On March 11, 2020, WHO declared COVID-19 as a public health emergency of international concern (1). Despite a milder form of the disease experienced by children, they can still be a major source of transmission, perhaps even more so than adults, due to varying degrees of signs and symptoms (2). This pandemic had a severe effect on patients with other respiratory conditions, as most of the medical services were occupied by COVID-19 patients. The pandemic has also had a dramatic impact on pulmonary diagnostic procedures, as many have been thought to have dangerous levels of infectious transmission as many have been thought to have high infectious transmission risk (3). Fear of the risk of transmitting COVID-19 has led many pulmonary function laboratories to minimize the number of tests due to fear of spreading the virus.
For assessing the airway in respiratory disease in the pediatric population, fiberoptic bronchoscopy (FB) is one of the most common diagnostic and therapeutic instruments. It has been widely used for identifying the cause of bronchiectasis, recurrent wheezing, and persistent stridor in children (4-6). According to a recent study, therapeutic bronchoscopies declined during the pandemic (7). Generally, the provision of essential and non-essential health services in the country has been severely affected by the epidemic. Still, no study has been reported on the epidemic's impact on pediatric fiberoptic bronchoscopy in Iran.
2. Objectives
We aimed to investigate how COVID-19 affected bronchoscopy procedures.
3. Methods
3.1. Patients
This retrospective cross-sectional study was carried out on pediatric patients who underwent fiberoptic bronchoscopy at Children's Medical Center (a tertiary pediatric hospital affiliated to Tehran University of Medical Sciences). Procedural analysis was done from 20 March 2019 to 20 February 2020 (the pre-pandemic period) and 20 March 2020 to 20 February 2021 (during the pandemic period). The pre and post COVID pandemic intervals are determined as before and after February 2020 in this study. Patients were divided into two groups based on undergoing bronchoscopy in each of these two-time intervals. Patients were randomly enrolled in both groups, and diagnostic and therapeutic categorized Indications for bronchoscopy were the same for the two groups. Patients with suspected COVID-19 disease did not undergo bronchoscopy to establish a diagnosis of COVID-19 (Except in cases of vital emergency). The prevalence of each indication for bronchoscopy was compared in both groups. The study included all patients who underwent bronchoscopy procedures during this time.
All the patients who underwent bronchoscopic procedures during this period were included in our study. Data regarding patients’ characteristics, bronchoscopy indications, and findings were extracted by reviewing the patient’s charts and bronchoscopy reports. The study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.CHMC.REC.1401.041).
Exclusion criteria were coagulopathy, hemodynamic instability, and severe hypoxemia (PaO2 < 55 mm Hg or SpO2 < 90% on room air). Absolute contraindications for bronchoscopy are absent informed consent, severe refractory hypoxia, inability to maintain adequate oxygenation during the procedure, or malfunctioning equipment. The common complications of flexible bronchoscopy are hypoxemia, tachycardia, bronchospasm, or bleeding. Since the information was extracted from the registry system of the bronchoscopy room, short-term follow-up of the patients is available until they regain consciousness. Still, long-term follow-up information of the patients was not available.
3.2. Statistical Analysis
Descriptive data analysis and chi-square test were used as statistical methods. Mean, standard deviation, median, frequency, and ratio values were used in the descriptive statistics. The distribution of variables was assessed with the Kolmogorov-Smirnov test. P values less than 0.05 were considered statically significant. Data were analyzed using SPSS Statistics 26.0.
4. Results
Our results from the data registry showed that from 20 March 2019 to 20 February 2020 (group 1), 290 patients vs. 241 patients from 20 March 2020 to 20 February 2021 (group 2) were admitted to the operation room at least once for bronchoscopy procedures. 131 (45.2%) females and 159 (54.8%) males were in group 1, and 150 (62.5%) females and 90 (37.5%) males were in group 2 (the demographic characteristics of the patients are demonstrated in Table 1. There were several indications for pediatric bronchoscopy. Table 2 shows the different indications for pediatric bronchoscopy and their frequency before and during the COVID pandemic. Indications whose frequency was above ten percent are listed in the table. Overall the most common indications in group 1 were suspicions of a foreign body in the first period vs. in group 2, persistent stridor followed closely by suspicions of a foreign body. There is a significant difference between the indications for Exploration of the airway in the two groups. Six patients (2%) in the first group and thirteen (5.4%) underwent bronchoscopy due to persistent wheezing in the second group. The difference between the two groups was significant (P-value = 0.039). Hemoptysis was indicated for bronchoscopy in nine (3.1%) patients and four (1.7%) in the first and second groups, respectively. The difference between the two groups was not significant (P-value = 0.288). In each group, difficult intubation included two cases (P-value = 0.849). With suspicion of tracheoesophaseal fistula, eleven patients (3.8%) underwent bronchoscopy, and this number was nine patients (3.7%) in the second group (P-value = 0.979). Dysphonia or aphonia was another indication for bronchoscopy in patients with other underlying diseases. Three and two patients were in groups one and two, respectively (P-value = 0.812). Two patients in the first group (0.7%) and seven patients in the second group (2.9%) underwent bronchoscopy to check the tracheostomy tube (P-value = 0.048). 12% (29 patients) in the second group and 2% (six patients) in the first group underwent bronchoscopy for other reasons such as Removal of airway secretions or mucus plugs, or Administration of drugs or investigation injuries caused by burns with ingestion of caustic substances or suspected ILD (Interstitial Lung Disease) or PAP (Pulmonary Alveolar Proteionosis) (P-value = 0.000).
Three patients from among the patients who underwent bronchoscopy during the period of COVID-19 had a positive test for COVID-19. All three patients were subjected to bronchoscopy with the suspicion of the presence of a foreign body, and foreign bodies were seen in all three cases.
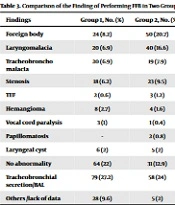
Table 3 shows the findings of bronchoscopy before and during the COVID pandemic. Although the findings of foreign body aspiration in bronchoscopy were more frequent in group 2, this difference was not significant in the two groups (P = 0.055). The number of cases without abnormality in group 2 was significantly less than in group 1 (P = 0.006). Also, the prevalence of Laryngomalacia was significantly higher in group 2 (P = 0.000).
| Group 1 | Group 2 | P-Value | |
|---|---|---|---|
| Age, y | 0.075 | ||
| Under 1 | 102 (35.9) | 86 (36) | |
| 1 - 5 | 131 (46.1) | 97 (40.6) | |
| 6 - 10 | 31 (11) | 39 (16.3) | |
| 10 - 15 | 21 (6.3) | 15 (6.3) | |
| Older than 15 | 2 (0.7) | 2 (0.8) | |
| Sex | 0.677 | ||
| Boys | 159 (54.8) | 150 (62.5) | |
| Girls | 131 (45.2) | 90 (37.5) |
| Indication for Bronchoscopy | Group 1, No. (%) | Group 2, No. (%) | P-Value |
|---|---|---|---|
| Persistent stridor | 73 (25.1) | 62 (26.7) | 0.862 |
| Suspicion of foreign body | 84 (28.9) | 47 (19.5) | 0.013 |
| Chronic cough | 31 (10.6) | 10 (4.1) | 0.005 |
| Persistent pneumonia & obtaining BAL | 30 (10.3) | 18 (7.5) | 0.256 |
| Radiologic abnormality including: persistent atelectasis / consolidation / localized pulmonary hyperlucency | 33 (11.3) | 38 (15.8) | 0.134 |
| Findings | Group 1, No. (%) | Group 2, No. (%) | P-Value |
|---|---|---|---|
| Foreign body | 24 (8.2) | 50 (20.7) | 0.055 |
| Laryngomalacia | 20 (6.9) | 40 (16.6) | 0.000 |
| Tracheobroncho malacia | 20 (6.9) | 19 (7.9) | 0.655 |
| Stenosis | 18 (6.2) | 23 (9.5) | 0.148 |
| TEF | 2 (0.6) | 3 (1.2) | 0.507 |
| Hemangioma | 8 (2.7) | 4 (1.6) | 0.401 |
| Vocal cord paralysis | 3 (1) | 1 (0.4) | 0.414 |
| Papillomatosis | - | 2 (0.8) | 0.120 |
| Laryngeal cyst | 6 (2) | 5 (2) | 0.991 |
| No abnormality | 64 (22) | 31 (12.9) | 0.006 |
| Tracheobronchial secretion/BAL | 79 (27.2) | 58 (24) | 0.421 |
| Others /lack of data | 28 (9.6) | 5 (2) | 0.000 |
There were no deaths or severe complications (such as pneumothorax and massive bleeding or respiratory failure) in any of the two groups. There was no hypoxia that led to the complete termination of the procedure. But in the first group, 6 cases required a short-term pause of the procedure to improve hypoxia, and in the second group, there were 5 cases. This difference between the two groups was not significant. Other minor and transient complications, such as transient hypoxia, transient tachycardia, or bradycardia, were ignored.
5. Discussion
Our results confirmed our prior hypothesis stating a decrease in pediatric bronchoscopy after the COVID-19 pandemic. Various reasons could explain this matter. Most diagnostic and therapeutic procedures have a high risk of aerosol transmission and are associated with an increased risk of infection transmission to the patient and healthcare workers (HCWs), and due to the fear of being infected with COVID 19, these procedures are much less performed. Furthermore, in the early months of this epidemic, this potential risk made many pulmonary function laboratories either shut down or reduce testing to minimal in fear of causing viral spread.
Also, the COVID-19 pandemic has had a profound effect on the National Health Service (NHS), causing a reorganization from a comprehensive healthcare service to one predominantly focused on treating patients with COVID-19. The results of a study by Call et al. showed that pulmonary diagnostic procedures were significantly reduced during COVID 19 epidemic, but bronchoscopy showed the least reduction compared to other procedures (8). Furthermore, according to a study published recently by Matta et al., the number of therapeutic bronchoscopies declined during this pandemic (7). The results of this study are in line with our study, except that these studies were performed in the adult age group.
Despite the decrease in the number of bronchoscopies during the epidemic, we noted an apparent increase in the number of children presenting with foreign body aspiration compared to the pre-pandemic period. However, this increase was not significant. Foreign body aspiration (FBA) is one of the common pediatric emergencies, and it is an extremely mortal accident. Despite the COVID-19 pandemic, airway emergencies continue to occur in children, and pediatric surgeons often have to act without waiting for COVID-19 test results in these emergencies (9, 10). Pizzol et al. reported a dramatic increase in battery ingestions in children, a potentially fatal event, during the COVID-19 pandemic lockdown (11). These data indicate that children's habits may have changed during the pandemic. Children were spending an abnormally long amount of time at home, which could have resulted in their increasing use of electronic devices, a need for more batteries, and eventually, an increase in accidents (11). The presence of parents at home has caused more care for children, as a result, the suspicion of foreign body aspiration has decreased with the direct supervision of families.
Pediatric bronchoscopies should be divided into three categories: urgent, semi-urgent, and elective during the pandemic. Endoscopies of the airways generate aerosol and are therefore considered high-risk procedures for transmitting pathogens to healthcare workers. Therefore, all patients should be screened for SARS-CoV-2 infection. However, Urgent bronchoscopy must be performed as soon as possible and, in any case, within 24 h after emergency department admission without results of SARS-CoV-2 testing available. It has been recommended that elective bronchoscopies be delayed unless the patient has completely recovered and has been declared free of infection with negative PCR testing (12). Various groups have advocated this policy to prevent the potential transmission of SARS-CoV-2 among patients and healthcare workers (12-15).
The registration of patients' information by the medical system during the COVID period has improved compared to the pre-COVID period, which may be related to two factors: 1. Reducing the number of bronchoscopies and reducing workload 2. Increasing the sensitivity of the medical system in recording information.
This study is limited by not evaluating clinical outcomes affected by this reduced testing, an important area for future study. In addition, our study was single-centered. The strength of our study is its novelty. To the best of our knowledge, this is the first study to assess the effect of COVID-19 on pediatric flexible fiberoptic bronchoscopy compared with pre-COVID-19 years.
5.1. Conclusions
The COVID pandemic has had a profound impact on bronchoscopy activity in children, which is evidenced by a considerable reduction in most procedures. However, there was no change in the immediate indications for bronchoscopy, and this pandemic had the most significant impact on elective bronchoscopy. Efforts should be made to safely return to pre-COVID situations so that the patients in need of essential health services can be evaluated and treated to suit their health needs.