1. Background
To ensure regularity of sleep cycles, external cues, as well as the internal body clock, need to be in harmony (1). Among the external environmental cues, the most potent regulator of sleep for adolescents is their school life, particularly the start times of their schools (2, 3). The school’s starting time has a strong effect not only on teens’ sleep regularity, but also on their overall sleep duration. This is because going to school affects sleep offset and may increases sunlight exposure and the possibility of activity on the way to school (4, 5). Accordingly, several studies and campaigns to delay schools’ starting times have been conducted worldwide (6). The regularity of these external cues particularly affects the variability of the sleep cycle; an extreme example is individuals undertaking shift work or changes to daylight savings time (7, 8). School life is considered the most potent sleep regulator for teens, irrespective of the mode of classes (9, 10).
COVID-19 has forcefully changed many aspects of lives worldwide, especially with students missing school days and experiencing online classes. Regardless of whether online classes are delivered synchronously or asynchronously, their overall influence differs in comparison to traditional face-to-face classes, thereby influencing students’ lifestyles and especially their sleep patterns (11). Online classes and social distancing were associated with decreased quality of sleep and amount of activity among teens in the early phase of the pandemic (12, 13). This might have been caused by an unstable social environment (14), abrupt changes in school schedules, or depressive mood; all of these factors were applicable worldwide. Social jetlag decreased during social distancing with reported lower nocturnal sleep efficiency (15).
2. Objectives
Compared to the early phase of the pandemic, after adjusting to social distancing, teens’ sleep patterns may have adapted, become fixed, and changed. This study, therefore, analyzed students’ sleep patterns under prolonged social distancing, and surveyed possible sleep debt as a result of changes in their sleep patterns.
3. Methods
3.1. Study Design
This was a cohort study using stratified data sampled from the whole of South Korea using complex sample methods (16). In the Korea Youth Risk Behavior Web-based Survey (KYRBS), several items were selected from 2018 to 2020, such as sleep schedule for the last 7 days, mood since the past 12 months, and sleep satisfaction, along with demographical characteristics, such as school year and gender. Data from 2018 to 2019 were used as a baseline, because the first case of COVID-19 and the subsequent transition to online classrooms occurred in January and February 2020, respectively (Appendix 1).
3.2. Data Source: The Korea Youth Risk Behavior Web-based Survey
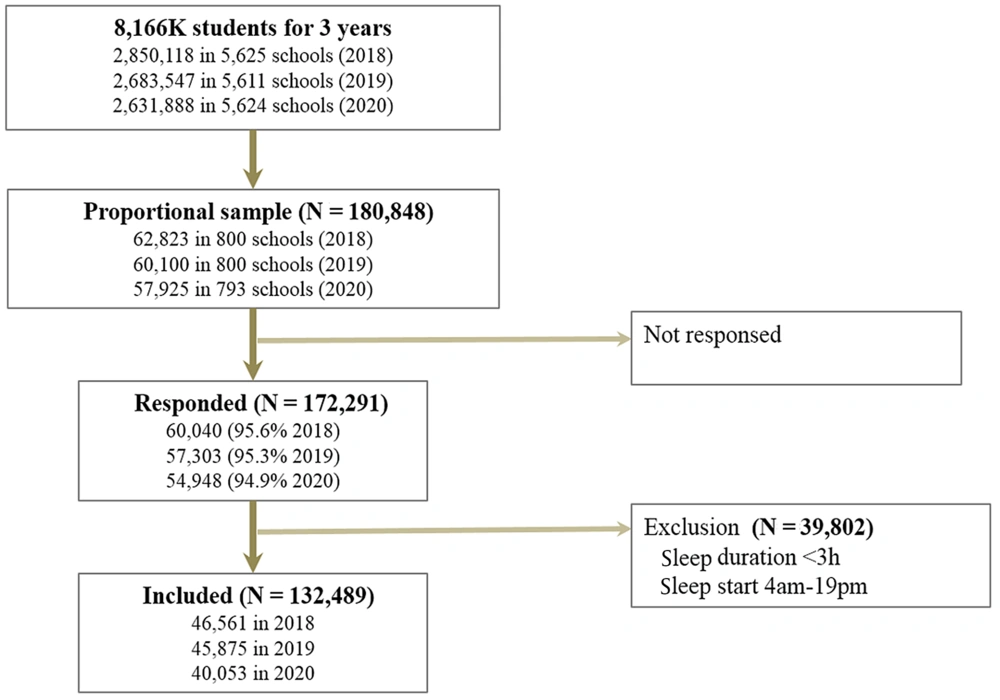
The Korea Youth Risk Behavior Web-based Survey (KYRBS) is a regular online survey conducted annually since 2005 to assess health and risk behaviors in adolescents, by the Centers for Disease Control and Prevention in South Korea with Statistics Korea. The survey for this study was performed in middle schools (1st to 3rd school year) and high schools (4th to 6th), which were proportionally selected according to school type and location. Data were obtained from nearly 800 sampled schools, representing 2.63 to 2.85 million students per year in approximately 5,600 schools (Figure 1). In the selected schools, all students provided their informed consent for participating in the survey. The data of those who agreed to take part in the survey were anonymized and used with their permission (17). The survey period in this study was June 1 to June 30, 2018 and 2019, and August 1 to November 30, 2020.
From August to November 2020, which was also the duration of our survey, social distancing was imposed to flatten the curve due to the worsening COVID-19 outbreak. Schools had the autonomy to decide on whether to conduct online classes. However, most school administrators decided the type of classes according to the stages of social distancing. Mostly, a third to two thirds of the students attended face-to-face classes and the others joined online classes by turn. These online classes were synchronous — live classes used cameras and ran at the same time as in-person school hours (students went to school at 9 am and returned home between 2 pm to 6 pm in 2018 - 2019).
3.3. Survey Item
Out of the 93 items in 15 areas, the selected items included questions about sleep time during weekdays and weekends, subjective sleep satisfaction, mood for the past 12 months, and subjective health. Moreover, data regarding participants’ height, weight, gender, school grade, and the year of survey were also used.
Subjective health perception was questioned through the item: How do you feel about your health in general? Responses were measured on 5 graded scales; classified as “very healthy,” “healthy,” and “ordinary” for “healthy” and “not healthy” and “very unhealthy” for “unhealthy.” Stress perception was determined as follows: “How much do you feel stressed?” and responses were measured on 5 graded scales; “very much” and “a lot” for “stressed” and “a little,” “do not feel stressed,” and “never stressed” for “not stressed.” The mood of the participants was assessed through the following question: “During the last 12 months, have you ever felt sadness or despair enough to disrupt your daily life for two weeks?” The answer was in terms of “yes” or “no.” Suicidal thoughts were identified through the item: “Have you had any serious suicidal thoughts in the past 12 months?” The answer was either “none in the last 12 months (no)” or “sometimes in the last 12 months (yes).”
3.4. Survey for Sleep
For subjective sleep sufficiency, the question asked was as follows: Do you think that the duration you have slept in the past 7 days is sufficient to not feel sleepy? Answers such as “more than enough,” “enough,” and “ordinary,” were classified as enough. Other responses such as “almost enough” and “not enough at all” were classified as “insufficient,” also known as sleep deprived.
Sleep time was assessed through the question: During the last 7 days, what time did you usually go to bed and wake up? The responses were meant to be for weekdays (Monday to Friday) and weekends (Saturday to Sunday), in hours and minutes (am/pm). Sleep duration during weekdays and weekends was computed with bedtime and wake time. Sleep inconsistencies and sleep durations for a week were also computed as follows: Sleep inconsistency was calculated as the difference between sleep duration during the weekend and weekdays; sleep duration for a week was computed as (sleep duration per weekday * 5) + (sleep duration per weekend day * 2). A positive value obtained for sleep inconsistency meant that the sleep duration on weekends was longer than that for weekdays.
3.5. Exclusion Criteria
Data were excluded if the responses for sleeping time and duration were likely to be an error. In other words, students were excluded if the reported bedtime during weekdays was between 4:00 a.m. and 7:00 p.m. or if the total sleep time per night during weekdays was less than 3 h. Considering that weekend sleep durations would vary a little more, data were excluded if the falling asleep time fell between 9:00 a.m. and 7:00 p.m., and if the sleep duration was less than 3 h per night.
3.6. Statistical Analysis
The KYRBS was a stratified survey. The data were analyzed using the complex sampling method proposed by the Korea Centers for Disease Control and Prevention (KCDC), with weight and clustering by restriction, age, sex, and type of schools. Comparing variables, the general linear model and regression analyses were conducted using complex samples design, which used unequal weight by stratification and clustering of the sample (16). Results represented as a raw count (proportion) or estimated means with 95% confidence intervals (CIs). Two-tailed tests with P-values < 0.05 were considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Sciences 25 for Windows (SPSS, IBM, Armonk, NY, USA).
3.7. Ethics
The institutional review board approved of the study protocol (IRB CHAMC 2021-06-086).
4. Results
4.1. Sample Characteristics
The overall survey population included approximately 58–63 thousand students, and the participation rates were 95.6% in 2018, 95.3% in 2019, and 94.9% in 2020. After exclusion of responses involving extraordinary sleep times or durations, 132,489 students were included for the three years. These students represented a population of 6,298,972 students, which consisted of 35.2% in 2018, 34.3% in 2019, and 30.5% in 2020. The weighted proportion of students in the first school year (1st year of middle school) was 16.1%, and that of students in the second school year was 15.3%. The third school year comprised 15.6%; the fourth school year (1st year of high school), 16.6%; the fifth school year, 17.2%; and the sixth school year, 19.1% (Table 1). Weighted proportions of men were 51.9%. The participants’ height and body weight are changed across the three years (P-value < 0.001). Heights were 165.4 ± 8.5 cm in 2018, 165.5 ± 8.6 cm in 2019, and 166.2 ± 8.4 cm in 2020. Weights were 58.6 ± 12.5 kg in 2018, 58.9 ± 12.9 kg in 2019, and 60.0 ± 13.2 kg in 2020.
| Variables | Survey Year | ||
|---|---|---|---|
| 2018 | 2019 | 2020 | |
| Height, cm | 165.4 ± 8.5 | 165.5 ± 8.6 | 166.2 ± 8.4 |
| Weight, kg | 58.6 ± 12.5 | 58.9 ± 12.9 | 60.0 ± 13.2 |
| Gender (male) | 23,310 (50.1) | 23,667 (51.6) | 21,147 (52.8) |
| School year | |||
| 1st | 7,503 (16.1) | 7,819 (17.0) | 7,531 (18.8) |
| 2nd | 7,580 (16.3) | 7,543 (16.4) | 6,799 (17.0) |
| 3rd | 7,753 (16.7) | 7,923 (17.3) | 6,458 (16.1) |
| 4th | 7,338 (15.8) | 7,452 (16.2) | 6,439 (16.1) |
| 5th | 7,935 (17.0) | 7,283 (15.9) | 6,467 (16.1) |
| 6th | 8,452 (18.2) | 7,855 (17.1) | 6,359 (15.9) |
Demographic Characteristics for 3 Years a
4.2. Mood
After being weighted with represented students using complex sample methods (Table 2), those who felt unhealthy were estimated to be similar from 6.4% (95% CI 6.2 to 3.7) in 2018 to 6.8% (6.5 to 7.1) in 2020, and the proportion of students who did not feel stressed increased from 59.9% to 60.7% between 2018 and 2019, to 67.3% (66.7 to 67.9) in 2020 with statistical significance. Students who had been feeling sadness or desperation for the past 12 months were at 26.0 – 27.1% in 2018 and 2019, which decreased to 23.3% (22.8 to 23.8) in 2020 (P = 0.000). The percentage of students having suicidal thoughts decreased from 12.7 to 9.9% (9.5 to 10.2, P = 0.000).
When adjusted by school year and gender (Table 2), the odds ratio of students who felt unhealthy increased by 1.108 (1.049 to 1.170) in 2019, increasing by even more in 2020 (1.116; 95% CI 1.054 to 1.182, P = 0.000). The proportion of students who did not feel stressed statistically increased in 2020 (1.351; 1.308 to 13.95, P = 0.000). The proportion of students experiencing sadness and despair as well as suicidal thoughts, also decreased in 2020 with statistical differences (P = .000).
| Year | Estimated Ratio | P-Value | Adjusted a | P-Value | |
|---|---|---|---|---|---|
| Subjective health perception: Unhealthy | 2018 | 6.4 (6.2 – 6.7) | 0.021 | Ref. | |
| 2019 | 6.9 (6.7 – 7.2) | 1.108 (1.049 – 1.170) | 0.000 | ||
| 2020 | 6.8 (6.5 – 7.1) | 1.116 (1.054 – 1.182) | 0.000 | ||
| Stress perception: Not stressful | 2018 | 59.9 (59.2 – 60.6) | 0.000 | Ref. | |
| 2019 | 60.7 (60.1 – 61.4) | 1.024 (0.992 – 1.057) | 0.138 | ||
| 2020 | 67.3 (66.7 – 67.9) | 1.351 (1.308 – 1.395) | 0.000 | ||
| Recovery from Sleep b | |||||
| Sleep satisfaction: Insufficient | 2018 | 43.3 (42.5 – 44.1) | 0.000 | Ref. | |
| 2019 | 45.7 (45.0 – 46.4) | 1.127 (1.088 – 1.169) | 0.000 | ||
| 2020 | 34.0 (33.4 – 34.7) | 0.695 (0.668 – 0.722) | 0.000 | ||
| Sadness and despair: Yes | 2018 | 26.2 (25.7 – 26.8) | 0.000 | Ref. | |
| 2019 | 27.3 (26.8 – 27.9) | 1.069 (1.033 – 1.107) | 0.000 | ||
| 2020 | 23.3 (22.8 – 23.8) | 0.876 (0.844 – 0.908) | 0.000 | ||
| Suicidal thoughts: Yes | 2018 | 12.7 (12.3 – 13.0) | 0.000 | Ref. | |
| 2019 | 12.5 (12.1 – 12.9) | 0.986 (0.944 – 1.03) | 0.532 | ||
| 2020 | 9.9 (9.5 – 10.2) | 0.766 (0.730 – 0.804) | 0.000 | ||
Estimated Proportion of Subjective Health Perception, Feel Stressed, and Sleep Recovery According to Survey Year
4.3. Sleep and Sleepiness
The number of students who felt that they had an insufficient recovery from sleep fatigue significantly decreased from 42.6% in 2018 and 44.9% in 2019 to 33.5% in 2020 (Table 1). After adjusting for participants’ sex and school year (Table 2), the degree of recovery from sleep fatigue was worse with a statistical significance in 2019 compared to 2018, but improved in 2020 (0.695, 95% CI 0.668 to 0.722, P < 0.001).
Bedtime during weekdays and weekends was delayed in 2020 without a change in sleep duration in raw value. Sleep inconsistency and sleep for the entire week were also similar for 2018–2019 and 2020. After adjustment for sex and school grade (Table 3), participants slept 9.743 (7.957 – 11.530) minutes later and woke up 4.684 (3.449 – 5.919) minutes later on weekdays in 2020, as compared to sleep durations in 2018 and 2019. Therefore, their sleep duration significantly decreased by five minutes after the COVID-19 outbreak. They also slept 15.721 (14.077 – 17.366) minutes later and woke up 12.309 (10.393 – 14.225) minutes later, sleeping -3.413 (-5.419 – -1.407) minutes less on weekends during social distancing. The differences in sleep duration between the weekdays and weekends did not change significantly. However, the weekly sleep duration decreased significantly by up to 32 minutes.
| Year | Estimated Mean (95%CI) | Adjusted a (Min) | P-Value | |
|---|---|---|---|---|
| Bedtime weekday (hh:mm) | 2018 | 00:42 (00:40 – 00:43) | ||
| 2019 | 00:42 (00:41 – 00:43) | 0.688 (-1.109 – 2.484) | 0.453 | |
| 2020 | 00:51 (00:50 – 00:53) | 9.743 (7.957 – 11.530) | 0.000 | |
| Wake time weekday (hh:mm) | 2018 | 07:01 (07:00 – 07:02) | ||
| 2019 | 07:03 (07:02 – 07:04) | 1.831 (0.689 – 2.974) | 0.002 | |
| 2020 | 07:06 (07:05 – 07:07) | 4.684 (3.449 – 5.919) | 0.000 | |
| Sleep duration weekday (hh:mm) | 2018 | 06:19 (06:18 – 06:21) | ||
| 2019 | 06:20 (06:19 – 06:22) | 1.144 (-0.64 – 2.928) | 0.209 | |
| 2020 | 06:14 (06:13 – 06:15) | -5.059 (-6.817 – -3.301) | 0.000 | |
| Bedtime weekend (hh:mm) | 2018 | 01:14 (01:13 – 01:15) | ||
| 2019 | 01:16 (01:15 – 01:17) | 2.009 (0.372 – 3.647) | 0.016 | |
| 2020 | 01:30 (01:29 – 01:31) | 15.721 (14.077 – 17.366) | 0.000 | |
| Wake-time weekend (hh:mm) | 2018 | 09:20 (09:19 – 09:21) | ||
| 2019 | 09:20 (09:19 – 09:22) | 0.268 (-1.540 – 2.076) | 0.771 | |
| 2020 | 09:32 (09:31 – 09:34) | 12.309 (10.393 – 14.225) | 0.000 | |
| Sleep duration weekend (hh:mm) | 2018 | 08:05 (08:04 – 08:07) | ||
| 2019 | 08:04 (08:02 – 08:05) | -1.741 (-3.775 – 0.292) | 0.093 | |
| 2020 | 08:02 (08:01 – 08:03) | -3.413 (-5.419 – -1.407) | 0.001 | |
| Sleep discrepancy (min) | 2018 | 106.2 (104.8 – 107.6) | ||
| 2019 | 103.3 (102.0 –104.6) | -2.885 (-4.763 – -1.007) | 0.003 | |
| 2020 | 107.8 (106.5 – 109.2) | 1.646 (-0.277 – 3.570) | 0.093 | |
| Sleep for a week (min) | 2018 | 2870.6 (2862.5 - 2878.8) | ||
| 2019 | 2872.9 (2864.8 – 2881.0) | 2.236 (-9.339 – 13.811) | 0.705 | |
| 2020 | 2838.5 (2830.7 - 2846.3) | -32.121 (-43.411 – -20.83) | 0.000 |
Estimated and Gender/School Year Adjusted Sleep Time and Duration
5. Discussion
This study was conducted to assess the effects of social distancing on teens’ sleep and proportionally stratified sampled the entire teen population in Korea as a cohort. It showed that social distancing caused teens to sleep late, have decreased sleep durations, and experience more regular sleep. Furthermore, teens became less stressed and less depressed, with a decreased proportions of students reporting insufficient sleep in 2020. After COVID-19, teens fell asleep and woke up later, on both weekdays and weekends. Although the total amount of sleep over the week decreased, the differences in sleep duration between weekdays and weekends did not change. More students felt unhealthy but fewer students felt stressed and sleep deprived. Moreover, fewer teens experienced sadness and suicidal thoughts.
An important regulator of sleep for adolescents is their school attendance, and any change in the latter has the potential of making this regulator weak. School starting times are also a potent regulator affecting teens’ routine in a variety of ways, such as eating breakfast, getting dressed, walking or riding a bus to commute to school, and observing sunlight. However, because of COVID-19, outdoor activities, such as walking, physical exercises, or observing sunlight during school hours would have decreased (18). Even though teens’ sleep phase is physiologically delayed after the onset of puberty, it still suffers from restrictions due to the gradually increasing school time. The social distancing and lockdown caused by COVID-19 have changed the style and nature of classes in many countries around the world, altering the pattern of teens’ daily life. Both synchronous and asynchronous online classrooms have created flexibility in the potent regulator of teens’ sleep.
Unlike the results of our study, previous studies reported a decrease in sleep quality after lockdowns. On surveying social media platforms immediately after social distancing, it was reported that adults also went to bed late and woke up late, reducing their night sleep time and increasing their naptime (19). Increased obesity and obstructive sleep apnea were also reported, resulting in poor sleep quality (20). Sleep quality decreased due to rapid changes in lifestyle during the early stages of the COVID-19 pandemic, causing people to experience negative moods without the change of daytime sleepiness (13). A review paper also reported that 36% of medical professionals and 32% of the general population suffered from sleep problems (21). In the case of college students, during stay-at-home orders, sleep time increased by about 30 minutes on weekdays, and by 24 minutes on weekends. Sleep inconsistencies also decreased by about 12 minutes. They reportedly slept 50 minutes late on weekdays and 25 minutes late on weekends (22). Accordingly, social jet lag decreased in this group. Furthermore, other cases of college students indicated worse mood and poor quality of sleep (23). Another study found that weight did not increase significantly during lockdown, but sleep problems increased and self-perceived well-being decreased (12).
Another possible cause for the contrary results of sleep efficiency may be due to the participants’ depressed mood in the early pandemic phase. The survey for this study was conducted in Korea during summer, when people were already accustomed to social distancing and the number of infected cases was decreasing four to five months after the initial spread of the pandemic. Therefore, it is highly likely that our survey was conducted post an improvement in previously depressed moods. During the early spread of COVID-19, many studies showed an increase in mood disorders (24). In addition, there was a report stating that negative moods were severe during the initial period: April–June 2020 (14). A depressed mood generally affects sleep quality and efficiency. Therefore, due to this discrepancy the results of our study may differ from those of previous studies. Poor sleep quality is clearly associated with depression (25, 26). Even in teens and children with a high risk of depression, an increase in waking after sleep onset and a decrease in sleep efficiency have been observed (27).
In addition to differences in mood, the synchronization of teens’ sleep time and their internal sleep phases could be another cause for increase in sleep efficiency after COVID-19. Among the various factors that determine sleep efficiency, there is the degree of matching between the internal sleep phase and actual sleep (28). A typical example of the decrease in sleep efficiency due to a sleep phase mismatch is poor sleep quality in shift workers (29). It has been reported that the amount of slow wave sleep in shift workers is inversely proportional to the phase mismatch. One objective paper states that sleep efficiency on polysomnography and the dim light melatonin onset value, which is representative of the internal sleep phase, are related (30). In the same study, it was concluded that there was a negative correlation between the difference in internal phase and bedtime and sleep efficiency. Another study showed that abrupt changes in sleep time can decrease sleep duration and sleep efficiency (8, 31).
In this study, improved sleep quality in 2020 is indirectly supported by decreased sleep duration and improved sleep sufficiency in 2020. Moreover, this is also supported by the fact that sleep inconsistencies did not increase after social distancing, even though sleep durations decreased. The differences in sleep durations between weekdays and weekends is indicated by catch-up sleep to pay off the sleep debt that was lacking during weekdays (32). In this study, insufficient sleep compared to habitual sleep durations appeared as a potential sleep debt (32). When teens could sleep freely, the amount of rebound sleep and potential sleep debt were directly proportional (33). Weekend catch-up sleep is correlated with poor school performance due to potential weekday sleep restrictions, which can be a useful tool to check for sleep insufficiency (2). With these results, it can be suggested that teens’ sleep time has clearly decreased after COVID-19, but sleep debt and sleep insufficiency are similar to those during pre-COVID-19 times.
This study has a few limitations. At the time of the investigation, we only had information that most students attended school rotationally. Therefore, this study could not include individual class type information. As the survey period was extended due to COVID-19, the seasonal homogeneity had disappeared. To avoid errors, teens with extreme values of sleep time were excluded, thus the results might have been distorted and biased. Moreover, we did not include daytime naps as a variable. Lastly, the subjective sleep duration could be overestimated compared to the objective assessment (34).
Online classes due to COVID-19 have altered teens’ sleep patterns dramatically. Flexible school times as a sleep regulator was associated with effective sleeping patterns among teens. Post recovery from COVID-19, school systems could assess their timings and the nature of class delivery such that they benefit teens’ sleep efficiency.
5.1. Conclusions
To the best of our knowledge, this study is the largest national study on the effects of social distancing on teens’ sleep which proportionally samples all teens in a country as cohort. During social distancing due to COVID-19, teens fell asleep and woke up later, and slept less both on weekdays and weekends. Although the total amount of sleep per week decreased, the difference in sleep durations between weekdays and weekends did not change. More students felt unhealthy but fewer students felt stressed and sleep deprived.