1. Background
Foreign body aspiration (FBA) is a common problem for children and the leading cause of accidental death among children between 0 - 3 years, in whom 7% of deaths are due to this reason (1, 2). The clinical manifestation of patients with FBA varies according to the location and size of the foreign body (3). Rigid bronchoscopy is the gold standard method of treatment (4). Bradycardia due to bronchospasm and desaturation are challenging complications and may even lead to death during this procedure (5). Different agents are being used to avoid these complications. In this regard, β2 agonists (salbutamol) have the strongest bronchodilation effect on the bronchial smooth muscle of the airway. With its fast onset of action (5 minutes), it is particularly suitable for management and has a duration of action of 4 - 6 hours in most patients. Also, it has anti-inflammatory effects because of reducing intercellular adhesion molecule-1 (ICAM-1), granulocyte-macrophage colony-stimulating factors (GM-CSF) release, and inhibits multiple inflammatory pathways (6, 7).
Glucocorticoids have immunomodulatory effects on airway smooth muscle cells (8). Dexamethasone, which expresses transcription factors in airway epithelial cells and lung fibroblasts, controls airway inflammation by reducing mucus hypersecretion (9).
2. Objectives
This study was conducted on children who underwent rigid bronchoscopy due to foreign body aspiration. We aimed to evaluate the effect of preoperative dexamethasone and β2 agonist (salbutamol) administration and compare the effect of those agents administered 30 minutes before the procedure and during the anesthetic induction.
3. Methods
The study was performed in adherence to the Declaration of Helsinki and was approved by the Local Ethics Committee (no: 08-416-17) on May 2017. Written informed consent was taken from all parents. Fifty-four patients who underwent elective bronchoscopy because of the aspirated foreign body between August 2017 and January 2019 were enrolled prospectively in the study. Children were divided into two groups independent of their clinical conditions via random numbers table. β2 agonists (salbutamol) (2.5 mg < 20 kg, 5 mg > 20 kg) and dexamethasone (0.5 mg/kg) with ranitidine (1 mg/kg) were administrated to group 1, 30 minutes before the procedure. The same agents were administrated intravenously to group 2 with the anesthetic induction. Demographic data, the occurrence of bronchospasm, desaturation, and bradycardia were evaluated. The data were analyzed using the SPSS for Windows (SPSS 23.0 IBM, Armonk). Mann-Whitney U test was used to compare the two groups. P-values less than 0.05 were considered statistically significant.
4. Results
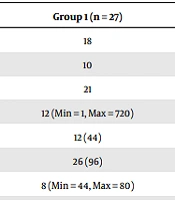
Fifty-four children were enrolled in the study. There were 27 children in each group. Indications for bronchoscopy were history of aspiration, signs of aspiration or examination findings supporting aspiration or chest X-rays findings. The mean age of groups 1 and 2 were 18.2 months (8 - 48 months) and 18.4 months (3 - 81 months), respectively. There were 21 females and 33 males in the study. Foreign bodies were localized in the right bronchial tree in 15 cases (55.6%), the left in 11 cases (40.7%), both right and left bronchial trees in one case (3.7%) in group 1. For group 2, they were localized in the right bronchial tree in 17 cases (62.9%) and the left in ten cases (37.1%). The time period between the onset of the symptoms and the procedure was similar in the two groups (P > 0.05). Since the children who were intervened in emergency conditions were excluded from the study, two groups were similar in clinical aspects. The bronchospasm, desaturation, and bradycardia count were similar in both groups (P = 0.37, P = 0.72, P = 0.24). Clinically, periods of spasm and desaturation were shorter, and patients recovered faster in group 1. The preoperative, operative, and postoperative findings are presented in Table 1.
| Clinical Presentation | Group 1 (n = 27) | Group 2 (n = 27) |
|---|---|---|
| Cough (n) | 18 | 19 |
| Desaturation | 10 | 6 |
| Wheezing | 21 | 15 |
| Durations between aspiration and bronchoscopy | 12 (Min = 1, Max = 720) | 24 (Min = 2, Max = 1060) |
| Radiographic finding (+) | 12 (44) | 14 (51) |
| Operative aspirated material (organic) | 26 (96) | 23 (85) |
| Desaturation (O2 sat < 80%) | 8 (Min = 44, Max = 80) | 13 (Min = 3, Max = 80) |
| Bradycardia | 0 | 2 |
| Bronchospasm | 5 | 7 |
| Granulation | 2 | 3 |
| Complication | 1 (Bleeding) | 0 |
| Mortality | 0 | 0 |
| Postoperative complication | 0 | 0 |
| Discharge time (hours) | 32 (Min = 1, Max = 80) | 30 (Min = 12, Max = 72) |
a Values are expressed as No. (%) unless otherwise indicated.
5. Discussion
This study aimed to evaluate the effects of preoperative β2 agonist (salbutamol) and dexamethasone administration on operative complications such as bronchospasm, desaturation, and bradycardia. Even though the results regarding these complications showed no statistical significance, the authors observed a slightly better clinical course in the group 1.
Foreign body aspiration is one of the children’s most common reasons for life-threatening situations (10). It is the leading cause of accidental death in children 0 - 4 years old (1). Males are observed to be more prone to aspirate foreign bodies than females in many studies except the turban-pin aspiration in adolescent fs in some studies (10). The most common findings are the history of choking, coughing, and wheezing (11). The new onset of any of these symptoms or history alone is a certain indication for rigid bronchoscopy (12). Kiyan et al. showed that the sensitivity and specificity of physical examination are 94.6% and 46.4%, respectively (13). Direct chest X-ray is usually enough for imaging but may not always lead to positive findings (11).
Foreign bodies may cause radiological signs in direct chest X-ray, such as unilateral or localized hyperlucency and mediastinal shift (3). An abnormal chest X-ray is observed in 42 - 73%, and normal chest X-ray is found in 33 - 52.4% of patients (14). Low-dose chest CT and virtual bronchoscopy are rarely used when there is a suspected complication (3, 15).
The former treatment choice was non-endoscopic in the past, with only bronchodilators and postural drainage, but it evolved to rigid bronchoscopy because of the fatal risks of the method (15). But even rigid bronchoscopy comes along with severe complication risks such as bronchospasm, desaturation, bradycardia, respiratory and cardiac arrest, and death (16). Even though mortality is rare, other operative complications may be seen in 2 - 3% (11). β2 agonists (salbutamol), corticosteroids, and atropine sulfate have been used to avoid these preoperatively or intraoperatively (11, 15, 17, 18). In the literature, many studies have used premedication with salbutamol 10-30 min before surgery for perioperative respiratory adverse events such as bronchospasm (19-21). von Ungern-Sternberg et al. showed that β2 agonists (salbutamol) decreased the incidence of bronchospasm and desaturation during the perioperative period in asthmatic children (19). Jiang et al. showed that preoperative β2 agonists (salbutamol) 30 min before surgery decreased the occurrence of bronchospasm and new-onset pulmonary infiltration in patients (22). Akcora et al. used a combination of nebulized albuterol and budesonide starting right after the hospitalization and stated a significant decrease in bronchospasm and desaturation during bronchoscopies in their retrospective study (15). In the present study, even though the statistics showed no significance, the authors observed a slight relief in the clinical conditions of the children. It was easier to remove foreign bodies with the bronchodilation developed in patients who were given β2 agonists (salbutamol) 30 minutes before the procedure. In this way, the duration of the operation of group 1 patients was shortened. Although it was not statistically significant, it was clinically observed that the duration of bronchospasm and desaturation during the procedure were shorter and the patients recovered faster after the procedure. The minimum O2 saturation was 3 in the group 2, while it was 44 in the group 1. There were two periods of bradycardia in the group 2. Clinically, periods of spasm and desaturation were slightly shorter in the group 1. Therefore, we may suggest that a larger data set in future studies may lead to more significant results and a better evaluation to conclude. The limitations of the study may be the relatively small number of patients and absence of a control group without any medications.
5.1. Conclusions
The rigid bronchoscopy may be the first choice of treatment, but it has severe complication risks. Severe complications, including death, still cannot be totally avoided, and medication prior to or during this procedure may reduce the risks. Randomized studies with a higher number of patients searching for more effective agents may lead to more certain results.