1. Background
The urethra is a common route for acquiring urinary tract infections (UTIs) in children (1). Among children, the average prevalence of UTIs accompanied by fever is 7%. In children under one year of age, the incidence of UTI has been 2% in girls and 3.7% in boys (2), with a higher prevalence among uncircumcised male infants (3). Regarding the indeterministic clinical symptoms of UTI in very young patients, these people are susceptible to delayed diagnosis and, therefore, complications such as chronic hypertension in the long run (4).
The diagnosis of UTI relies on suggestive clinical signs, urinalysis (UA) findings, or both. A urine culture is essential to confirm the diagnosis and determine the appropriate treatment (5). Currently, UA is performed using two methods. In the standard microscopic method, a centrifuged urine sample is inspected for the presence of white blood cells (WBC), bacteria, red blood cells, and crystals. In this method, pyuria is defined as the presence of 5 ≥ WBC/high-power field (hpf). However, this technique is relatively time-consuming and has low sensitivity because the Brownian motion of particles may cause them to be misidentified as mobile bacteria. In addition, manual UA is an operator-dependent method subjected to variations due to different duration of centrifugation and resuspension, as well as technical expertise.
Enhanced microscopy, which is currently used in some centers, is performed via the microscopic examination of uncentrifuged urine samples using the hemocytometer method (6). This technique uses Gram-stained smears to detect bacteria in hpf microscopic views. Several investigations have shown that enhanced microscopy is a sensitive tool for detecting bacteriuria (7). However, the applicability of this technique in children is less studied, especially among Iranian populations.
2. Objectives
We aimed to assess the diagnostic value of enhanced UA in the diagnosis of UTIs in children with presumptive infections.
3. Methods
This cross-sectional study was conducted on 191 consecutive patients referred to Dr. Sheikh Hospital, Mashhad, Iran. We included patients who were aged < 18 years and were suspected of having UTIs. Children treated with antibiotics before sampling or those suffering from underlying diseases predisposing to UTI were excluded from the study. The parents of all patients were requested to provide informed consent for participation in the study. The study protocol was approved by the Ethics Committee of Mashhad University of Medical Sciences (ethical code: IR.MUMS.fm.RC.1396.776).
Demographic and clinical data of the patients were recorded. Midstream clean-catch urine samples were collected from the patients who had urinary control, and bladder catheterization was used for infants or children unable to void on request.
Urine analysis was performed for each patient using both standard and enhanced methods. Also, quantitative urine culture was performed for each sample. The standard UA method included standard microscopy, in which a centrifuged urine sample was used to examine WBCs, erythrocytes, and crystals. In this method, pyuria was defined as the presence of ≤ 5 WBCs/hpf. The samples were then subjected to the enhanced UA method, which relies on the microscopic examination of uncentrifuged urine samples using a hemocytometer slide. For urine culture, the specimens were inoculated into plates containing 5% sheep blood agar by a 0.01 mL calibrated loop, followed by incubation at 35 – 37°C. Culture results were read after 24 to 48 hours of incubation. A positive urine culture was defined as ≥ 50000 colony-forming units (CFU), according to the current clinical guidelines of the American Academy of Pediatrics (8).
Urinalysis using a dipstick and cell count was also performed in a standard way to predict infections in children based on the nitrite and leukocyte esterase bands.
3.1. Statistical Analysis
Based on Hoberman et al.’s study, which reported a rate of 85% for positive manual microscopy results among patients with suspected UTI, and considering type I error (α) of 0.05 and type II error (β) of 0.20, the sample size was calculated as 196 according to the following formula (9).
The data were recorded in SPSS software and analyzed. The characteristics of the subjects were described by descriptive statistics, including central tendency indices, dispersion indices, and frequency distribution, presented in the form of tables. The chi-square test (or Fisher’s exact if necessary) and independent t-test were used to compare the qualitative variables between the two groups. In all calculations, the value of 0.05 was considered significant.
4. Results
Among 191 patients, 122 were females (63.9%), and 69 were males (36.1%). The mean age of the patients was 5.1 ± 3.3 years; the minimum age was one month, and the maximum age was 15 years. Most children had urinary symptoms (62.3%), including fever (38.2%) and abdominal pain (23.6%, Table 1).
| Variables | UTI Negative (N = 147) | UTI Positive (N = 44) | Total | P Value |
|---|---|---|---|---|
| Age (y) | 5.1 ± 3.3 | |||
| Sex (male) | 8 (18.2) | 61 (41.5) | 69 (36.1) | 0.005 |
| Clinical symptoms | ||||
| Fever | 20 (45.5) | 53 (36.1) | 73 (38.2) | 0.26 |
| Nausea/vomiting | 2 (4.5) | 4 (2.7) | 6 (3.1) | 0.62 |
| Restlessness | 5 (11.4) | 24 (16.3) | 29 (15.2) | 0.42 |
| Abdominal pain | 13 (29.5) | 32 (21.8) | 45 (23.6) | 0.29 |
| Diarrhea | 0 (0) | 3 (2) | 3 (1.6) | 0.99 |
| Urinary symptoms | 31 (70.5) | 88 (59.9) | 119 (62.3) | 0.20 |
Demographic Data and Clinical Characteristics of Patients with or Without UTI a
Forty-four samples (23%) were diagnosed with UTI, while others had negative urine culture results. In the initial UA by the standard method, 37 (19.4%) patients had hematuria, and 70 (36.64%) patients had pyuria. Furthermore, 27 (14.1%) patients were positive for nitrite, and 40 (20.9%) were leukocyte esterase positive. Pyuria, positive nitrite, and positive leukocyte esterase were significantly more prevalent in UTI-positive than in UTI-negative patients (P < 0.001, Table 2).
| Urine Analysis Method | UTI Results | |||
|---|---|---|---|---|
| UTI Positive (N = 44) | UTI Negative (N = 147) | Total (N = 191) | P Value b | |
| Manual | ||||
| Nitrite test (+) | 25 (56.8) | 2 (1.4) | 27 (14.1) | < 0.001 |
| Leukocyte esterase test (+) | 32 (72.7) | 8 (5.4) | 40 (20.9) | < 0.001 |
| Pyuria | 40 (90.9) | 30 (20.4) | 70 (36.6) | < 0.001 |
| Hematuria | 11 (25) | 26 (17.7) | 37 (19.4) | 0.28 |
| Enhanced | ||||
| Gram staining | 44 (100) | 15 (10.2) | 59 (30.9) | < 0.001 |
| Pyuria | 43 (97.7) | 29 (19.7) | 72 (37.7) | < 0.001 |
| UTI enhanced method | 43 (97.7) | 10 (6.8) | 53 (27.7) | < 0.001 |
Urine Analysis Results Using Manual and Enhanced Methods According to the Presence or Absence of UTI a
Based on the enhanced UA method, 72 (37.7%) of the patients had pyuria. Gram staining indicated that 59 (30.9%) patients were positive for the presence of bacteria, and 132 (69%) patients were negative in this regard. Pyuria and Gram-staining positive samples were significantly higher among UTI-positive than in UTI-negative patients (P < 0.001, Table 2).
The sensitivity of the nitrite test to detect UTI was calculated as 56.8%, and its specificity was calculated as 98.7%. The sensitivity and specificity of the leukocyte esterase test to detect UTI were 72.7% and 94.5%, and these values were 90.9% and 79.5% for pyuria, respectively.
Among patients diagnosed with UTIs, all 44 patients had a positive Gram-staining result in the enhanced method. The sensitivity of bacteriuria based on Gram staining by the enhanced UA method for detecting UTI was equal to 100%; its specificity was 89.7%, and its positive predictive value (PPV) and negative predictive value (NPV) were 74.5% and 100%, respectively. Regarding the enhanced UA method, sensitivity, specificity, PPV, and NPV of pyuria for identifying UTI were 97.7%, 80.2%, 59.7%, and 99.1%, respectively.
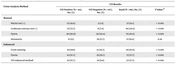
The sensitivity of the enhanced UA method for detecting UTI was obtained as 97.7%; the specificity was 93.1%, and PPV and NPV were 81.1% and 99.3%, respectively (Table 3).
| Variables | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| Manual method | ||||
| Pyuria | 90.9 | 80.7 | 57.1 | 96.9 |
| Nitrite | 56.8 | 98.7 | 92.5 | 88.4 |
| Leukocyte esterase | 72.7 | 94.5 | 80 | 92 |
| Enhanced method | ||||
| Gram staining | 100 | 89.7 | 74.5 | 100 |
| Pyuria | 97.7 | 80.2 | 59.7 | 99.1 |
| Pyuria + bacteriuria | 97.7 | 93.1 | 81.1 | 99.3 |
Diagnostic Values of Manual and Enhanced Urine Analysis
5. Discussion
Urine analysis is the method of choice for the primary diagnosis of UTI. This method is performed using two techniques, including manual and enhanced. The manual technique is time-consuming and operator-dependent and offers a relatively low diagnostic performance. The enhanced method has been shown to provide an accurate test for detecting UTIs, and it needs a lower volume of urine compared to the conventional method. However, the clinical utility of the enhanced technique is less specified in children, especially in Iran.
We found that in standard UA, the sensitivity of pyuria for the initial diagnosis of UTI was 90.9%, and its specificity was 80.7%. In the enhanced method, the sensitivity of pyuria and bacteriuria for identifying UTI rose to 97.7% and its specificity to 93.1%, with PPV and NPV of 81.1% and 93.9%, respectively. These findings show that the enhanced technique was superior to the manual method. The higher sensitivity and specificity of the enhanced method indicated that this technique could accurately diagnose patients with UTI, ruling out healthy patients at an acceptable rate. In a similar study by Shah et al. (10) conducted on 703 children with suspected UTI, the sensitivity of the enhanced method was 77.5%, and its PPV was reported as 84.4%. In our study, the sensitivity of the enhanced method for detecting UTI was 97.7%; the specificity was 93.1%, and PPV and NPV were 81.1% and 939%, respectively. In our study, the sensitivity of pyuria (10 ≥ WBC) calculated by the enhanced method alone in predicting UTI was equal to 97.7%, and its PPV was equal to 59.7 %. However, in Shah et al.’s study (10), the sensitivity was 83.6%, and PPV was 53.5%. In addition, Shah et al. reported a sensitivity of 79.5% and PPV of 37.5% for pyuria for the diagnosis of UTI (10), which were lower compared to the respective values (90.9% and 57.1%) obtained in our study.
In another study by Suresh et al. (11), it was shown that both enhanced and standard UA techniques had low sensitivity (< 70%), while their specificities were 88% and 92%, respectively. Kabilan (12) reported the sensitivity and specificity of the enhanced UA method as 89.5% and 93.2%, respectively, suggesting that the enhanced technique had a better diagnostic performance compared to the manual method.
In a study by Fernandez et al. (8), the sensitivity of the nitrite test was reported to be 47.37%, and its specificity was 93.94%. In our study, the sensitivity and specificity of the nitrite test for UTI diagnosis were 56.8% and 98.7%, respectively. Fernandez et al. (8) reported that the sensitivity and specificity of the leukocyte esterase test for UTI diagnosis were 42.11% and 75.76%, respectively. In our study, the sensitivity and specificity of the leukocyte esterase test for detecting UTI were calculated as 72.7% and 94.5%, respectively.
In Khodami et al.’s (13) study, in which 600 patients were enrolled, the sensitivity and specificity of the standard UA method for detecting UTI were described as 64.8% and 89%, along with the PPV and NPV of 51.3% and 93.4%, respectively. In our study, the sensitivity, specificity, PPV, and NPV of pyuria according to the standard method were 90.9%, 80.7%, 57.1%, and 96.9%, respectively.
In a study by Lin et al. in 2000, conducted on 230 febrile children under one year of age, pyuria in the enhanced method (defined as ≥ 10 WBC using a hemacytometer) delivered a significantly higher sensitivity and PPV than the same test in the context of the standard technique (WBC ≥ 5) (14).
Urinary tract infections are among the most common infectious diseases in children, and a delay in their diagnosis can have serious harmful consequences. Currently, UA using a dipstick and standard cell counting is used to predict the risk of UTI in children. In this study, it was shown that the enhanced method had higher sensitivity, specificity, PPV, and NPV than the standard UA method, providing a faster diagnostic modality.
Among different urine collection methods, collection through a urinary catheter or using the suprapubic method are considered more accurate and superior methods to diagnose UTIs; however, due to the invasive nature of these methods, they cannot be used in all children suspected of having UTI. The importance of this issue is more pronounced in children who are not toilet-trained and cannot use the more acceptable method of midstream urine collection. Therefore, such young children require using a urine bag for specimen collection, increasing the possibility of contamination. Thus, if positive results are yielded, further investigation is required. It should be noted that culture results from urine samples collected through urine collection bags deliver a relatively high NPV for urinary infections.
5.1. Study Limitations
This study suffered from several limitations. First, our sample size was relatively small compared to similar studies. Second, our specimens were examined by various laboratory technicians; therefore, our results may be hampered by the possibly different experience levels of these technicians. However, we believe that this factor increases the generalizability of our data since many hospital laboratories have settings similar to that of our study.
5.2. Conclusions
Our study showed that the enhanced UA technique offered a better diagnostic procedure for screening UTIs in children compared to the manual technique. This method should be considered the primary laboratory option when evaluating children with presumptive UTIs due to its accuracy and cost-effectiveness. A lower volume of urine is required in the enhanced technique, which adds to its value considering that urine volume is a challenge when testing pediatric populations.