1. Background
The current status of delayed diagnosis of CHD is not promising. A study in a high-income country showed that the proportion of delayed diagnosis of CHD was 8.9%, including 10.4% of non-cyanotic CHD, and 8.7% of cyanotic CHD (1). Another study demonstrated that the proportion of delayed diagnosis of critical CHD was 29.5% (2). Previous study in a low-middle-income country showed that the proportion of delayed diagnosis of CHD was 85.1%, which was due to inadequate health system training and socioeconomic limitation (3). Murni et al. reported that the proportions of delayed diagnosis of children with non-cyanotic and cyanotic CHD were 54.9% and 86.2%, respectively, and delayed diagnosis caused by physicians was the most common reason (4). At the time of definitive diagnosis, 49.4% and 15.8% of the children with CHD had already developed heart failure and pulmonary hypertension, respectively (4). Therefore, the early detection, diagnosis, and treatment of CHD are very important.
Hainan is the southernmost underdeveloped province in China, where the technology of screening, diagnosis, and treatment of CHD in children has not been fully developed, resulting in a considerable number of children with CHD who do not receive timely treatment.
2. Objectives
This study, therefore, aimed to introduce and promote an appropriate technology system for screening, diagnosing, and evaluating the neonatal CHD in Hainan province in order to obtain the epidemiological data, provide early detection, improve treatment, as well as facilitate formulation of management policies on the given disease by providing additional support for the health department of local government.
3. Methods
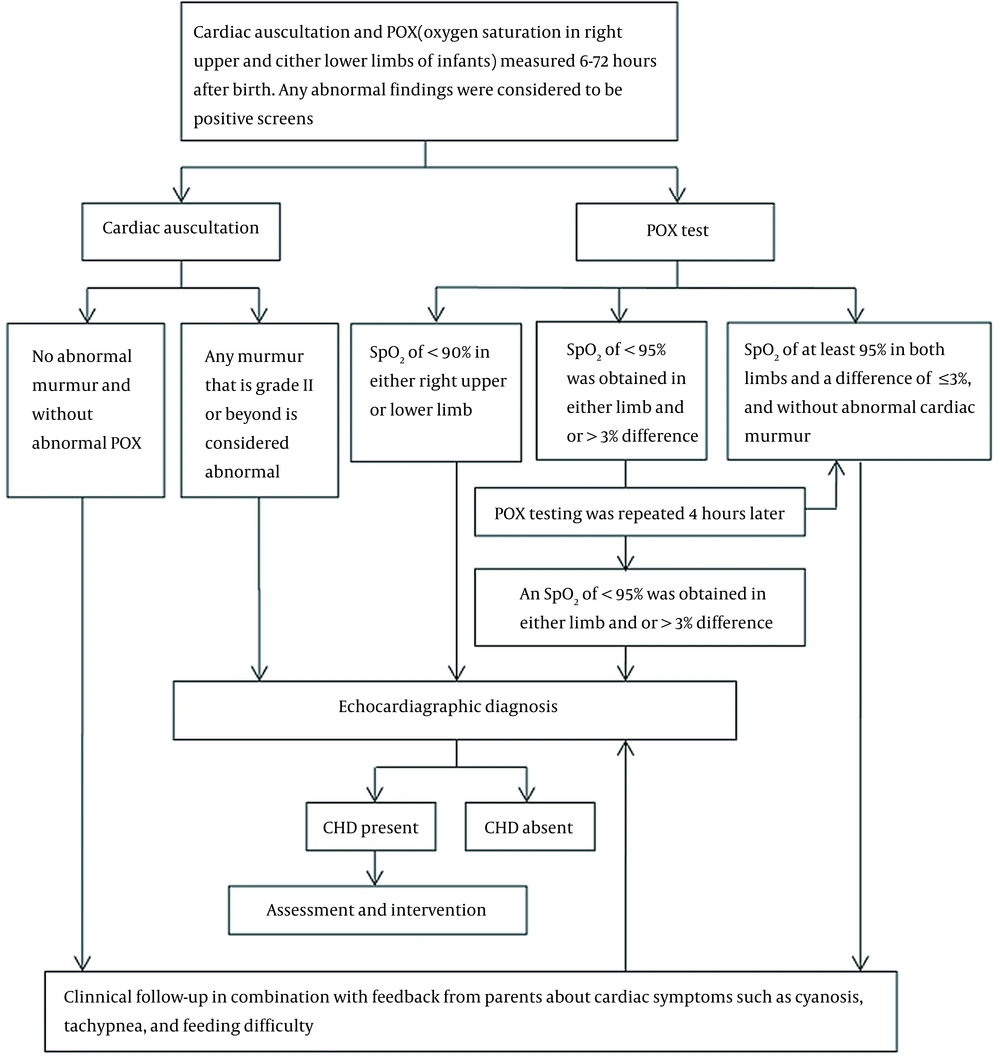
Live newborns (six to 72 hours after birth) from all delivery institutions located in 17 cities and counties in Hainan Province, including those referred to the local neonatal departments or NICUs due to illnesses, were recruited into this study from January 1, 2019, to December 31, 2021. Our study protocol is shown in Figure 1 (5). Cardiac auscultation was performed on the five points of auscultation (i.e., pulmonic, aorta, Erb’s point, tricuspid, and mitral) for each newborn, and the duration lasted at least 60 seconds per neonate. Pulse oxygen saturation (SpO2) was measured using the right hand and on either foot, and SpO2 levels were recorded on a report sheet. Cardiac auscultation was performed and immediately followed by POX measurement. A positive screen result was defined as the presence of any abnormality in the two examinations (Figure 1). Neonates who screened positive for CHD were referred for echocardiography within seven days.
Our institution was the main center used in this study, conducting standardized training for the screening staff in various cities and counties. The procedures of this study were as follows: (1) CHD screening procedure: All delivery institutions in 17 cities and counties of Hainan province, including the local neonatal departments or NICUs, were certified by Hainan Provincial Health Commission as screening institutions. Before implementing the CHD screening procedure, the screening staff were authorized after homogenized training, and informed consents were obtained from the guardians. The live newborns were screened by the staff using two indicators (i.e., cardiac auscultation and POX) within six to 72 hours after birth. (2) CHD diagnosis procedure: As diagnosis institutions certified by Hainan Provincial Health Commission, the 31 medical institutions performed echocardiographic examination for the screened-positive newborns in a week. During the follow-up for 12 months, the screened-negative newborns also underwent echocardiography at the diagnosis institutions as long as they developed CHD symptoms, such as cyanosis, tachypnea, and feeding difficulty. (3) CHD evaluation procedure: The qualified cardiovascular physicians and cardiac surgeons from the evaluation institutions checked the diagnosis results and performed necessary reevaluation, then provided medical suggestions or implemented treatments for the children confirmed with CHD. The six tertiary hospitals certified as evaluation institutions were as follows: Hainan Provincial Women and Children's Medical Center, the First Affiliated Hospital of Hainan Provincial Medical College, The Second Affiliated Hospital of Hainan Provincial Medical College, Hainan Provincial People's Hospital, Haikou Municipal People's Hospital, and Sanya Municipal Maternal and Child Health Care Hospital. (4) Review procedure: Values for screening indicators for CHD detection were evaluated. The data of this project were uploaded to a dedicated neonatal CHD screening information management net (https://www.nchd.org.cn/Admin/System/Admins/login).
Using echocardiographic diagnosis as the "gold standard", children with confirmed CHD were included. The following conditions were excluded from the study: (1) simple patent foramen ovale (PFO); (2) patent ductus arteriosus (PDA) that closed spontaneously within three months; and (3) simple malformation without hemodynamic significance. Definitions for the severity of CHD are as follows: Insignificant CHD, significant CHD, serious CHD, and critical CHD (6, 7). In this study, critical and serious cases of CHD were classified as major CHD, and significant and insignificant cases were classified as minor CHD.
Clinical data were analyzed using SPSS version 17.0 software package. Categorical variables were expressed as count and percentage. Differences between the groups regarding categorical variables were compared using the chi-square test, and P-value of <0.05 was considered statistically significant. Values of different screening indicators for neonatal CHD detection, including true positive, true negative, false positive, false negative, sensitivity, specificity, and Yoden index, were calculated separately. Informed written consent was obtained from the participating infants’ guardians.
4. Results
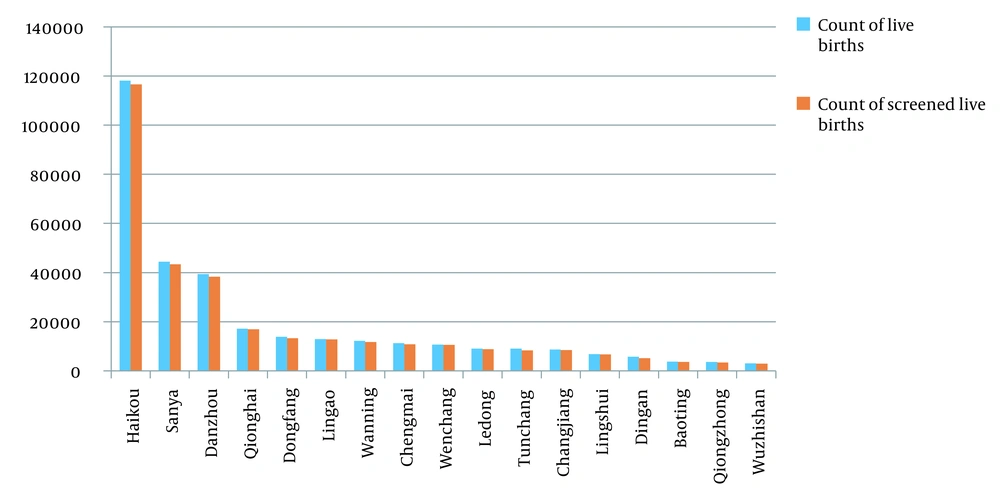
From January 1, 2019, to December 31, 2021, the count of live births in Hainan Province was 329387. The CHD screening was performed on 321447 live births, including 163246 males, and the overall screening rate was 97.59% (321447/329387). Furthermore, 8032 cases were screened-positive, suggesting a screened positive rate of 2.50% (8032/321447). The counts of live births and screened live births in different cities and counties are presented in Figure 2.
All screened-positive newborns underwent echocardiography examination immediately. According to our results, 1010 cases were confirmed to have CHD, out of who 8032 cases were the screened-positive newborns. During the follow-up, 89 cases of children with minor CHD were identified as follows: 44 cases of atrial septal defect (ASD), 26 cases of patent ductus arteriosus (PDA), 10 cases of ventricular septal defect (VSD), 5 cases of pulmonary valve stenosis, 3 case of partial anomalous pulmonary venous connection, and 1 case of aortic coarctation. A total of 1099 children were confirmed to suffer from CHD, suggesting an overall CHD prevalence of 3.419 per 1000 live births. The most common congenital heart lesion was ASD, with a prevalence of 1.313 per 1000 live births, followed by VSD (0.952) and PDA (0.653) (Table 1). The prevalence of insignificant, significant, serious, and critical CHD were 1.680, 1.260, 0.376, and 0.103 per 1000 live births, respectively.
| Subtype of CHD | Male (N = 565) | Female (N = 534) | Total (N = 1,099) |
|---|---|---|---|
| Atrial septal defect | 216 (1.323) | 206 (1.302) | 422 (1.313) |
| Ventricular septal defect | 159 (0.974) | 147 (0.929) | 306 (0.952) |
| Patent ductus arteriosus | 112 (0.686) | 98 (0.619) | 210 (0.653) |
| Pulmonary valve stenosis | 15 (0.092) | 18 (0.114) | 33 (0.103) |
| Partial anomalous pulmonary venous connection | 10 (0.061) | 13 (0.082) | 23 (0.072) |
| Tetralogy of Fallot | 11 (0.067) | 10 (0.063) | 21 (0.065) |
| Partial atrioventricular septal defect | 5 (0.031) | 7 (0.044) | 12 (0.037) |
| Total anomalous pulmonary venous connection | 5 (0.031) | 4 (0.025) | 9 (0.028) |
| Transposition of the great arteries | 5 (0.031) | 3 (0.019) | 8 (0.025) |
| Pulmonary atresia | 4 (0.025) | 4 (0.025) | 8 (0.025) |
| Single ventricle | 4 (0.025) | 4 (0.025) | 8 (0.025) |
| Interrupted aortic arch | 3 (0.018) | 5 (0.032) | 8 (0.025) |
| Coarctation of aorta | 3 (0.018) | 2 (0.013) | 5 (0.016) |
| Complete atrioventricular septal defect | 2 (0.012) | 3 (0.019) | 5 (0.016) |
| Double-outlet right ventricle | 2 (0.012) | 2 (0.013) | 4 (0.012) |
| Double outlet of left ventricle | 2 (0.012) | 1 (0.006) | 3 (0.009) |
| Right aortic arch | 0 (0) | 2 (0.013) | 2 (0.006) |
| Mitral valve cleft | 0 (0) | 1 (0.006) | 1 (0.003) |
| Left ventricular outflow tract stenosis | 1 (0.006) | 0 (0) | 1 (0.003) |
| Aortopulmonary septal defect | 1 (0.006) | 0 (0) | 1 (0.003) |
| Double aortic arch | 0 (0) | 1 (0.006) | 1 (0.003) |
| Pulmonary artery sling | 1 (0.006) | 0 (0) | 1 (0.003) |
| Aortic arch stenosis | 0 (0) | 1 (0.006) | 1 (0.003) |
| Aortic stenosis | 1 (0.006) | 0 (0) | 1 (0.003) |
| Mitral valve malformation of aortic valve | 0 (0) | 1 (0.006) | 1 (0.003) |
| Tricuspid stenosis | 1 (0.006) | 0 (0) | 1 (0.003) |
| Absence of pulmonary artery | 1 (0.006) | 0 (0) | 1 (0.003) |
| Malformation of brachiocephalic artery | 1 (0.006) | 0 (0) | 1 (0.003) |
| Abnormality of pulmonary artery | 0 (0) | 1 (0.006) | 1 (0.003) |
a Values are expressed as No. (per 1,000 live births).
Cardiac murmurs were identified in 1.88% (6028/321447) of the newborns, of which 12.61% (760/6028) were confirmed as CHD. Abnormal POX detections were identified in 0.68% (2176/321447) of newborns, of which 16.91% (368/2176) were confirmed as CHD. In addition, 2.50% (8032/321447) of newborns were screened-positive by POX plus cardiac auscultation, of which 12.57% (1010/8032) were confirmed as CHD. The sensitivity of cardiac auscultation, POX, and two indicators’ combination for CHD detection were 69.15%, 33.49%, and 91.90%, respectively, and the specificity of them were 98.36%, 99.43%, and 97.81%, respectively. Values of different indicators for neonatal CHD detection are shown in Table 2.
| Screening Indicators | True Positives | False Positives | True Negatives | False Negatives | Sensitivity (%) (95%CL) | Specificity (%) (95%CL) | Youden Index |
|---|---|---|---|---|---|---|---|
| Cardiac auscultation | 760 | 5268 | 315080 | 339 | 69.15 (66.31-71.86) | 98.36 (98.31-98.40) | 0.68 |
| POX | 368 | 1808 | 318540 | 731 | 33.49 (30.71-36.37) | 99.43 (99.41-99.46) | 0.33 |
| Cardiac auscultation plus POX | 1010 | 7022 | 313326 | 89 | 91.90 (90.09-93.41) | 97.81 (97.76-97.86) | 0.90 |
There were 154 cases of children with major (serious and critical) CHD. At the initial screening, 36 cases were single positive in cardiac auscultation, 30 cases were single positive in POX, and 88 cases were both positive in the two screening indicators. Comparing the multiple groups showed that the ratio of both positive in two indicators in the children with major CHD at the initial screening was significantly higher than that of single positive in any indicator (χ2 = 59.455, P < 0.001) (Table 3).
| Screening Indicator | Major CHD, No. (%) |
|---|---|
| Simple positive in cardiac auscultation | 36 (30.85) |
| Simple positive in POX | 30 (22.34) |
| Both positive in 2 indicators | 88 (46.81) |
| χ2 | 59.455 |
| P-value | 0 |
All 33 cases of children with critical CHD were promptly treated with cardiac surgery. Also, 98 cases of children with serious CHD underwent cardiac surgery, and 23 cases of children with serious CHD underwent interventional therapy. There were 405 cases of children with significant CHD, out of who 212 cases underwent cardiac surgery, 103 cases underwent interventional therapy, and 90 cases accepted medical treatment or were followed up. Moreover, 540 cases of children with insignificant CHD were followed up, and 15 cases of children with major (serious and critical) CHD died from severe conditions. The standardized mortality rate of children aged 0 - 1 years with CHD was 4.67/100,000 (15/321,447), and the case fatality rate of major CHD was 9.74% (15/154).
5. Discussion
Through introducing and promoting this appropriate technology in our study, it was found that the prevalence of CHD was 3.419 per 1000 live births in Hainan, which was consistent with the result detected for Shaanxi province (8). It was also discovered that minor CHD was the main lesion in Hainan, and ASD (simple PFO was excluded in our protocol) was the most common type, with a prevalence of 1.313 per 1000 live births. Zhang X et investigated the birth defect monitoring system from 2014 to 2018 in Zhejiang, China, and also reported that minor CHD was the main lesion of children with CHD, and ASD was the most common type, while the average prevalence of major CHD was 1.6 per 1000 live births, which remained stable over time (9). However, some previous studies in other regions of China found that VSD was the most common CHD type (8, 10-12). ASD was the most common type in Hainan, which may have been due to the regional difference. According to the previous studies, the prevalence of CHD ranged from 1.5 to 16 per 1000 live births across various regions in China (8, 10-12). The differences were mainly due to the prevalence of minor CHD varying in regions, while the prevalence of major CHD remained stable (13). Contrary to the previous studies in China, our study conducted a prospective multicenter screening project in all participating institutions located in geographically diverse regions of Hainan in order to eliminate the bias. Our CHD screening protocol was proven to be economical, reliable, and efficient (11). From January 1, 2019, to December 31, 2021, the overall neonatal CHD screening rate in our study was as high as 97.59%, which indicated that this protocol was applicable for neonatal CHD screening in remote areas similar to Hainan.
Cardiac auscultation is one of the most important indicators for neonatal CHD screening. Song et al. screened 3327 newborns in Wenzhou city and determined that the sensitivity and specificity of murmur-alone for neonatal CHD detection were 17.3% and 99.7%, respectively (14). In our study, the sensitivity and specificity of murmur-alone for neonatal CHD detection were 69.15% and 98.36%, respectively. The sensitivity of murmur-alone for neonatal CHD detection was not extremely high, which may have been due to the following reasons: The pressure difference between the left and right heart in neonatal period is not obvious when there is a defect in the heart, the blood shunt between the left and right heart is not very large, or no high-speed turbulent blood flow exists, then the heart murmur is not obvious, atypical or inaudible.
POX is also one of the most important indicators for neonatal CHD screening. POX can be used to detect catheter-dependent types or other types of major CHD with hypoxemia (15). Hu et al screened 167190 newborns in 15 hospitals in Shanghai from July 1,2012 to December 31, 2014 and discovered that the sensitivity and specificity of POX-alone for neonatal detection were 44.3% and 99.9%, respectively (5). In 2017, a meta-analysis including 22 articles showed that the sensitivity and specificity of POX-alone for neonatal CHD detection were 69% and 99%, respectively (16); however, those in our study were 33.49% and 99.43%, respectively. The sensitivity of POX alone was relatively low in our study, which may have been attributed to the fact that minor CHD was the common type, without significant hypoxia.
According to our study results, the sensitivity may have been significantly improved by two indicators’ combination for CHD detection, while the specificity of two indicators’ combination was close to that of any single indicator. The sensitivity and specificity of two indicators’ combination for CHD detection were 91.90% and 97.81%, respectively, which were similar to those reported by Hu et al. (sensitivity = 93.7%, specificity = 98.3%) (5) and Song et al. (sensitivity = 89.9%, specificity = 94.7%) (14). In this study, the Youden index of two indicators’ combination for CHD detection was higher than that of any single indicator, suggesting a higher authenticity. At the initial screening, according to our study results, the ratio of both positive in two indicators in children with major CHD was significantly higher than that of single positive in any indicator, which was likely associated with severe hemodynamic abnormalities in major CHD. Therefore, it was recommended that extra attention should be paid to the newborns with both positive in two indicators at initial screening and that echocardiography examination should be assigned main priority.
During follow-up for the screened-negative children in this study, 89 cases of children were identified to have minor CHD. Children with minor CHD may have no significant cardiac murmur or hypoxemia, thus causing false negative screening, highlighting the importance of follow-up. In this study, all the children with major CHD underwent timely evaluation, and most of the children with significant CHD received timely treatment; only 15 cases died from severe conditions. From January 1, 2019 to December 31, 2021, the standardized mortality rate of children aged 0 - 1 years with CHD in Hainan was 4.67/100000. Previous studies had reported that 15969 children aged 0 - 1 years died from CHD in China from 2004 to 2018, and the standardized mortality rate of CHD dropped from 106.81/100000 to 38.70/100000 (17). The standardized mortality rate of children aged 0 - 1 years with CHD in Hainan was significantly lower than the above-mentioned rate. A related report determined that the case fatality rate of major CHD was as high as 27% due to the delayed diagnosis and treatment (18). The case fatality rate of children with major CHD in Hainan was 9.74% (15/154), which was also significantly lower. Therefore, the promotion of this project was conducive to timely diagnosis and treatment of children with CHD –those with major CHD, in particular – and to reduce the mortality.
In sum, the combination of two indicators (i.e., cardiac auscultation and POX) for neonatal CHD screening was found reliable as well as non-invasive, simple, and easy to operate; therefore, it was conducive for promotion. Introducing and promoting an appropriate technology system for screening, diagnosis, and evaluation of neonatal CHD were also found extremely significant for timely diagnosing and treating the children with CHD – those children with severe CHD, in particular.