1. Background
As a provincial-level tertiary pediatric hospital with 3,300,000 outpatient visits per year, the Emergency Department of the Children’s Hospital affiliated with Zhejiang University School of Medicine, Zhejiang, China, crowded with pediatric patients and their caregivers, is a daily sight. However, this setting is also where nosocomial infections can develop and often occur. Since the outbreak of coronavirus disease 2019 (COVID-19), the Children’s Hospital expanded the fever clinic to swiftly triage patients with fever, suspected cases of COVID-19, or other infectious diseases. Meanwhile, the medical staff of the aforementioned hospital was trained to improve the management of children’s visits, effectively preventing nosocomial infection (1-4).
The fever clinic triage system not only triages fever patients with a high risk of infectious diseases but also prioritizes those with emergency conditions. For example, as a common pediatric emergency, febrile convulsions are more common in children under 3 years. The clinical manifestations are localized or generalized tonic-clonic convulsions, often accompanied by disturbance of consciousness (5). When not managed in a timely manner, patients might experience central nervous system (CNS) damage and/or sequelae, aspiration pneumonia, other related adverse consequences, and even death, which are severely morbid to the children’s normal growth and development and life (6). Therefore, an effective triage system in a fever clinic is essential to rapidly screen high-risk patients based on the principles of priority treatment for the efficient allocation of limited healthcare resources and the best prognosis for patients (7).
This study reviewed the triage process of children in this fever clinic within 2019 - 2020 and the need for emergency care at the Children’s Hospital of Zhejiang University School of Medicine, Zhejiang, China. This study aimed to develop a scientific and accurate triage of children’s fever clinic by shortening the waiting time for consultation, providing timely and effective treatment, and reducing the incidence of disease complications, and improving the cure rate of children in a short time.
The Children’s Hospital’s experiences outlined herein could be helpful for other institutions or hospitals to avoid the collapse of the medical system during a pandemic.
2. Objectives
This study devised a procedure for triaging COVID-19 patients, which has been running efficiently in this hospital for 3 years. The process has been demonstrated to be successful in triaging patients affected by the recent influenza outbreak. In the future, this approach will be employed to combat further communicable diseases.
3. Methods
3.1. Pre-consultation Assessment and Triage of Children in Fever Clinic
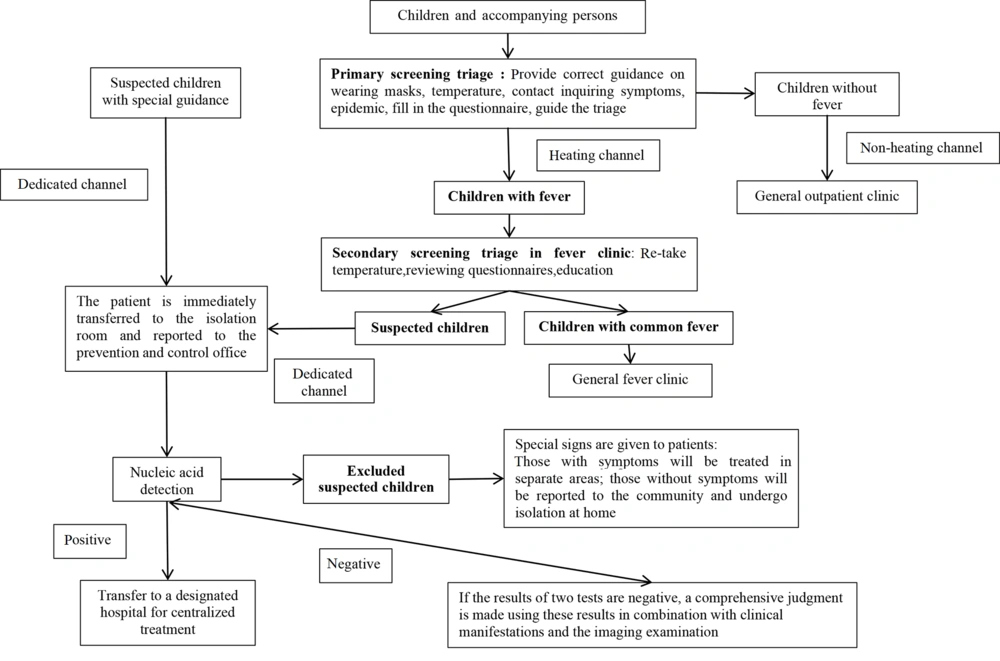
The specific triage procedures are described in this section (Figure 1). The fever clinic is located in a single, isolated three-story structure (called Public Health Emergency Building (PHEB)), which is separate from the inpatient and outpatient facilities. For patients with further acute conditions requiring rapid intervention, there is another emergency department in the outpatient facility. At the entrance to the first level of PHEB, a pre-consultation assessment/triage counter was set up. On the first level, nurses oversee triaging patients with fever, a history of close epidemiological contact, or emergency and rescue situations. Among the triage methods are temperature rechecking, vital sign assessment, severity evaluation, and inquiry into epidemiological contact history. These patients will be triaged on the second level following the pre-consultation assessment.
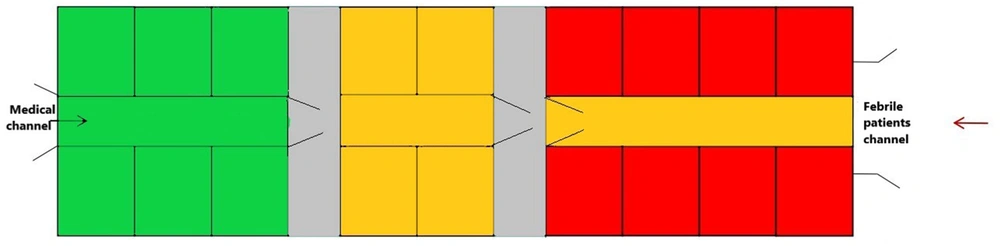
The second and third floors were separated into three areas, including the specialized isolation area, general fever clinic area, and emergency and rescue room. Each area was set up based on the principle of “three zones and two routes” (see below) to avoid cross-infection and contamination. Figure 2 depicts the layout of the fever clinic. Patients suspected of being infected will be triaged in a specific isolation area. This region is distinct from the other two sections with distinct routes; therefore, clean zone (green zone), potentially contaminated zone (yellow zone), and contaminated zones (red zone) were designated as “three zones and two routes”. Between the potentially contaminated zone and the contaminated zone, a buffer zone was established. The clean zone houses the staff restroom, toilet, shower room, and donning/doffing room. Potential contaminated areas include medical and nurse workstations, treatment rooms, and isolation wards.
Patients triaged in the general fever area can be examined and treated in this area because it comprises a nurse station, a laboratory, an imaging room, a pharmacy, and a patient’s toilet. The emergency and rescue room is set up for emergency patients with a fever.
The viral antigens adenovirus (ADV), influenza A virus (IAV), influenza B virus (IBV), and respiratory syncytial virus (RSV) were detected by the colloidal gold immunochromatography antigen test kits (KaiBiLi Respiratory Virus Antigen Detection Kit, Hangzhou Genesis Corporation, China). The results could be observed within 15 minutes.
Patients who attended the above-mentioned hospital for 6 months before and after using pre-consultation assessment and triage were selected for the study in two phases, namely July-December in 2019 and January-June in 2020. A total of 170 patients admitted from July to December 2019 were designated as the control group; however, 170 patients admitted from January to June 2020 were designated as the intervention group. The inclusion criteria were all enrolled children who had hyperthermia with tympanic temperature ≥ 38.5°C. All parents were informed about the study and completed appropriate consent forms. The exclusion criteria were children with hereditary or congenital diseases and children with intracranial infections and other related CNS diseases. The general data of children in the two groups were evenly distributed, and the differences were not statistically significant (P > 0.05).
Observation indices consisted of time to consultation, time to consultation and treatment, time to fever reduction, duration of hospitalization, incidence of adverse events, and satisfaction of the children in the two groups. Parents of the children were given a questionnaire drafted by the hospital, which included objective satisfaction on the waiting atmosphere, consultation order, waiting time, quality of care, and information communication, among other things. There were 10 elements as follows:
- Satisfaction with the hospital room, clinic, and meals
- Satisfaction with hospital staff, such as physicians, nurses, and other staff
- The quality of the provided treatment, such as waiting atmosphere, consultation order, waiting time, and quality of care
Each point is worth 10 scores, and the overall score was 100, with 80, 80 - 90, and > 90 points reflecting dissatisfaction, satisfaction, and great satisfaction, respectively. This study was approved by the Ethics Committee of the Children’s Hospital of Zhejiang University School of Medicine.
3.2. Statistical Analysis
The trend of prevalence and emergency medical needs of patients in fever clinics is described by gender, age, etiology, and season. The number and percentage were presented for categorical variables; nevertheless, the chi-square test was used to evaluate the significance of differences between the groups. All the analyses were performed using SPSS software (version 17.0). Two-sided P-values were reported throughout the study. A P-value less than 0.05 represented statistical significance.
4. Results
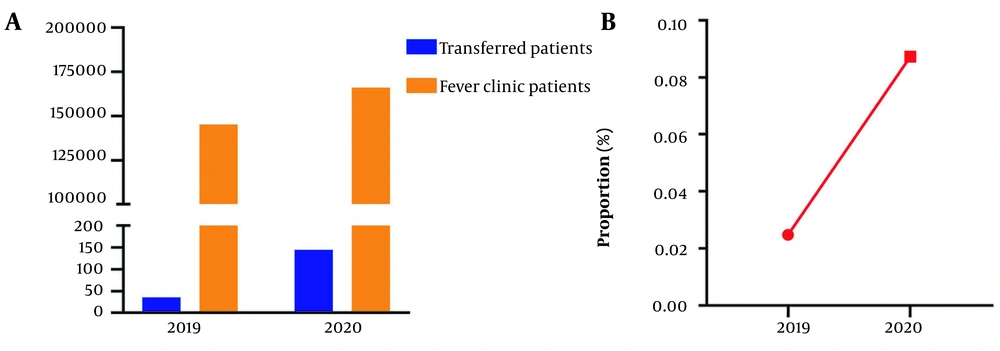
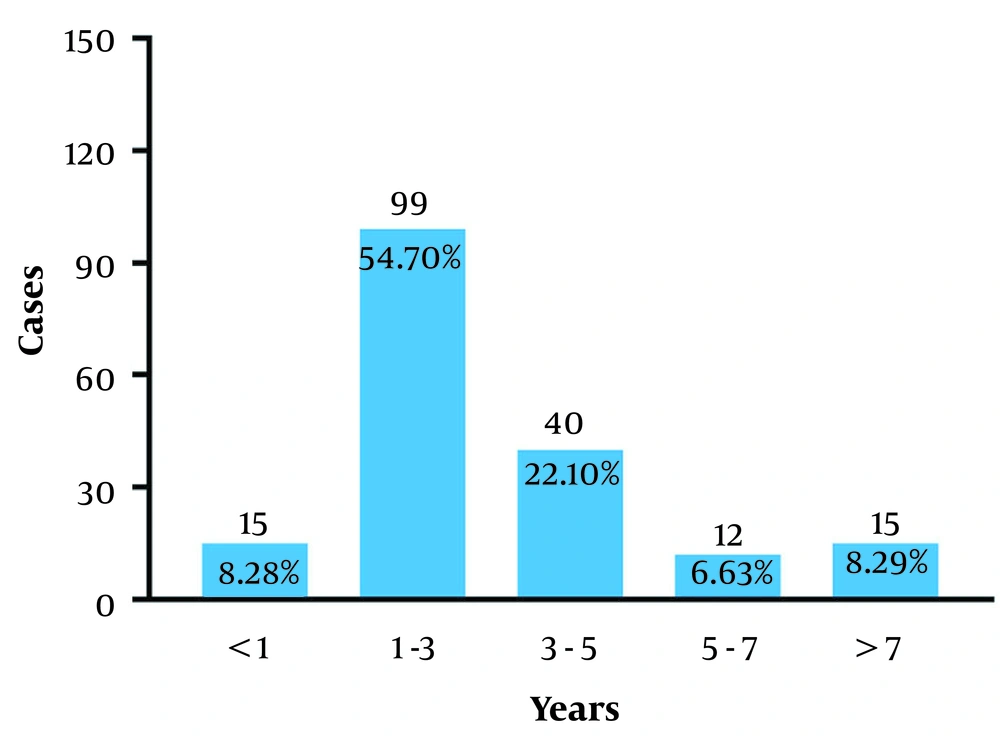
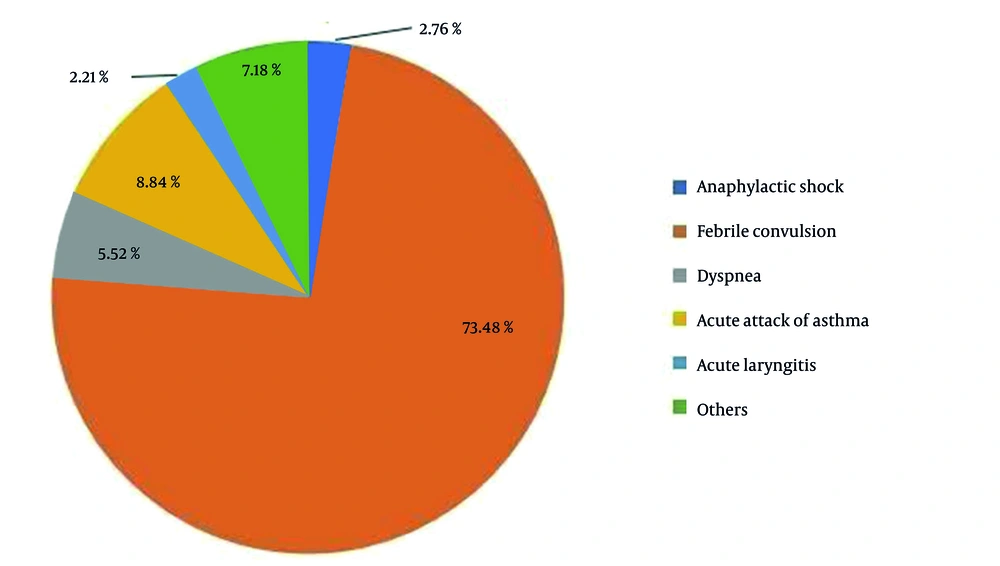
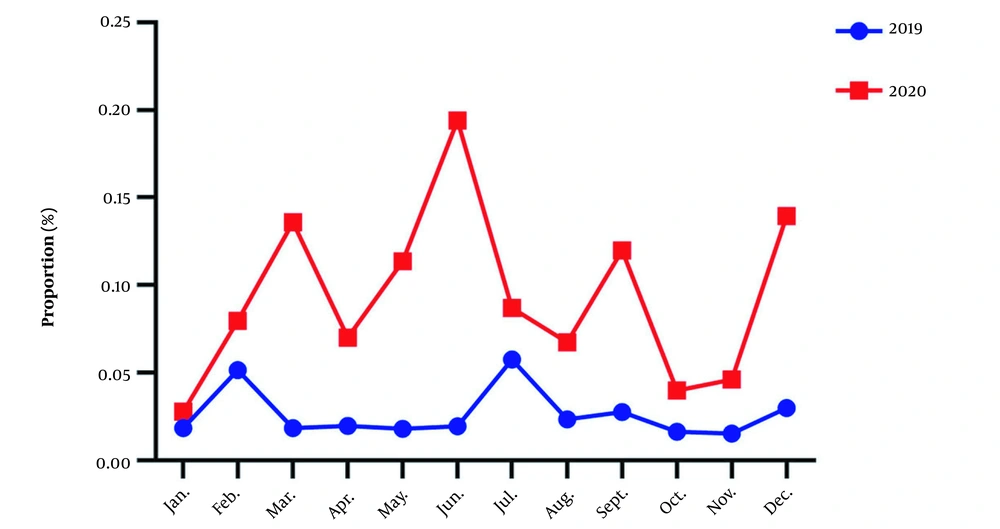
Fever outpatient visits increased from 145,271 in 2019 to 166,036 in 2020 (Figure 3A). In 2019, 36 (0.025%; 36/145,271) patients who visited the fever clinic required emergency care; the number increased remarkably by about four-fold to 145 (0.087%; 145/166,036) in 2020 (χ2 = 52.17; P < 0.001; Figure 3B). Among the 181 patients in both years who needed emergency care, 121 and 60 were male and female children, respectively. Figure 4 illustrates the proportion of children who needed emergency care during the period, 8.28% (15/181), 54.70% (99/181), 22.10% (40/181), 6.63% (12/181), and 8.29% (15/181) of whom were aged < 1, 1 - 3, 3 - 5, 5 - 7, and > 7 years, respectively. The most common disease requiring emergency care was febrile convulsions (73.48%; 100/181), followed by acute asthma attacks (8.84%; 16/181), dyspnea (5.52%; 10/181), anaphylactic shock (2.76%; 5/181), acute laryngitis (2.21%; 4/181), and other diseases (7.18%; 13/181) (Figure 5).
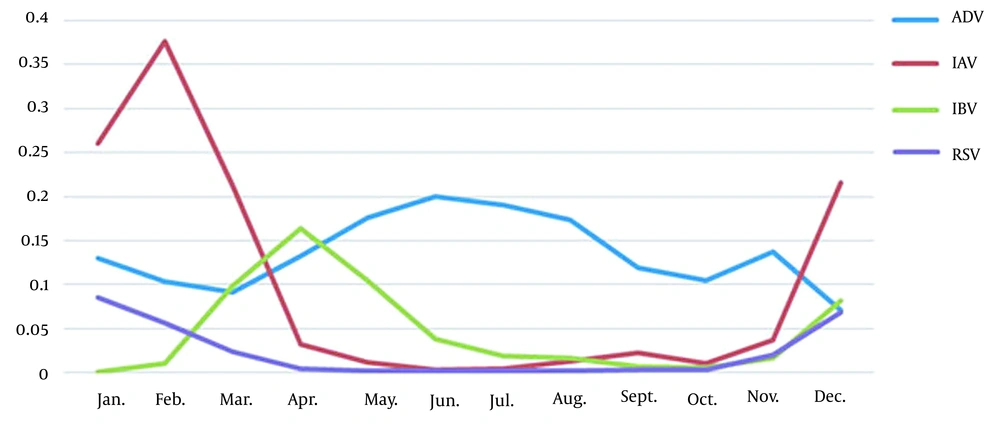
As shown in Figure 6, the proportion of children who needed to be sent to emergency care in 2020 was higher than in 2019. There were four epidemic peaks each year, namely February, July, September, and December in 2019 and March, June, September, and December in 2020. As shown in Figure 7, December to February were the peak seasons of IAV (1.6 - 37.7%), IBV (0.1 - 17.6%), and RSV (4.3 - 13.7%) infections, and June to July were the peak seasons of ADV (3.7 - 20.0%) epidemics.
Among all clinical indicators, time to consultation, time to diagnosis and treatment, time to fever reduction, and duration of hospitalization of the intervention group were all lower than the control group, and the differences were statistically significant (P < 0.001 for all indicators; Table 1). Moreover, 94.71% (161/170) of participants in the intervention group expressed satisfaction with the new nursing model, compared to 81.17% (138/170) in the control group. The difference was statistically significant (P < 0.05; Table 2).
| Groups | n | Clinic Time (h) | Diagnosis and Treatment Time (h) | Heat Reduction Time (h) | Hospital Stay (h) |
|---|---|---|---|---|---|
| Control group | 170 | 0.6 ± 0.2 | 3.8 ± 0.3 | 5.9 ± 1.4 | 10.7 ± 2.0 |
| Research group | 170 | 0.3 ± 0.1 | 1.3 ± 0.2 | 4.2 ± 1.3 | 6.2 ± 1.7 |
| P-value | 0.001 | 0.001 | 0.001 | 0.001 |
| Groups | n | Great Satisfaction | Satisfaction | Dissatisfaction | Degree of Satisfaction (%) |
|---|---|---|---|---|---|
| Control group | 170 | 87 | 51 | 32 | 81.17 |
| Research group | 170 | 134 | 27 | 9 | 94.71 |
Depending on their epidemiological history, febrile children were classified into common fever or suspected COVID-19. Children who were positive for a history of travel or contact with epidemic areas and had symptoms of dry cough, dyspnea, lymphopenia, and/or leukopenia were considered suspected of COVID-19. Despite advancements in contact tracing technology, epidemiological history is still an important basis for the early identification and diagnosis of children with COVID-19 infection. In the pre-consultation assessment and triage system, epidemiological history investigators should pay special attention to the investigation of parents’ epidemiological history and their children’s contact population, especially for school-age children whose classmates have a fever. To facilitate this issue, parents should be encouraged to actively declare if they suspect COVID-19 among their children through publicity and patient education. Additionally, it is advised to focus more on the investigation of family clustering, residential area (village) clustering, and their related family members (including children and their caregivers).
Children with suspected COVID-19 are immediately transferred to an isolation/observation room, and the COVID-19 prevention and control office of the hospital is notified. Then, the nurse will fill in the contact information and obtain signed informed consent from the patient’s caregiver. A routine physical examination, along with blood, urine, and stool routine, and other necessary tests are performed. Additionally, the patient’s body temperature is frequently monitored, and a lung X-ray can be included as part of a routine examination. However, lung computed tomography is not recommended and should not be performed on all suspected children due to the harmful nature of radiation exposure. At this stage, nurses provide life care and appropriate psychological counseling based on the child’s condition and self-care ability. Furthermore, the nurses also provided compassionate explanations and health education for the children to relieve the tension, anxiety, and unease caused by the isolation from their caregivers, chiefly their parents. If the patient’s consecutive nucleic acid test results are positive, they will be immediately reported to the COVID-19 epidemic prevention and control office of the hospital and the Hangzhou Center for Disease Control and Prevention, after which the patient will be transferred to a designated hospital for treatment. Patients negative for both nucleic acid tests and respiratory symptoms are treated in the green zone. The patients who tested negative but positive for respiratory symptoms will be kept as outpatients; they were housed in a separate area designated as the yellow zone. Figure 1 depicts the entire workflow.
5. Discussion
Emergency pre-examination and triage nurses can deliver health education to children and their parents who have a high temperature (3). The instruction of children and their parents with a high fever and hot convulsion-related knowledge makes parents aware that children in a hot state for an extended period can cause adverse events, such as heat convulsions, aspiration, or brain damage, to guide parents to deal with high fever measures, such as giving children physical cooling or oral antipyretic and sticking a cooling gel, with temperature control, to accelerate children’s recuperation (6).
In pediatric clinics or hospitals, viral infections of the respiratory tract are considered a prevalent condition. Fever, sore throat, cough, and other upper respiratory infection signs are pathognomonic. Infection with a respiratory virus is the most prevalent cause of fever among children. If children are not treated promptly and effectively, severe complications, such as acute asthma attacks, febrile convulsions, and systemic infections, might arise, endangering the children’s wellbeing and increasing the likelihood of medicolegal disputes, which is why rapid evaluation, diagnosis, and intervention is paramount.
Emergency pre-consultation assessment and triage nurses should deliver comprehensive health education to parents whose children have a high fever. Such information allows parents to be aware and alert of the potential devastating adverse events, such as heat convulsions, aspiration, and brain damage, that might occur in an extended febrile state and guides parents to actively administer temperature-lowering measures for their child, such as physical cooling (e.g., cooling gel pads and cold-water baths) and oral antipyretics (6).
According to the present study, the number of children who were admitted to this fever clinic in 2020 was greater than in 2019, although the number of pediatric patients with illness dropped owing to the hygiene and isolation strategies in place during the COVID-19 pandemic. The proportion of patients admitted to the emergency department was also much higher than in 2019, which increased four-fold in comparison. Patients requiring emergency treatment in the fever clinic were predominantly aged 1 - 3 years, followed by those aged 3 - 5 years, according to the current study. Among all emergency conditions, febrile convulsions were most prevalent, followed by acute asthma episodes, dyspnea, anaphylactic shock, and acute laryngitis. Furthermore, based on the present study, there were four peak infection periods in each year, namely February-March, June-July, September, and December. It was discovered that the peak seasons for IAV and IBV were December-February and March-May, respectively.
Most of the fever patients in the present study were infected with RSV. Over 95% of children had a history of infection with RSV by or before the age of 2 years, and they remain susceptible to life-long RSV reinfection despite partial immunity (8, 9). In infants under 6 months, RSV mainly causes bronchiolitis and pneumonia, which according to recent studies, might lead to non-atopic asthma as a sequela later in life (9).
The most distinctive feature of an influenza virus infection is that patients often present with rapid onset of symptoms and a high average body temperature. This seasonal influenza virus frequently induces upper respiratory infection symptoms, such as rhinitis, paranasal sinusitis, and pharyngitis, or in less but concerning situations, causes myocarditis and/or infiltrates the CNS via the transneural route, which can progress to encephalitis, meningitis, and other neurologic complications, resulting in a high fatality rate (10). The main strategies for dealing with the influenza virus are primary prevention and timely therapy.
On the other hand, ADV infection is also quite prevalent and commonly occurs in a co-infection setting with RSV, rhinovirus, or influenza virus, which must be detected using clinical and imaging criteria. There is currently no specific treatment for ADV infection. Management is supportive; virostatic agents, such as ribavirin and cidofovir, have very limited indications and are only considered in specific immunocompromised patients due to their associated risks of usage (11).
In pediatric clinics, viral respiratory tract infection is a prevalent and often occurring condition. Fever, throat discomfort, cough, and other clinical signs are common. If children are not treated promptly and effectively, significant consequences, such as acute asthma attacks, febrile convulsions, and systemic infection, might arise, endangering their safety and increasing the likelihood of medical disputes. Acute laryngitis in children is an acute inflammation of the laryngeal mucosa, primarily in the glottic region. It is common among children under the age of 5 years, especially in the winter and spring, due to some factors, such as delayed treatment or inadequate nursing. The disease’s progression poses a risk to children’s health and possibly life safety (12).
Children’s Hospital of Zhejiang University School of Medicine, as a provincial-level tertiary pediatrics hospital, has been designated as a dedicated treatment facility for pediatric COVID-19 patients since the outbreak. As the key facility for the treatment and provision of medical service at the frontmost position in the fight against the pandemic, the fever clinic of this hospital has formulated a series of adjustment measures in terms of the service process, pre-consultation assessment and triage, and treatment links, to safeguard the health of its medical personnel, patients, and the wider public and has been shown to be effective in curbing the spread of the nosocomial respiratory infections in the hospital, even in the post-pandemic era.
5.1. Conclusions
To minimize missed diagnoses of influenza patients, fever should not be used as a sole justification for pre-triage. However, it should be assessed in conjunction with clinical symptoms and epidemiological history. For the successful prevention and management of infectious diseases, new pre-consultation assessment indicators should be developed based on the features of infectious diseases in different seasons.