1. Background
Celiac disease (CD) is an autoimmune enteropathy characterized by sensitivity to gluten in genetically predisposed individuals, resulting in villous destruction and associated clinical manifestations (1). Currently, the asymptomatic ("non-classical") form of CD is more commonly encountered than those presenting with typical symptoms of malabsorption, weight loss, and steatorrhea. Since CD affects many systems, it can also present with endocrinological findings such as short stature, delayed puberty, and osteoporosis (2).
Individuals with CD are known to have osteoporosis, and especially in newly diagnosed patients, bone mineral density (BMD) has been shown to be lower than that of healthy controls (3). It was reported that normal BMD values are achieved within one year after diagnosis in diet-compliant patients (4). Inadequate bone mass accrual, particularly during adolescence, may increase the risk of osteoporotic fractures in adulthood (5). For this reason, it is very important to identify additional risk factors in pediatric celiac patients, follow them closely regarding bone health, and provide support if necessary.
2. Objectives
This study aimed to review BMD measurements in children with CD and determine additional risk factors predisposing them to osteoporosis.
3. Methods
The files of patients diagnosed with CD who were followed at the Pediatric Gastroenterology Outpatient Clinic 1 of Adana City Research and Training Hospital between 18.09.2017 and 30.09.2022 were reviewed retrospectively. Among them, 106 patients undergoing bone mineral densitometry (DEXA) measurements for osteoporosis screening were included in the study. The diagnosis of CD was based on the criteria from the 2012 European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee guidelines (6). The study was initiated after approval from the Adana City Training and Research Hospital Ethics Committee (no: 114/2204). The study was carried out in accordance with the Declaration of Helsinki. Patients aged 3 - 18 years without any comorbidities that may cause osteoporosis (osteogenesis imperfecta, metabolic disease, immobility, cerebral palsy) were included in the study. Bone mineral density measurements were obtained for all patients using the Lunar iDXA (GE Healthcare) system. Age- and sex-specific lumbar spine (L1-L4 vertebrae) Z-scores were calculated from the corresponding BMD values measured by DEXA using the program available at Bone Mineral Density website, taking into account Turkish reference values (6). In addition, sex- and height-specific femoral neck (FN) BMD Z-scores were calculated using the formula (SDS = child's value - population mean/standard deviations (SD)), again taking into account Turkish reference values. Also, BMD Z-scores calculated by the Lunar iDXA (GE Healthcare) system based on the United States (US) normal reference ranges by age and sex were noted.
Statistical package for social sciences (SPSS) software, version 26.0, was used for statistical analysis of the study data. Categorical measurements were summarized as numbers and percentages, and continuous measurements as mean and standard deviation or median and min-max where appropriate. The Kolmogorov-Smirnov test was used to check whether the parameters tested followed a normal distribution. When comparing continuous measurements between the groups, the independent samples t-test was used, assuming a normal distribution. The Pearson correlation test was used to determine relationships between continuous measurements. The statistical significance level was set at 0.05 for all tests.
4. Results
Of the 106 patients included in the study, 68 (64.2%) were female, and 38 (35.8%) were male. While the mean age of the patients was 10.2 ± 3.9 years, the mean age at diagnosis was 6.3 ± 3.6 years. The time since diagnosis was 3.7 ± 2.7 years. The mean height was 132.4 ± 22.1 cm, and the mean SDS for height-for-age was -0.96 ± 1.23. The patients had a mean body weight of 31.5 ± 16.7 kg, and the mean SDS weight-for-age was -1.12 ± 1.34. Laboratory data of the patients are presented in Table 1. Bone mineral density measurements of the patients and Z-scores adjusted for sex, age, and height are shown in Table 2.
| Mean ± SD | |
|---|---|
| Calcium (mg/dL) | 9.9 ± 0.9 |
| Phosphorus (mg/dL) | 4.6 ± 0.4 |
| Glucose (mg/dL) | 90.5 ± 31.6 |
| ALP (U/L) | 220.9 ± 76.1 |
| PTH (pg/mL) | 45.7 ± 19.4 |
| 25-OH-vitamin D (ng/mL) | 26.7 ± 8.8 |
| Somatomedin-C (IGF-1) | 149.2 ± 76.4 |
Laboratory Values of the Participants
| Mean ± SD | Median (Min-Max) | |
|---|---|---|
| L1-L4 (g/cm2) | 0.73 0 ± 0.197 | 670 (0.445 - 1.402) |
| FN (g/cm2) | 0.765 ± 0.192 | 0.726 (0.300 - 1.53) |
| L1-L4 Z-score (age) a | 1.28 ± 1.82 | 0.99 (-1.70 - 7.27) |
| L1-L4 Z-score (height) b | 1.54 ± 1.69 | 1.36 (-1.10 - 12) |
| FN Z-score (height) b | 2.05 ± 1.74 | 1.81 (-2.80 - 7.90) |
| L1-L4 Z-score (US) c | -0.65 ± 0.97 | -0.65 (-2.70 - 2.70) |
| FN Z-score (US) c | -0.31 ± 1.23 | -0.31 (-2.70 - 4.40) |
Bone Mineral Density Results of the Participants
A strong positive correlation (r = 0.729; P < 0.01) was found between the L1-L4 BMD Z-score by height (SDS value adjusted for sex and height) and the L1-L4 BMD Z-score by age (SDS adjusted for sex and age) in Turkish children. Bone mineral density Z-score values obtained with different calculations are shown in Table 3. Twenty-two (20.7%) patients had at least one prior fracture and/or bone pain. L1-L4 BMD values were significantly lower in patients with a prior fracture and/or bone pain compared to patients without a fracture and/or bone pain (0.822 ± 0.242 g/cm2 vs 0.706 ± 0.178 g/cm2, respectively; P = 0.047).
| r | L1-L4 (g/cm2) | FN (g/cm2) | L1-L4 Z-score (Height) a | L1-L4 Z-score (Age) b | L1-L4 Z-score (US) c | FN Z-score (Height) a | FN Z-score (US) c |
|---|---|---|---|---|---|---|---|
| L1-L4 (g/cm2) | 1 | 0.791 d | 0.499 d | 0.568 d | 0.448 d | 0.365 d | 0.279 d |
| FN (g/cm2) | 1 | 0.310 d | 0.428 d | 0.319 d | 0.658 d | 0.636 d | |
| L1-L4 Z- score (height) a | 1 | 0.729 d | 0.709 d | 0.549 d | 0.326 d | ||
| L1-L4 Z- score (age) b | 1 | 0.855 d | 0.451 d | 0.495 d | |||
| L1-L4 Z- score (US) c | 1 | 0.434 d | 0.573 d | ||||
| FN Z-score (height) a | 1 | 0.755 d | |||||
| FN Z-score (US) c | 1 |
Evaluation of the Relationship Between Variables
L1-L4 BMD Z-score (SDS adjusted for sex and height in Turkish children) was lower in patients with a BMI SDS value below -2 (moderately or severely malnourished) than in patients with a BMI SDS above -2 (mildly malnourished or normal) (0.02 ± 1.19 vs 1.4 ± 1.82, respectively; P = 0.014). Among subjects with short stature (height Z-score below -2 SD), L1-L4 BMD Z-score (SDS adjusted for sex and age in Turkish children) was significantly lower than those without short stature (0.46 ± 2.05 vs. 1.47 ± 1, respectively; P = 0.025). Disease duration and diet adherence were not correlated with any BMD measurements. A moderately strong positive correlation (r = 0.547; P < 0.01) was found between somatomedin-C (IGF-1) levels and L1-L4 BMD (g/cm2). A moderate negative correlation (r = -0.321; P < 0.001) was observed between blood phosphorus levels and L1-L4 BMD (g/cm2). Although no correlation was found between vitamin D levels and L1-L4 BMD (g/cm2) (P = 0.100), 25-OH-vitamin D levels below 30 ng/mL were found in 56 (52.8%) patients. Differences in vitamin D (25-OH-vitamin D) levels by sex (P = 0.100), age (P = 0.124), and time since diagnosis (P = 0.404) were not statistically significant.
In our study sample, the L1-L4 Z-score (SDS adjusted for age and sex in Turkish children) was 1.14 ± 1.62 in 36 (33.9%) patients, including 8 (7.5%) newly diagnosed patients and 28 (26.4%) patients in the first year of diagnosis versus 1.35 ± 1.92 in patients with time since diagnosis of more than one year. Still, the difference did not reach statistical significance (P = 0.56).
The prevalence of patients with low BMD varied according to the measurement method. It was remarkable that low BMD was not identified in any patients using L1-L4 Z-score by height and L1-L4 Z-score by age of Turkish children. Low BMD was detected in 1 patient (0.9%) using the femoral neck (FN) Z-score by the height of Turkish children. Nine (8.5%) patients were found to have low BMD using the US age- and sex-specific L1-L4 Z-score from the GE Healthcare Lunar iDXA system. However, low BMD was detected in 6 (5.7%) patients using the US FN Z-score from the GE Healthcare Lunar iDXA system.
5. Discussion
In our study, we found decreased L1-L4 Z-scores in CD patients with short stature or low BMI. Although a moderately strong positive correlation (r = 0.547; P < 0.01) was found between IGF-1 level and L1-L4 Z-scores, we could not demonstrate any relation between 25-OH-vitamin D levels and BMD scores. We found inconsistent results when interpreting BMD values for Turkish references.
Many adult patients with celiac disease have low BMD (3, 7). Low BMD results from many factors, such as malabsorption, hypocalcemia, vitamin D deficiency, secondary hyperparathyroidism, reduced physical activity due to fatigue, autoimmune effects, and inflammation (5). Another important cause of low BMD is the failure to reach sufficient peak bone density during childhood and adolescence. When peak bone mass is reached, suboptimal bone mineral accrual in the 20 s and 30 s may increase the risk of osteoporosis and fractures in later life (8). Osteoporosis occurs not only in CD but also in all other inflammatory diseases (9). Osteoclast activation due to elevations of several proinflammatory cytokines such as IL-1, tumor necrosis factor-alpha (TNF-α), IL-6, and IL-1β, increased bone resorption resulting from RANKL release by T cells, and increased osteoprotegerin antibodies have all been implicated in enhanced osteoporosis driven by inflammation (10, 11). In addition, these cytokines trigger muscle breakdown and show anorexigenic effects (12). Considering all these factors, it is important to ensure optimal BMD and eliminate osteoporosis causes in this patient group to prevent future complications.
In adult patients with CD, the prevalence of low BMD as measured by bone densitometry is variable. While the frequency ranges between 38% and 72% at the time of diagnosis, it decreases to 9% to 47% after adherence to a gluten-free diet (3, 13). In our study sample, the L1-L4 Z-score (SDS adjusted for age and sex in Turkish children) was 1.14 ± 1.62 in a total of 36 (33.9%) patients, including 8 (7.5%) newly diagnosed patients and 28 (26.4%) patients in the first year of diagnosis versus 1.35 ± 1.92 in patients with time since diagnosis of more than one year, but the difference did not reach statistical significance (P = 0.56). It was shown that while the frequency of fractures was more than 2-fold higher in symptomatic adult celiac patients compared to age- and sex-matched controls (47% and 15%, respectively) (14), the prevalence of fractures in patients with subclinical/silent celiac disease was not different from that of controls (15). We think that fewer fractures (7.5%; n = 8) were observed in our study due to the patients' short follow-up period and younger age (mean, 10.2 years).
The risk factors for low BMD that we found in this study are not specific to CD but are established risk factors for all children. It is known that low BMD occurs especially in malnourished patients due to low protein and calcium intake (16), and 10.3% (11 patients) of our patient group were moderately or severely malnourished, and 27.3% (29 patients) were mildly malnourished. In addition, the BMD values of children with short stature are lower than those of the same age and normal height. Short stature was identified in 18.8% (20 patients) of our patient group (17). Also, BMD values are lower in patients with delayed puberty (18). In our study, a moderate positive correlation (r = 0.547; P < 0.01) was found between somatomedin-C (IGF-1) and L1-L4 BMD (g/cm2) measurement, which can be explained by an increase in bone density due to the effect of increasing growth hormone with age (19). Additionally, a moderate negative correlation (r = -0.321; P < 0.001) was observed between blood phosphorus level and L1-L4 BMD (g/cm2), which can be attributed to the decrease in phosphorus level while bone density increases with age (20). Although no correlation was found between vitamin D level and L1-L4 BMD (g/cm2) (P = 0.100), 25-OH-vitamin D levels below 30 ng/mL were found in 56 (52.8%) patients. The endocrine society recommends maintaining vitamin D supplementation at 2 - 3 times the recommended dose to keep 25-OH-vitamin D levels above 30 ng/mL in patients at risk of osteoporosis (21). In this context, we would like to reemphasize the importance of providing vitamin D supplementation for our patients.
It is challenging to define osteoporosis in pediatric patients. According to the International Society for Clinical Densitometry (ISCD) criteria, low BMD is a BMD Z-score of 2 SD below the average value. The diagnosis of osteoporosis should not be solely made on the basis of densitometric criteria and requires both histories of a clinically significant, low-trauma fracture (two upper extremity fractures, a lower extremity fracture, or a vertebral fracture) and the presence of low BMD as demonstrated by a Z-score adjusted for age, sex, and height. Lumbar spine BMD is the most important indicator of total body BMD (22). Looking at both L1-L4 and FN measurements in our study, we found a strong positive correlation (r = 0.791; P < 0.01) between L1-L4 BMD (g/cm2) and FN BMD (g/cm2) values. Thus, we think FN values can also be considered in cases where the lumbar vertebrae cannot be evaluated.
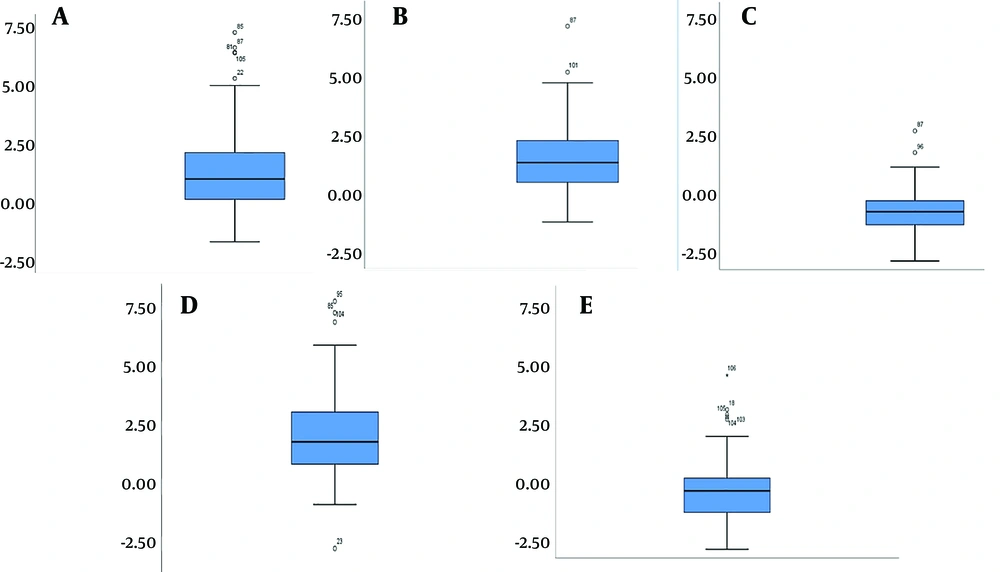
In another study from Erzurum, Turkey involving children with CD of similar age to our sample, the BMD Z-score was -1.23 ± 1.07, which was below the average as expected (23). In addition, the specifics of the bone densitometer (manufacturer, model) used by Volkan et al. (23) for BMD measurement in their patients were not provided. Interestingly, although we used the same reference values, the Z-scores of our patients were 1.28 ± 1.82 above the average, and low BMD was not detected in any of the patients. Comparing our results with previous reports, the high BMD values observed in the CD group were unexpected. Inconsistency among the data can be related to the use of QDR 4500A Fan Beam X-ray Bone Densitometer (Hologic, Bedford) by Goksen et al., where they collected data from 345 healthy children to establish Turkish reference values (6). The present study used the Lunar iDXA system (GE Healthcare). As such, discrepant data may have resulted from the use of a densitometer of another brand and model. Figure 1 shows how Z-scores calculated from the same values differ from each other. In order to prevent erroneous "normal" BMD reporting, the model of the device should be considered when interpreting BMD results. In case of inconsistency, the device's own normal range should be used.
Z-score results of bone mineral density (BMD) measurement of the subjects. A, lumbar vertebrae 1-4, SDS adjusted for sex and age in Turkish children; B, lumbar vertebrae 1-4, SDS adjusted for sex and height in Turkish children; C, lumbar vertebrae 1-4, United States normal range by age and sex from GE Healthcare Lunar iDXA measurements; D, femoral neck, SDS adjusted for sex and height in Turkish children; E, femoral neck, United States normal range by age and sex from GE Healthcare Lunar iDXA measurements.
5.1. Limitations
The limitations of our study include the lack of a control group, not measuring the participants' lean body mass, not evaluating their puberty stage, and not questioning their diet history and daily calcium and protein intakes.
5.2. Conclusions
In conclusion, considering the risk factors for suboptimal bone health in children and adolescents with celiac disease, malnutrition should be addressed, vitamin D supplementation provided based on vitamin D measurement, and all efforts should be made to prevent short stature. In addition, because of the risk of osteoporosis in these patients, BMD should be screened with bone densitometry. False "normal" BMD interpretations can be avoided by considering the model of the BMD measuring device and by using the device's normal ranges in case of inconsistency with the Turkish reference values.