1. Background
Electrodiagnostic (EDX) studies, including needle electromyography (EMG) and nerve conduction studies (NCS), are widely used in several neuromuscular disorders of children and adolescents. They can help physicians diagnose neuromuscular disorders, determine the injury severity and type in traumatic and non-traumatic injuries of neural plexuses and peripheral nerves, determine prognosis, and predict therapeutic response (1).
Physiological factors such as age, temperature, height, and gender affect nerve conduction velocity (NCV). Age and height are important factors affecting the NCS values (2). According to evidence, age can significantly affect nerve conduction characteristics. These age-specific differences are usually due to different nerve diameters, myelination, and body sizes of the patients (2, 3).
Nerve conduction velocity in neonates is half that of adults, while it reaches the adult-specific range at 3 - 5 years of age. Then, it stays at a constant level until the age of 25 - 30 years while decreasing at a rate of 1 - 3% each decade afterward (4, 5). There is also a negative relationship between age and nerve amplitude, possibly due to losing nerve fibers with age (6). Moreover, according to some studies, racial and geographical factors can affect these electrophysiological characteristics (7). Therefore, the normal NCS values are different in children compared to adults.
Furthermore, many laboratories have developed their own pediatric reference values when discussing NCS results. However, to the best of our knowledge, no study has ever investigated these characteristics in Iranian children. According to our previous experiences in clinical practice, the NCS parameters of Iranian children are slightly higher than the normal references reported by the studies in other countries. Moreover, Iranian children usually reach the normal NCS values of the adult population at younger ages.
2. Objectives
The present study aimed to investigate the normal NCS values in Iranian children of different ages.
3. Methods
The present descriptive cross-sectional study included 1,186 pediatric patients of Iranian nationality aged 7 days to 14 years. They were referred to the Electrodiagnosis Clinic of the Children's Medical Center, Tehran, Iran, after 2015, underwent an electrodiagnostic study, and had their NCS results in the normal range based on the references. The Ethics Committee of the Tehran University of Medical Sciences approved the study. Moreover, the patients or their parents gave written informed consent for their medical data to be published.
Since the EMG-NCV study is an invasive test, performing this analysis on healthy children would be unethical. Therefore, our sample did not consist of healthy children, but children had already been referred to the Electrodiagnosis Clinic of the Children's Medical Center for examination. All the patients underwent history taking and physical examination. The primary inclusion criteria were having Iranian parents, Iranian nationality, age between 7 days to 14 years when performing the EMG-NCV study, and absence of any neurological or neuromuscular disorder by history and examination. We excluded those that had or later developed any neuromuscular disorders or findings suggestive of lower motor neuron disorders, severe muscular atrophy due to disuse or surgical procedures, previous medical diseases (such as diabetes mellitus and thyroid disorders), extremity deformity, and significant muscular weakness due to peripheral nerve involvement (neuropathy).
The patients were divided into 8 age groups (7 days to one month, 1 - 3 months, 3 - 6 months, 6 - 12 months, 1 - 2 years, 2 - 4 years, 4 - 6 years, and 6 - 14 years). All groups were balanced in terms of sex and age. Then, the NCS was performed by a physical medicine and rehabilitation specialist and a pediatric neurologist experienced in pediatric EDX studies using a Nihon Kohden electromyogram (Tokyo, Japan). The data of the patients with NCS values in the normal range were included in the analysis. The criteria to determine normal values of NCS parameters were based on available normative data at the time of study in published literature (8, 9).
First, the temperature of the limb was assessed. The optimal temperatures for the lower and upper limbs were considered 30°C and 31 - 32°C, respectively (10). The limbs colder than this range were warmed using hot packs or thermal infrared lamps. Then, the NCS was performed when the limbs reached the optimal temperature.
The NCS parameters assessed for motor and sensory nerves included amplitude, conduction velocity, and F-wave latency. The motor nerve conduction values were recorded for the following nerves with corresponding muscles: The ulnar nerve using the abductor digiti minimi, the median nerve using the abductor pollicis brevis, the peroneal nerve using the extensor digitorum brevis, and tibial nerves using the abductor hallucis.
The amplitudes of the electrical responses evoked by distal stimulation sites were recorded in millivolts (mV) for all these motor nerves. Moreover, the conduction velocity was calculated as the distance between the distal and proximal stimulation sites divided by the latency difference and expressed in meters per second (m/s). Also, the stimulation sites of the upper limb included the wrist and elbow, while the ankle and popliteal fossa below the fibular head were used for lower limbs.
The sensory nerve conduction values were recorded for the following nerves with corresponding cutaneous areas using the mentioned methods: The median nerve on digit III (antidromic) and the medial plantar nerve (orthodromic). The base-to-peak amplitude at the distal stimulation site was recorded and expressed in microvolts (µV) for all these sensory nerves.
The frequency filters for motor nerve conduction studies were set at 2 HZ for the low pass and 20 kHz for the high pass, while the frequency filters for sensory nerve conduction studies were set at 30 Hz for the low pass and 3 kHz for the high pass. For motor NCS, the recording sweep speed was set to 2 ms/division, and the sensitivity was set to 5 mV/division. For sensory NCS, sweep speed and sensitivity were set to 2 ms/division and 20 µV/division, respectively. Also, the tibial and ulnar nerves were stimulated ten times on the ankle and wrist to record the F-wave latency, and the lowest latency was included in the analysis.
Data analysis was performed using SPSS version 22.0 and the chi-square test. A P-value < 0.05 was considered statistically significant. We also report parametric studies calculating the mean values and standard deviations for each nerve.
4. Results
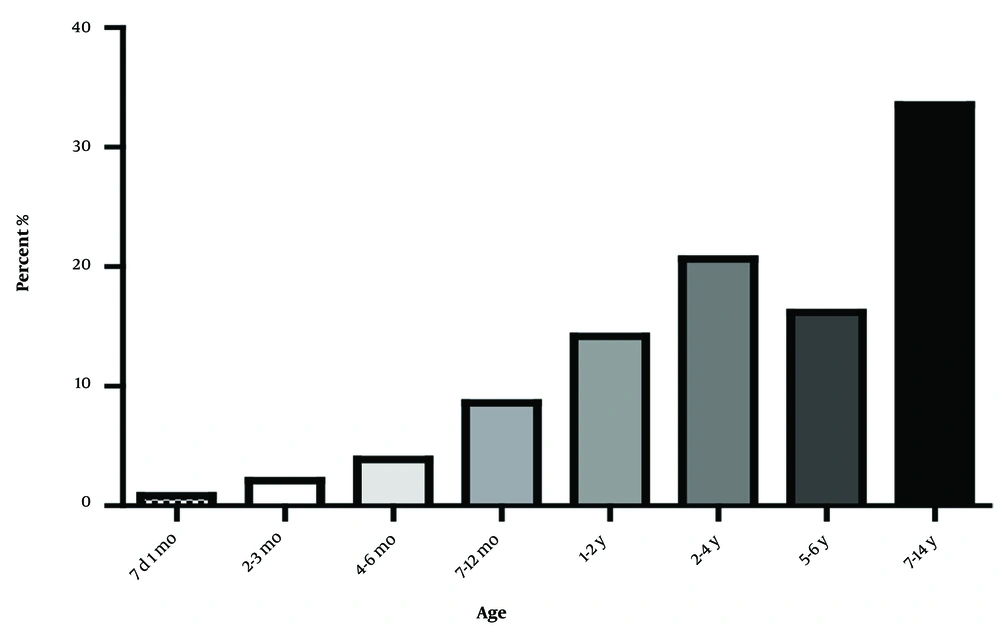
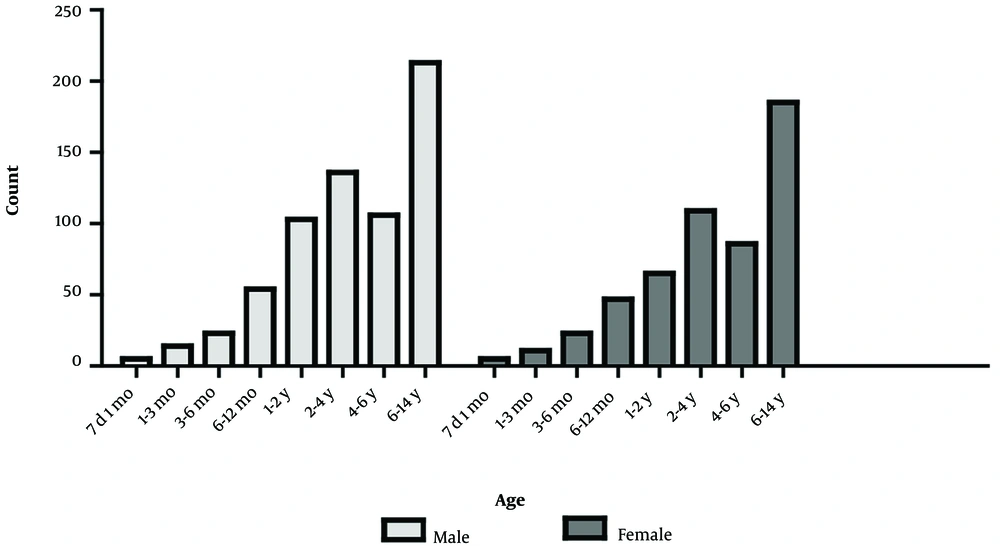
Most patients were 7 - 14 years old (Figure 1). Moreover, the numbers of female and male patients were almost the same in all age groups (Figure 2).
As presented in Table 1, the mean SNAP amplitude of the median nerve reached its peak in 6-month-old babies, while it was near the normal range of the adult population (8) in the age group of 7 days to one month (P < 0.001, F = 12.69). Also, the mean SNAP velocity of the median nerve was different in various age groups, reaching its highest value at 6-14 years of age (P < 0.001, F = 291.02).
| Age | Median Nerve | |
|---|---|---|
| Velocity | Amplitude | |
| 7 d - 1 mo | 26.4 ± 3.66 | 29.01 ± 6.86 |
| 1 - 3 mo | 28.50 ± 9.44 | 33.24 ± 9.66 |
| 3 - 6 mo | 33.99 ± 4.15 | 46.51 ± 16.77 |
| 6 - 12 mo | 40.76 ± 5.22 | 58.56 ± 19.46 |
| 1 - 2 y | 46.47 ± 5.78 | 55.46 ± 16.02 |
| 2 - 4 y | 49.65 ± 4.08 | 54.90 ± 16.89 |
| 4 - 6 y | 51.76 ± 3.44 | 49.92 ± 13.28 |
| 6 - 14 y | 54.38 ± 4.18 | 48.99 ± 14.07 |
| Total | 48.98 ± 7.84 | 51.57 ± 16.14 |
Amplitude and Velocity of Median Nerve in SNAP
According to Table 2, the mean CNAP amplitude of the medial plantar nerve showed an increasing trend (P < 0.001, F = 20.26), with a slope after 6 months of age due to increased cutaneous area and subcutaneous tissue. Also, the mean CNAP velocity significantly increased with age, reaching the normal range of the adult population at 1-2-years-old (P < 0.001, F = 1421.5).
| Age | Medial Plantar Nerve | |
|---|---|---|
| Velocity | Amplitude | |
| 7 d - 1 mo | 24.13 ± 1.98 | 11.06 ± 4.35 |
| 1 - 3 mo | 27.27 ± 2.95 | 16.92 ± 3.94 |
| 3 - 6 mo | 32.35 ± 4.07 | 21.08 ± 12.07 |
| 6 - 12 mo | 36.32 ± 4.18 | 26.31 ± 7.44 |
| 1 - 2 y | 41.82 ± 4.58 | 29.02 ± 7.98 |
| 2 - 4 y | 45.82 ± 3.82 | 30.77 ± 8.63 |
| 4 - 6 y | 47.39 ± 4.06 | 29.83 ± 7.87 |
| 6 - 14 y | 49.32 ± 5.31 | 25.81 ± 8.35 |
| Total | 45.11 ± 6.88 | 27.86 ± 8.80 |
Amplitude and Velocity of Medial Plantar Nerve in CNAP
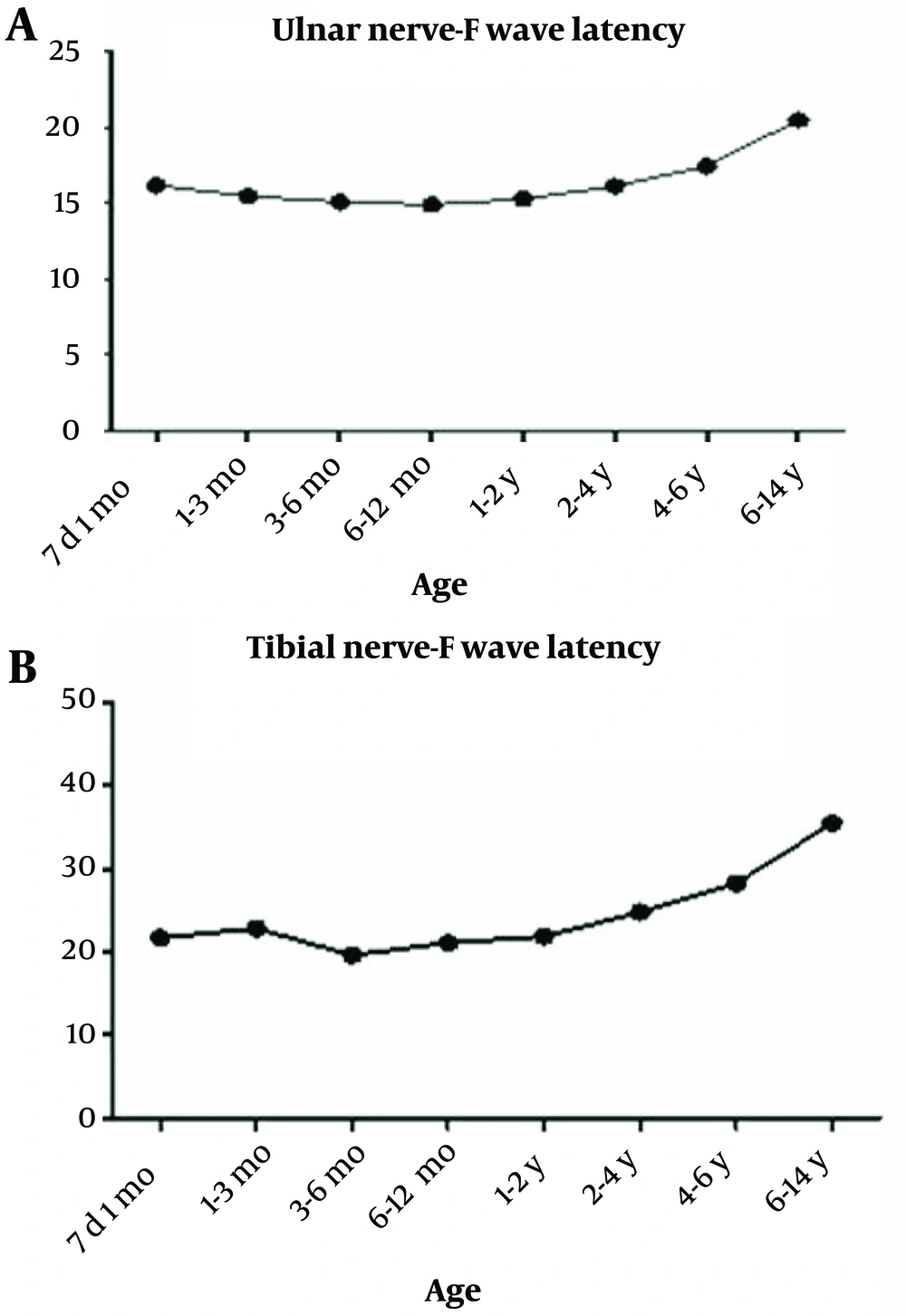
As shown in Figure 3, the mean F-wave latency of the ulnar nerve was significantly increased with age (P < 0.001, F = 240.6). However, it was lower than the normal range of the adult population. The same trend was observed for the F-wave latency of the tibial nerve (P < 0.001, F = 442.02).
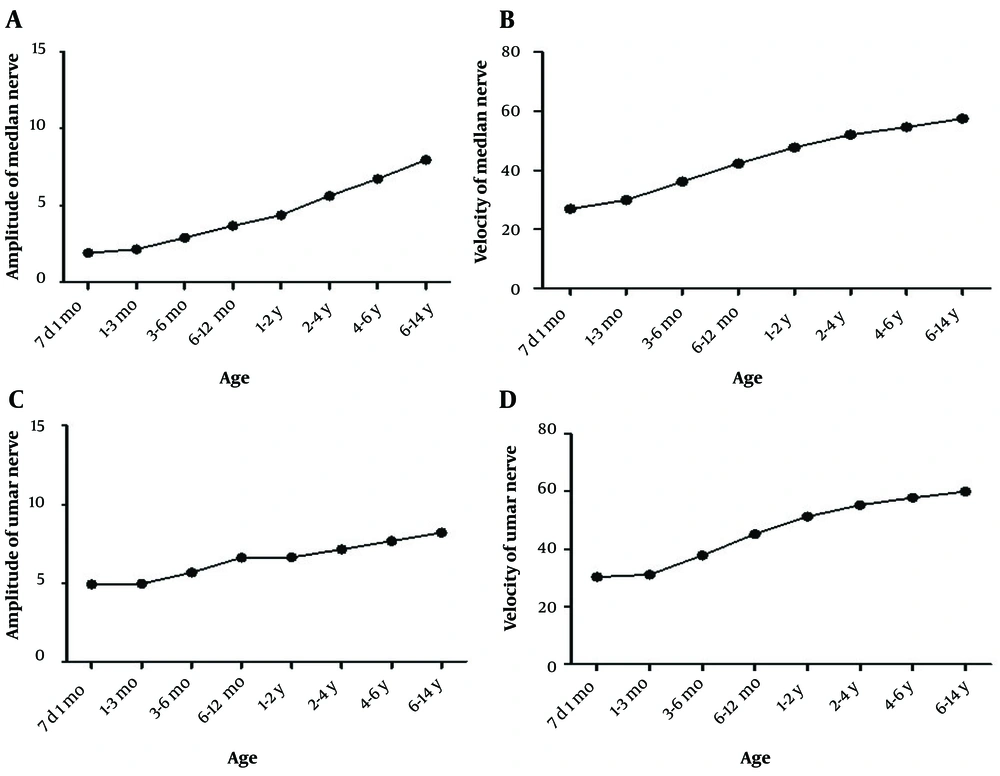
According to our findings, the mean CMAP amplitude of the median nerve significantly increased with age, reaching the normal range of the adult population at 2-4-years-old (Figure 4). Moreover, the mean CMAP velocity of the median nerve was significantly increased with age and reached the normal range of the adult population at 1-2-years-old (P < 0.001, F = 279.1). Also, the mean CMAP amplitude of the ulnar nerve significantly increased with age, reaching the normal range of the adult population at the age of 6-12 months (P < 0.001, F = 42.7), while the mean CMAP velocity of the ulnar nerve was significantly increased with age and reached the normal range of the adult population at 1-2 years of age (P < 0.001, F = 240.5).
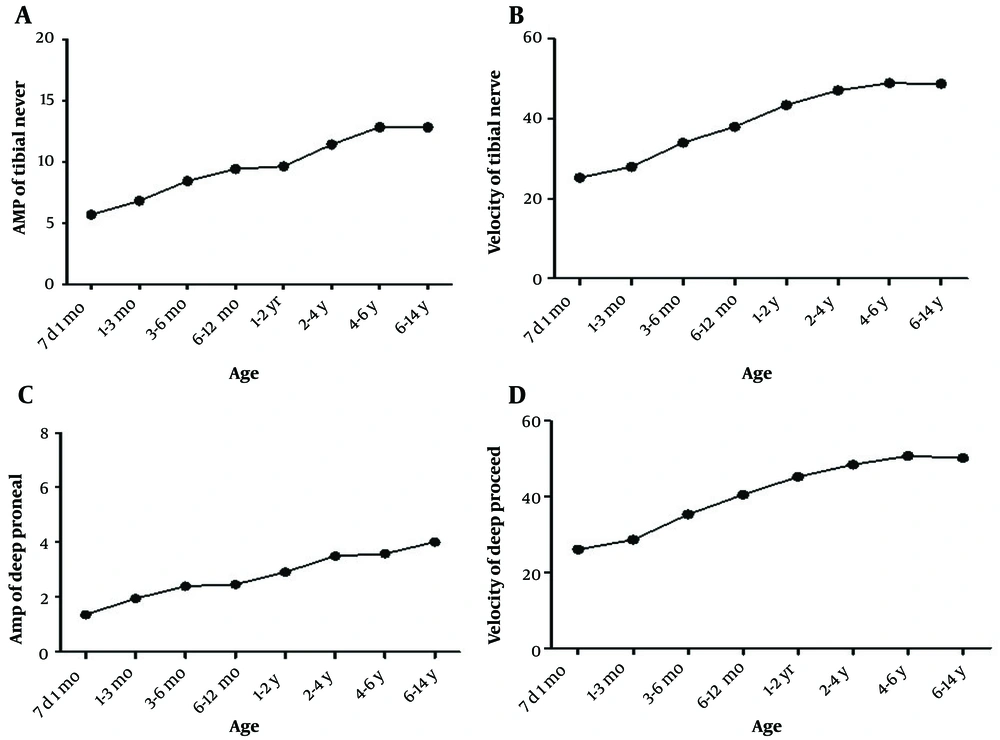
Finally, the mean CMAP amplitude of the tibial nerve showed a significantly increasing trend with age (P < 0.001, F = 51.1), reaching the normal range of the adult population at 3-6-months-old (Figure 5). Moreover, the mean CMAP velocity of the tibial nerve was significantly increased with age and reached the normal range of the adult population at 1-2-years-old (P < 0.001, F = 216.1). Also, the mean CMAP amplitude of the deep peroneal nerve significantly increased with age, reaching the normal range of the adult population at the age of 4 - 6 years (P < 0.001, F = 42.7), while the mean CMAP velocity of the deep peroneal nerve was significantly increased with age and reached the normal range of the adult population at 1-2 years of age (P < 0.001, F = 146.7).
5. Discussion
The NCS is routinely used for neurological assessment of children and adolescents. According to some studies, there are some age-related differences in NCS parameters, which can be attributed to different neural diameters and anthropometric characteristics in patients of different ages (2, 4). However, limited studies have investigated the normal ranges of NCS parameters in pediatric patients (11-17). Moreover, previous studies had some problems in determining the normal range of NCS parameters in pediatric patients. Some of these studies had small sample sizes, while some interpreted the measurements based on self-determined normal ranges without any explanation about the references of these values. Another problem was that the previous studies were usually confined to a specific racial group, such as European white children. Therefore, the present study was performed on a large sample size of 1,186 healthy children younger than 14 years, showing the significantly increasing trend of all NCS parameters with age.
Table 3 compares the present study findings with those of previous similar studies. As presented in this table, the amplitude of the median and medial plantar nerves showed an increasing trend with age, reaching the normal range of the adult population at 6 - 12 months and 2 - 4 years of age, respectively. The observed slope in the amplitude diagram of these nerves was probably due to the increased cutaneous area and subcutaneous tissue thickness after 6 months of age. Ryan et al. (12) reported that the amplitude of the median nerve reached the normal adult range at 2 - 4 years of age, while the normal adult values reported in the textbooks by Alexander et al. (9) and Dumitru et al. (8) were lower than those of the present study and Ryan et al.'s study (12). Also, the amplitude of the medial plantar nerve in the present study was lower than the values reported by Ryan et al. (12). In contrast, the amplitude values of the mentioned sensory nerves in the present study reached the normal range of adults in babies aged 7 days to one month, which was compatible with the findings by Ryan et al. (12). However, Alexander et al. (9) and Dumitru et al. (8) reported the age limit of 6 months for these amplitude values to reach the normal range.
| Present Study | Dumitru et al. | Alexander et al. (D2-W;D3-W) b | Ryan et al. | |
|---|---|---|---|---|
| Normal SNAP amplitude-median nerve | ||||
| 7 d to 1 mo | 29.01 ± 6.86 | 6.22 ± 1.30; | 6.22 ± 1.30; 4.86 ± 2.23 | 24 ± 7 |
| 1 - 3 mo | 33.24 ± 9.66 | 15.86 ± 5.18 | 16.74 ± 1.47 | 36 ± 12 |
| 3 - 6 mo | 46.51 ± 16.77 | 17.72 ± 3.35 | ||
| 6 - 12 mo | 58.56 ± 19.46 | 16.00 ± 5.18 | 16.00 ± 5.18; 17.55 ± 1.70; 9.00 ± 3.45 | 53 ± 20 |
| 1 - 2 y | 55.46 ± 16.02 | 24.00 ± 7.36 | 24.00 ± 7.36; 15.72 ± 4.50 | 54 ± 23 |
| 2 - 4 y | 54.90 ± 16.89 | 24.28 ± 5.49 | 24.28 ± 5.49; 12.02 ± 5.89 | 62 ± 24* |
| 4 - 6 y | 49.92 ± 13.28 | 25.12 ± 5.22 | 25.12 ± 5.22; 19.78 ± 4.21; 14.04 ± 5.99 | 54 ± 20** |
| 6 - 14 y | 48.99 ± 14.07 | 26.72 ± 9.43 | 26.72 ± 9.43; 20.50 ± 3.49 | 55 ± 19***; 50 ± 15**** |
| Normal CNAP amplitude-medial plantar nerve | ||||
| 7 d to 1 mo | 11.06 ± 4.35 | 10 ± 8 | ||
| 1 - 3 mo | 16.92 ± 3.94 | 21 ± 11 | ||
| 3 - 6 mo | 21.08 ± 12.07 | |||
| 6 - 12 mo | 26.31 ± 7.44 | 34 ± 15 | ||
| 1 - 2 y | 29.02 ± 7.98 | 32 ± 16 | ||
| 2 - 4 y | 30.77 ± 8.63 | 36 ± 18*; 42 ± 19** | ||
| 4 - 6 y | 29.83 ± 7.87 | 38 ± 17*** | ||
| 6 - 14 y | 25.81 ± 8.35 | 34 ± 16****; 27 ± 13***** | ||
| NCV of the median nerve in SNAP | ||||
| 7 d to 1 mo | 26.4 ± 3.66 | 22.31 ± 2.16 | 22.31 ± 2.16; 24.09 ± 2.6 | 26 ± 4 |
| 1 - 3 mo | 28.50 ± 9.44 | 35.52 ± 6.59 | 24.20 ± 3.51; 29.26 ± 4.14 | 38 ± 9 |
| 3 - 6 mo | 33.99 ± 4.15 | 29.91 ± 2.17 | ||
| 6 - 12 mo | 40.76 ± 5.22 | 40.31 ± 5.23 | 40.31 ± 5.23; 32.60 ± 3.15; 41.95 ± 2.68 | 48 ± 8 |
| 1 - 2 y | 46.47 ± 5.78 | 46.93 ± 5.03 | 46.93 ± 5.03; 45.12 ± 2.99 | 55 ± 6 |
| 2 - 4 y | 49.65 ± 4.08 | 49.51 ± 3.34 | 49.51 ± 3.34; 48.82 ± 3.02 | 59 ± 6* |
| 4 - 6 y | 51.76 ± 3.44 | 51.71 ± 5.16 | 51.71 ± 5.16; 41.04 ± 4.94; 50.72 ± 3.6 | 61 ± 5** |
| 6 - 14 y | 54.38 ± 4.18 | 53.84 ± 3.26 | 53.84 ± 3.26; 43.71 ± 3.37 | 64 ± 5***; 64 ± 4**** |
| F-wave latency of tibial nerve | ||||
| 7 d to 1 mo | 21.73 ± 2.02 | 23.92 ± 1.62 | ||
| 1 - 3 mo | 22.86 ± 3.19 | 28.59 ± 2.41 | ||
| 3 - 6 mo | 19.65 ± 4.29 | 23.93 ± 1.85 | ||
| 6 - 12 mo | 21.14 ± 2.07 | 23.78 ± 1.83; 22.0 ± 2.05 | ||
| 1 - 2 y | 21.90 ± 2.25 | 24.21 ± 1.63 | ||
| 2 - 4 y | 24.79 ± 2.98 | 25.6 ± 2.53 | ||
| 4 - 6 y | 28.28 ± 2.49 | 31.07 ± 3.10; 30.12 ± 2.52 | ||
| 6 - 14 y | 35.52 ± 5.04 | 36.32 ± 3.72; 32.78 ± 3.89 | ||
| F-wave latency of ulnar nerve | ||||
| 7 d to 1 mo | 16.17 ± 1.61 | 18.63 ± 1.6 | ||
| 1 - 3 mo | 15.46 ± 2.19 | 17.65 ± 1.39 | ||
| 3 - 6 mo | 15.08 ± 3.55 | 16.99 ± 1.28 | ||
| 6 - 12 mo | 14.89 ± 1.38 | 17.02 ± 1.45; 15.45 ± 1.37 | ||
| 1 - 2 y | 15.27 ± 1.25 | 15.67 ± 0.78 | ||
| 2 - 4 y | 16.12 ± 1.56 | 16.0 ± 1.41 | ||
| 4 - 6 y | 17.43 ± 1.44 | 18.51 ± 1.74; 18.25 ± 1.48 | ||
| 6 - 14 y | 20.47 ± 2.52 | 26.14 ± 3.03 | ||
| Amplitude of median nerve in CAMP | ||||
| 7 d to 1 mo | 1.92 ± 0.51 | 3.00 ± 0.31 | 3.00 ± 0.31; 1.27 ± 0.74 | 2.2 ± 1.6 |
| 1 - 3 mo | 2.16 ± 0.91 | 7.37 ± 3.24 | 7.37 ± 3.24; 2.37 ± 1.27 | 3.3 ± 0.8 |
| 3 - 6 mo | 2.91 ± 1.21 | |||
| 6 - 12 mo | 3.68 ± 1.39 | 7.67 ± 4.45 | 5.47 ± 2.01; 2.94 ± 1.17 | 5.9 ± 2.9 |
| 1 - 2 y | 4.38 ± 1.42 | 8.90 ± 3.61 | 8.90 ± 3.61; 4.12 ± 1.12 | 5.7 ± 1.9 |
| 2 - 4 y | 5.63 ± 1.81 | 9.55 ± 4.34 | 9.55 ± 4.34; 5.96 ± 2.01 | 7.2 ± 1.7* |
| 4 - 6 y | 6.73 ± 1.78 | 10.37 ± 3.66 | 10.37 ± 3.66; 6.49 ± 1.83 | 8.9 ± 3.3** |
| 6 - 14 y | 7.97 ± 3.11 | 12.37 ± 4.79 | 12.37 ± 3.66; 8.83 ± 1.87 | 10.9 ± 2.7*** |
| Amplitude of ulnar nerve in CAMP | ||||
| 7 d to 1 mo | 4.92 ± 1.23 | 1.88 ± 0.92 | 3.8 ± 1.6 | |
| 1 - 3 mo | 4.95 ± 0.94 | 3.11 ± 1.45 | 4.5 ± 1.9 | |
| 3 - 6 mo | 5.67 ± 1.33 | |||
| 6 - 12 mo | 6.61 ± 4.32 | 6.97 ± 1.89; 2.73 ± 1.09 | 5.4 ± 1.5 | |
| 1 - 2 y | 6.63 ± 1.63 | 4.55 ± 1.53 | 5.8 ± 1.8 | |
| 2 - 4 y | 7.14 ± 1.52 | 5.48 ± 1.42 | 6.2 ± 1.9*; 7.8 ± 1.9** | |
| 4 - 6 y | 7.67 ± 1.52 | 8.80 ± 2.35 | 7.2 ± 1.7*** | |
| 6 - 14 y | 8.20 ± 1.79 | 10.27 ± 2.02 | 9.2 ± 2.7****; 10.7 ± 2.4***** | |
| Amplitude of deep peroneal nerve in CAMP | ||||
| 7 d to 1 mo | 1.36 ± 0.52 | 3.06 ± 1.26 | 3.0 ± 1.26; 1.77 ± 0.62 | 2.1 ± 1.1 |
| 1 - 3 mo | 1.95 ± 1.12 | 5.23 ± 2.37 | 5.23 ± 2.37; 2.68 ± 1.04 | 2.8 ± 1.7 |
| 3 - 6 mo | 2.40 ± 1.18 | |||
| 6 - 12 mo | 2.47 ± 0.85 | 5.41 ± 2.01 | 5.86 ± 1.12; 2.64 ± 1.32 | 3.4 ± 1.2 |
| 1 - 2 y | 2.91 ± 1.13 | 5.80 ± 2.48 | 5.80 ± 2.48; 3.69 ± 1.27 | 3.7 ± 1.3 |
| 2 - 4 y | 3.50 ± 2.01 | 6.10 ± 2.99 | 6.10 ± 2.99; 4.25 ± 1.59 | 3.7 ± 1.5*; 4.4 ± 1.6** |
| 4 - 6 y | 3.58 ± 1.06 | 7.10 ± 4.76 | 7.10 ± 4.76; 3.78 ± 1.23 | 4.3 ± 1.8*** |
| 6 - 14 y | 4.01 ± 2.60 | 8.15 ± 4.19 | 8.15 ± 4.19; 7.22 ± 1.64 | 4.7 ± 1.6****; 5.4 ± 2.0***** |
| Amplitude of tibial nerve in CAMP | ||||
| 7 d to 1 mo | 5.68 ± 2.09 | 4.40 ± 1.73 | 5.3 ± 1.6 | |
| 1 - 3 mo | 6.81 ± 1.76 | 6.16 ± 2.44 | 9.5 ± 0.9 | |
| 3 - 6 mo | 8.42 ± 1.60 | |||
| 6 - 12 mo | 9.40 ± 2.06 | 14.06 ± 2.58; 6.83 ± 2.69 | 10.0 ± 2.8 | |
| 1 - 2 y | 9.62 ± 2.15 | 9.07 ± 2.12 | 11.1 ± 3.0 | |
| 2 - 4 y | 11.40 ± 2.81 | 9.57 ± 3.54 | 11.1 ± 3.1* | |
| 4 - 6 y | 12.82 ± 3.17 | 9.48 ± 2.39 | 13.6 ± 5.2** | |
| 6 - 14 y | 12.80 ± 3.28 | 15.75 ± 1.77 | 12.8 ± 3.8***; 11.8 ± 3.6**** | |
| MCV of median nerve | ||||
| 7 d to 1 mo | 26.9 ± 1.13 | 25.43 ± 3.84 | 25.43 ± 3.84; 26.17 ± 2.16 | 25 ± 3 |
| 1 - 3 mo | 29.92 ± 4.30 | 34.35 ± 6.61 | 32.3 ± 3.56 | 37 ± 9 |
| 3 - 6 mo | 36.17 ± 5.06 | 37.0 ± 4.38 | ||
| 6 - 12 mo | 42.32 ± 4.93 | 43.57 ± 4.78 | 42.3 ± 6.43; 43.91 ± 3.44 | 45 ± 13 |
| 1 - 2 y | 47.68 ± 4.60 | 48.23 ± 4.58 | 48.23 ± 4.58; 47.81 ± 2.33 | 47 ± 5 |
| 2 - 4 y | 52.04 ± 4.44 | 53.29 ± 5.29 | 53.59 ± 5.29; 52.71 ± 3.71 | 51 ± 6* |
| 4 - 6 y | 54.60 ± 4.56 | 56.26 ± 6.61 | 56.26 ± 4.61; 55.00 ± 5.20; 56.48 ± 2.36 | 56 ± 7** |
| 6 - 14 y | 57.47 ± 5.23 | 57.32 ± 3.35 | 57.2 ± 3.71; 57.32 ± 3.35 | 58 ± 4*** |
| MCV of ulnar nerve | ||||
| 7 d to 1 mo | 30.33 ± 3.50 | 25.03 ± 2.7 | 35 ± 7 | |
| 1 - 3 mo | 31.06 ± 2.97 | 35.1 ± 3.40 | 43 ± 7 | |
| 3 - 6 mo | 37.78 ± 4.61 | 40.5 ± 4.24 | ||
| 6 - 12 mo | 45.17 ± 5.56 | 47.2 ± 6.33; 45.02 ± 2.93 | 51 ± 7 | |
| 1 - 2 y | 51.26 ± 5.52 | 48.95 ± 2.46 | 53 ± 7 | |
| 2 - 4 y | 55.20 ± 5.37 | 54.19 ± 3.49 | 56 ± 6*; 58 ± 6** | |
| 4 - 6 y | 57.79 ± 4.61 | 56.9 ± 4.34; 56.51 ± 3.19 | 60 ± 6*** | |
| 6 - 14 y | 60.0 ± 5.90 | 58.3 ± 5.76 | 61 ± 6****; 62 ± 5***** | |
| MCV of deep peroneal nerve | ||||
| 7 d to 1 mo | 26.06 ± 1.42 | 22.43 ± 1.22 | 22.43 ± 1.22; 25.60 ± 3.68 | 31 ± 14 |
| 1 - 3 mo | 28.06 ± 1.42 | 35.18 ± 3.96 | 30.8 ± 2.91 | 41 ± 4 |
| 3 - 6 mo | 28.64 ± 3.51 | 36.1 ± 4.67 | ||
| 6 - 12 mo | 35.30 ± 5.27 | 43.55 ± 3.77 | 40.8 ± 6.16; 43.11 ± 4.13 | 44 ± 7 |
| 1 - 2 y | 45.28 ± 4.58 | 51.42 ± 3.02 | 51.42 ± 3.02; 47.43 ± 2.5 | 48 ± 8 |
| 2 - 4 y | 48.49 ± 4.38 | 55.73 ± 4.45 | 55.73 ± 4.45; 51.21 ± 3.95 | 49 ± 5*; 50 ± 5** |
| 4 - 6 y | 50.8 ± 4.42 | 56.14 ± 4.96 | 56.14 ± 4.96; 49.6 ± 4.98; 53.99 ± 3.74 | 50 ± 4*** |
| 6 - 14 y | 50.21 ± 4.37 | 57.05 ± 4.54 | 49.6 ± 3.40; 57.05 ± 4.54 | 52 ± 4****; 51 ± 5***** |
| MCV of tibial nerve | ||||
| 7 d to 1 mo | 25.23 ± 3.21 | 25.03 ± 1.96; 23.21 ± 2.79 | 24 ± 3 | |
| 1 - 3 mo | 27.95 ± 2.77 | 27.8 ± 3.89; 27.9 ± 2.27 | 40 ± 5 | |
| 3 - 6 mo | 33.97 ± 3.99 | 36.3 ± 4.98; 34.7 ± 2.92 | ||
| 6 - 12 mo | 37.98 ± 3.94 | 38.5 ± 5.50; 39.45 ± 4.29 | 41 ± 5 | |
| 1 - 2 y | 43.39 ± 3.94 | 42.6 ± 3.80; 42.42 ± 2.23 | 46 ± 4 | |
| 2 - 4 y | 47.08 ± 3.71 | 49.8 ± 5.78; 44.81 ± 1.91 | 51 ± 5* | |
| 4 - 6 y | 48.87 ± 3.36 | 50.0 ± 4.26; 48.6 ± 4.25; 48.43 ± 2.53 | 50 ± 6** | |
| 6 - 14 y | 48.72 ± 3.98 | 48.2 ± 2.76; 52.4 ± 4.19 | 52 ± 5***; 50 ± 4**** |
Comparison of the Results with Other Studies a
The sensory conduction velocities (SCVs) of nerves in the SNAP assessment are presented in Table 3. As shown, the SCV values of the median and medial plantar nerves in the present study were 50% and 60% of the normal range of adults, respectively. They reached the normal range at 2 - 4 and 1 - 2 years of age for the median and medial plantar nerves, respectively. Also, both nerves showed an increasing trend until 14 years of age. To the best of our knowledge, no previous study has investigated the mentioned parameter for the medial plantar nerve. However, our findings are compatible with those of Alexander et al. (9) and Dumitru et al. (8), while they are lower than the values reported by Ryan et al. (12).
According to Dumitru et al. (8), which used the ranges reported by Parano et al. (18), the SNAP assessments of the median and sural nerves reached the normal range of adults at 4 - 6 and 1 - 2 years of age, respectively. These findings are compatible with the present study, but the values reported by the present study for the median nerve reached the normal range later. Moreover, the results by Alexander et al.(9) are similar to those of Dumitru et al. (8), showing the increasing trend of SVC with age. Also, the puberty-related alterations for sensory orthodromic and motor antidromic conductions were similar, and the SNAP assessment values of the upper and lower limbs did not reach the lower limit of the normal adult range until 6 and 2 years of age, respectively. Furthermore, Ryan et al. (12) reported that the mentioned values reached the normal adult range at 2 years of age.
According to our findings, the normal values of F-wave latencies for ulnar and tibial nerves decreased with age from 1 to 6 months of age. Then, the values stayed constant until two years of age and showed an increasing trend afterward until 14 years of age. However, the F-wave latency of the ulnar nerve, but not that of the tibial nerve, did not reach the normal range of adults until 14 years of age. The values obtained in the present study are slightly lower than the normal values reported by Alexander et al. (9). Also, the F-wave latency values for the upper and lower limbs of the children younger than 6 years of age in our study were less than 20 and 30 milliseconds, respectively. According to Dumitru et al. (8), the mean F-wave latencies of the median and ulnar nerves were 15.3 and 14.6 milliseconds until 2.5 years of age, respectively. Then, they increased gradually to reach the normal values at 20 years of age. The F-wave latency stayed constant in the first 3 years of life due to a rapid increase in NCV and subsequent increase in arm length. Afterward, it showed an increasing trend due to the increasing arm length (19). The F-wave latency in children is biphasic. It is higher in neonates and children than in infants, which can be due to the opposite effects of increased height and myelination degree (19, 20). According to the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM), the increasing trend of F-wave latency from the first week of life until the age of 7 was only reported by one study. In contrast, 6 other studies reported no increase during infancy and a gradual increase in 1 - 3 years of age until adolescence due to the linear growth during childhood. The effect of height on the F-wave latency is higher than that of age. Therefore, height should be considered while interpreting the F-wave latency in adolescents with rapid growth (21).
The amplitude of the median, ulnar, deep peroneal, and tibial nerves showed a gradual increase from 7 days of age until 14 years of age, reaching the normal values of the adult population at 2 - 4 years, 12 months, 4 - 6 years, and 3 - 6 months of age, respectively. According to Dumitru et al. (8), the CMAP amplitude of the median nerve is 4 mv at one month of age and reaches 14.1 mv at 6 - 11 years of age, showing a 3-fold increase until 11 years of age. The increase is usually sharper in the first 6 months of life. Moreover, Alexander et al. (9) reported that the CAMP amplitudes of the lower and upper limbs in neonates were about 33 - 50% and 25%-33% of the normal range of adults. However, these values did not reach the adult range until 10. Also, Ryan et al. (12) reported that most nerves did not reach the normal range of adults until 2 - 3 years of age.
The amplitude of the median nerve reported in the present study is lower than the values reported by Dumitru et al. (8), which can be due to different calculation methods (base-to-peak method vs. peak-to-peak method). However, our results are compatible with those reported by Alexander et al. (9), who used the base-to-peak method, while they were lower than the values reported by Ryan et al. (12). For the ulnar nerve, the amplitude in our study was higher than in other reports. Moreover, we did not compare the present study results and those of Dumitru et al. (8) for assessing the deep peroneal nerve because different techniques were used. However, the present study findings are lower than those reported by Alexander (13\7) and Ryan et al. (12). Considering the tibial nerve, our results are compatible with the results of Ryan et al. (12) while higher than those reported by Alexander et al. (9).
On the other hand, the motor conduction velocity (MCV) had an increasing trend in all nerves with age. For the median and ulnar nerves, the MCV was 50% and 60% of the normal range of adults in children aged 7 days to 1 month, reaching the normal range at 1 - 2 years of age. For the tibial and deep peroneal nerves, it was 60% of the adult range and reached the normal range at 1 - 2 years of age. According to Dumitru et al. (8), the MCV of the ulnar nerve in CAMP assessment is 28 milliseconds (50% of the normal adult value), reaching the adult range at 3 - 5 years of age. Moreover, Alexander et al. (9) reported that MCV values of the upper and lower limbs were the same in the first year of life, while the values grew higher in the upper limb afterward. According to our results, the MCV values did not reach the adult range until age 2, which was compatible with those reported by Ryan et al. (12) and Alexander et al. (9).
The present study results showed that the NCS parameters in Iranian children are slightly different from the normal references reported by the studies in other countries. The SNAP and CMAP amplitudes and motor conduction velocity of these children usually reached the normal values of the adult population earlier.
This is the first study we know of that attempts to establish normative data for NCS in Iranian pediatric populations. We rigorously controlled technical factors and techniques in our study. Iranian electrodiagnostic laboratories can use this cutoff table to evaluate children suspected of neuromuscular disorders based on the large sample size and standard methodology of our study.
The present study also had some limitations, including selecting healthy Iranian children from a general pediatric hospital. Moreover, we only used the children referred to one healthcare facility, which can result in lower generalizability of the results. Also, we used a retrospective design for data collection in the present study due to the invasive procedure of EDX modalities and insufficient cooperation of pediatric patients. Finally, it is recommended to perform further studies in several centers and countries by using optimal sampling methods and considering the anthropometric variables. Such studies can provide us with more reliable findings that can be used for developing a comprehensive database for normal electrodiagnostic ranges in the pediatric population.