1. Background
The portal vein results from the connection of the splenic vein to the superior mesenteric vein behind the neck of the pancreas and is located in the hepatoduodenal ligament behind the Hepatic Artery (HA) and the joint bile duct (1, 2). The portal vein is created from joining of the splenic vein, inferior mesenteric vein, superior mesenteric vein, left gastric vein, and umbilical vein, supplies approximately 75% of the liver blood and delivers nutrients absorbed from the digestive system to the liver (3).
Dysfunction of anatomical and physiological characteristics of portal vein, such as the vein diameter, blood flow, and blood pressure, probably indicates liver diseases such as cirrhosis, varicose veins, and liver dysfunction (4). Full or partial obstruction of the portal vein (owing to infection, trauma, and malignancies), obstruction of intrahepatic branches of the portal vein (due to schistosomiasis, congenital fibrosis, primary biliary cirrhosis), sinusoidal obstruction syndrome (VOD) and cirrhosis, and obstruction of hepatic veins (Budd-Chiari syndrome) lead to portal vein blood flow in the opposite direction (hepatofugal) instead of moving toward the liver (hepatopetal), thereby increasing portal vein pressure (3, 5). In addition, the portal vein flow may be normal; however, it is qualitative and can quantitatively indicate portal hypertension or arteriovenous fistula (6); for example, a normal but very slow-velocity direction may indicate damage. Furthermore, measurement of PVD has high specificity for evaluating the blood pressure of portal vein and the hemodynamic status of portal circulation; however, it has low sensitivity (7). Hence, a more comprehensive evaluation should be conducted, including measurement of HA flow, Peak Systolic Velocity (PSV), End-diastolic Velocity (EDV), and Resistance Index (RI) to quantify the flow, velocity, and blood pressure of the portal vein leading to better diagnosis of liver disorders (8, 9). In addition to the indices, other characteristics such as liver parenchyma structure, hemostatic factors, and hepatosplenomegaly must be considered to interpret the results (10).
Abdominal ultrasound is a diagnostic method for imaging and evaluating abdominal, hepatic, and portal pathology. Abdominal ultrasound evaluates internal solid organs, bowel wall thickness, and ascites and has high precision. In such ultrasound, Doppler techniques measure blood flow, flow velocity (cm/s), and Arterial Blood Flow Waveform Shape (ABFWS), which play an important role in assessing portal hypertension (11, 12).
2. Objectives
Normal values of PVD and Doppler indices are affected by individuals' characteristics, such as age, gender, ethnicity, and other demographic characteristics (13, 14). Owing to the lack of study on determination of portal vein diameter and velocity in healthy children in Iran, the present study aimed to evaluate normal ranges of portal vein diameter and PSV in Iranian children aged 0 to 18 years and investigate their changes according to age and gender.
3. Methods
The present descriptive-analytical study examined PVD and PSV in healthy Iranian children. In this regard, 250 healthy children under the age of 18 were selected from whom were visited in Imaging Center of the Imam Khomeini Hospital in Tehran during 2018 and 2019 using the convenience sampling method. Children’s characteristics, including age and gender, were first recorded. Then individuals were classified into five age groups: Under one month, one month to 2 years, 2 - 6 years, 6 - 10 years, and 10 - 18 years, with an equal gender ratio. Moreover, 50 children were assigned to each group, including 25 boys and 25 girls.
The inclusion criteria were as follows: Not suffering from any acute or chronic disease, under 18 years of age, and consent to participate in the study. Participants who did not fast enough, patients with known hepatobiliary diseases, portal hypertension and splenomegaly, myeloproliferative disorders, cardiac and coagulation diseases, previous history of cholecystectomy or cardiac operation, hepatobiliary surgery or recent surgery for other reasons, and abnormal liver function tests were excluded from the study because their medical condition would alter the sonographic findings.
As mentioned above, all measurements were done in the fasting state, and the average fasting time depended on the age of the child. It was 2 hours in neonates (< 1 m), 2 - 4 hours for children aged 1 month to 2 years, 4 - 5 hours for children aged 2 – 6 years, 5 - 6 hours for children aged 6 – 10 years, and 6 - 8 hours for children aged 10 – 18 years.
The physical conditions of the child in terms of mobility and breathing are effective on the measurements; all the measurements were done when the child was completely calm. Before each exam, parents were told that their child did not have any significant physical activity within the last half hour. Also, the examination of the children who were crying was delayed until they returned to a stable position.
First, measurement of the main portal diameter was done by a radiologist blinded to the research subject. Using 5MHZ convex probe sonography, the patient was scanned in a supine and right anterior oblique position with the transducer in the RUQ of abdomen. The portal vein was accessed either through a subcostal approach with the transducer-directed posterior-cephalad or through the right intercostal approach with the transducer directed medially. Each of these views in which the diameter of the port was seen better would be considered.
The measurements were taken at the greatest anteroposterior diameter at the site where the hepatic artery crossed the portal vein. The diameter was taken by putting the two cursors in the internal wall of portal vein with exclusion of the echogenic wall (inner to inner).
Respecting variation of portal vein diameter with phases of respiration, an average of three times measurement was taken to minimize measurement errors. The exam was done with deep inspiration, deep expiration, and a quiet respiratory phase. The average of these three measurements was considered the mean diameter of portal vein. The measurements were repeated 30 minutes later, and the average of values in these two different times was considered as the final PVD.
In the next step, the Doppler ultrasound was performed by the radiologist following the instructions (Figures 1 and 2).
Regarding the important limitations of Doppler US, reproducibility, and accurate measurements, we needed to standardize the method. The transducer was oriented along the longitudinal axis of the main portal vein using a paramedian or slightly oblique plan during quiet inspiration by the same sonographer.
The portal vein flow velocity was measured three consecutive times to minimize intraobserver variability and avoid the influence of cardiac and respiratory fluctuations, and the mean value was recorded. The measurements were repeated 30 minutes later, and the final PSV entered in the calculations was the average of the measurements at these two different times.
The ultrasound scan head was inserted at a position where the maximum length of the tube was visible, and the angle of insonation was set between 55° and 60°. The sample volume was set in the middle of the portal vein trunk (where the laminar velocity is the fastest). The gate width was adjusted to two-thirds of the vessel's diameter to avoid wall artifacts. For each duplex scanning, the sample gate was adjusted at 6 - 10 mm (depending on diameter of the vessel) to obtain Doppler shift frequency spectra. The pulse repetition frequency was set at 4 kHz, and the wall filter was set at 100 Hz. Also, PSV (maximum blood flow velocity) was defined as peak systolic blood flow velocity in the central layer of the vessel. The measurements of color Doppler were done at the same place where the diameter was measured (at greatest anteroposterior diameter at the site where the hepatic artery crossed the portal vein). Eventually, the assistant radiologist recorded the results, including PVD and PSV. The PVD measurement scale was in millimeters, and the PSV scale was in centimeters per second.
The statistical data analysis was conducted using frequency percentages for qualitative variables and the mean and standard deviation for quantitative variables according to the Mann-Whitney, Kolmogorov-Smirnov, Kruskal-Wallis and wald chi-squared tests in SPSS 26. A significance level of 0.05 was considered in the present study.
4. Results
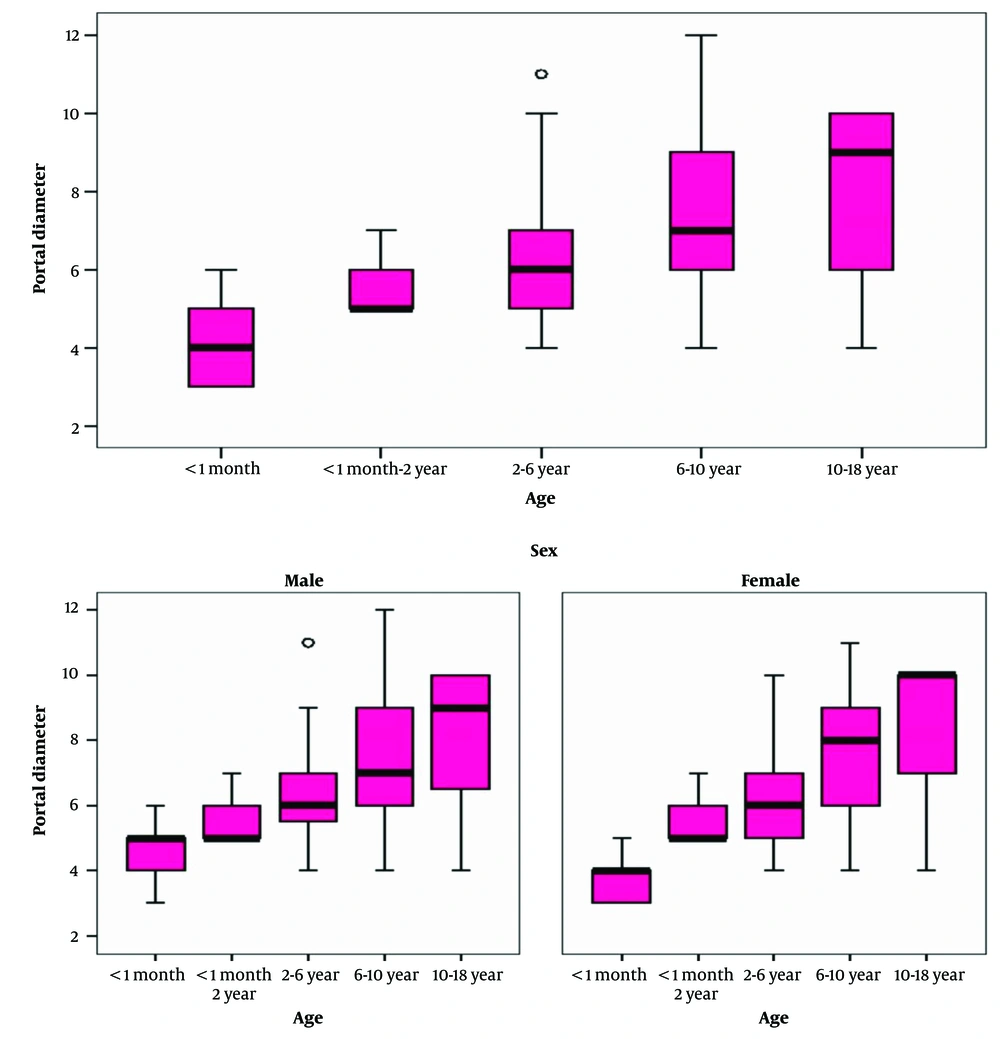
A total of 250 healthy children in five age groups were included in the study. The mean PVD was 6.34 mm in all children, 6.49 mm in boys, and 18.6 mm in girls. The mean PVD was equal to 4.08 mm in children under one month of age, 5.64 mm in one-month to 2-year-old children, 6.14 mm in 2 to 6-year-old children, 7.50 mm in 6 to 10-year-old children, and 8.32 mm in 10 to 18-year-old participants. In terms of gender, the mean PVD values were 4.46, 5.61, 6.25, 7.41, and 8.26 mm in boys and 3.73, 5.67, 6.04, 7.62, and 8.39 mm in girls, respectively. The Kruskal-Wallis test indicated a statistically significant difference between the mean PVD values of different age groups in all children, boys, and girls (P = 0.001), so the mean PVD increased with age (Table 1 and Figure 3). A detailed table with exact p-values is provided in Appendix 1 in the Supplementary File.
| Age | No. | Mean ± SD (mm) | P-Value a |
|---|---|---|---|
| All Children | 0.001 | ||
| <1 mo | 50 | 4.08 ± 0.80 | |
| 1 mo –2 y | 50 | 5.64 ± 0.80 | |
| 2 - 6 y | 50 | 6.14 ± 1.60 | |
| 6 - 10 y | 50 | 7.50 ± 1.90 | |
| 10 - 18 y | 50 | 8.32 ± 2.09 | |
| Total | 250 | 6.34 ± 2.12 | |
| Boys | 0.001 | ||
| <1 mo | 25 | 4.46 ± 0.77 | |
| 1 mo – 2 y | 25 | 5.61 ± 0.83 | |
| 2 - 6 y | 25 | 6.25 ± 1.62 | |
| 6 - 10 y | 25 | 7.41 ± 1.90 | |
| 10 - 18 y | 25 | 8.26 ± 2.12 | |
| Total | 125 | 6.49 ± 2.06 | |
| Girls | 0.001 | ||
| <1 mo | 25 | 3.73 ± 0.66 | |
| 1 mo – 2 y | 25 | 5.67 ± 0.78 | |
| 2 - 6 y | 25 | 6.04 ± 1.61 | |
| 6 - 10 y | 25 | 7.62 ± 1.96 | |
| 10 - 18 y | 25 | 8.39 ± 2.10 | |
| Total | 125 | 6.18 ± 2.19 |
a P-value less than 0.05 was considered statistically significant.
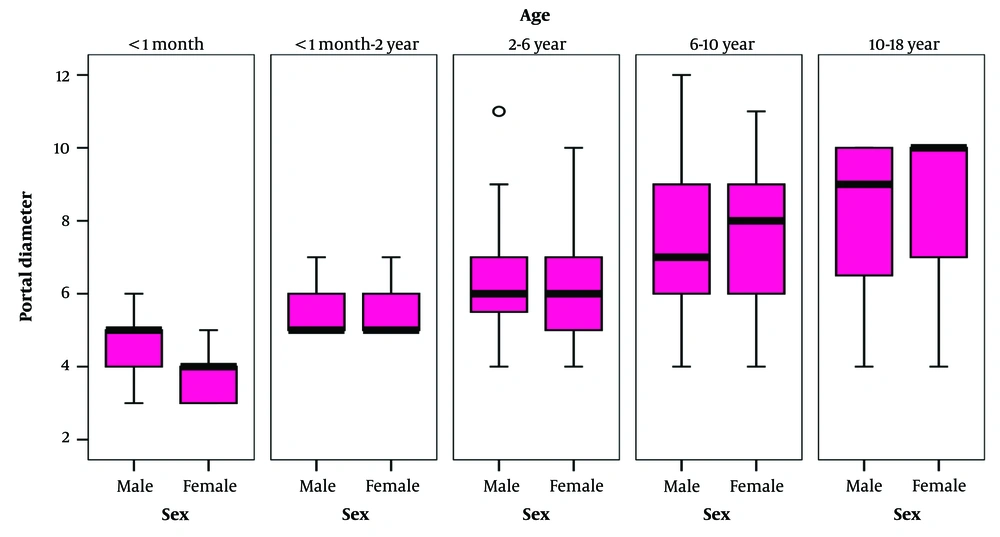
The comparison of meanPVD between age and gender groups indicated that it was higher in boys than in girls at the age group of under one month (P = 0.001); however, no statistically significant difference was found in other age groups (P = 0.18) (Table 1 and Figure 4).
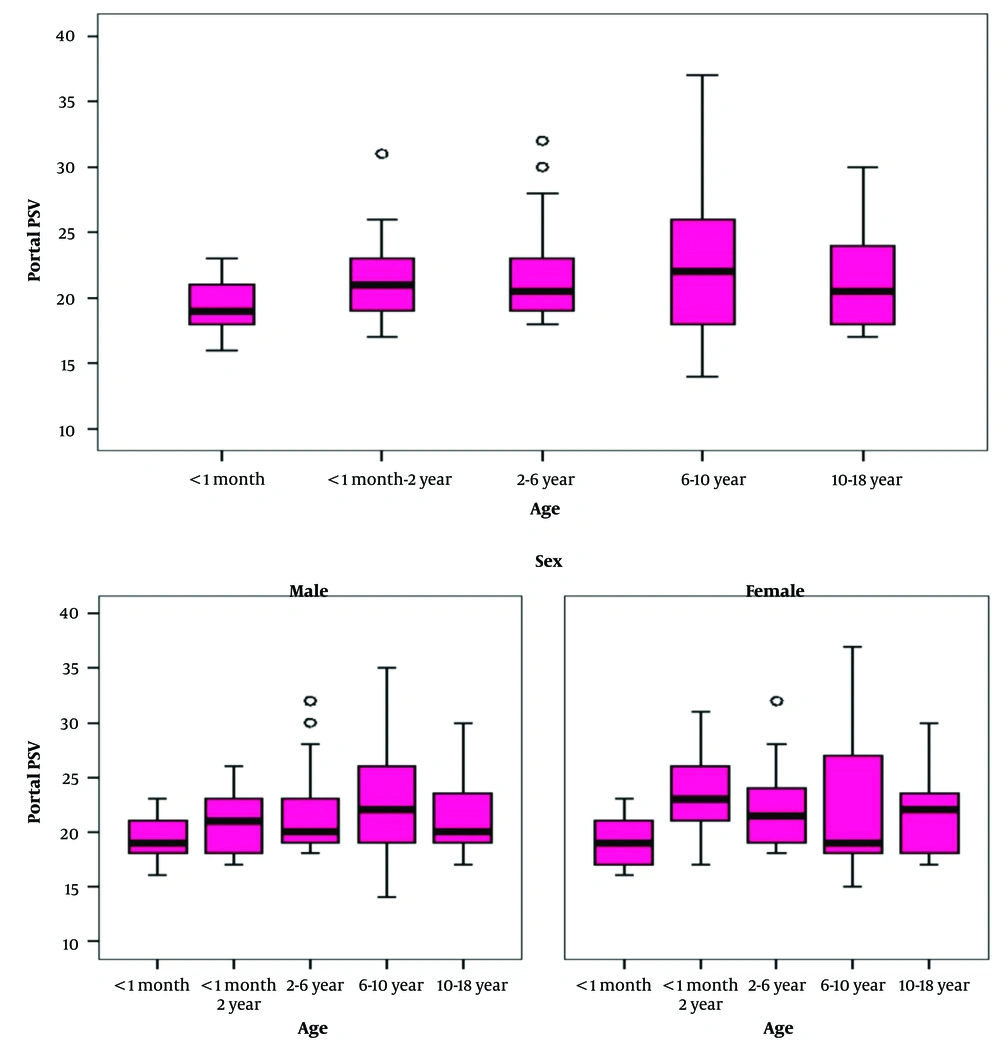
According to the results, the mean PSV values were 19.26, 22.20, 21.68, 22.86, and 21.48 cm/s in children under one month, one month to 2 years, 2 - 6 years, 6 - 10 years, and 10 - 18 years of age, respectively. The normal ranges were 15 to 23.7, 15 to 29.8, 15 to 29.1, 15 to 1.34, and 15 to 29 cm/s, respectively. The results of the Kruskal-Wallis test indicated a statistically significant difference in the mean PSV values of portal vein between different age groups (P = 0.001). In addition, the mean PSV of portal vein was different between different age groups, which was increased with increasing age (P = 0.01 and P = 0.003) (Table 2 and Figure 5).
| Age | No. | Mean ± SD (cm/s) | P-Value a |
|---|---|---|---|
| All children | 0.001 | ||
| <1 mo | 50 | 19.26 ± 2.25 | |
| 1 mo –2 y | 50 | 22.20 ± 3.78 | |
| 2 - 6 y | 50 | 21.68 ± 3.73 | |
| 6 - 10 y | 50 | 22.86 ± 5.61 | |
| 10 - 18 y | 50 | 21.48 ± 3.75 | |
| Total | 250 | 21.50 ± 4.12 | |
| Boys | 0.01 | ||
| <1 mo | 25 | 19.17 ± 2.14 | |
| 1 mo – 2 y | 25 | 20.61 ± 2.91 | |
| 2 - 6 y | 25 | 21.63 ± 3.99 | |
| 6 - 10 y | 25 | 23.28 ± 5.28 | |
| 10 - 18 y | 25 | 21.67 ± 3.77 | |
| Total | 125 | 21.36 ± 4.03 | |
| Girls | 0.003 | ||
| <1 mo | 25 | 19.35 ± 2.39 | |
| 1 mo – 2 y | 25 | 23.56 ± 3.94 | |
| 2 - 6 y | 25 | 21.73 ± 3.55 | |
| 6 - 10 y | 25 | 22.29 ± 6.13 | |
| 10 - 18 y | 25 | 21.26 ± 3.81 | |
| Total | 125 | 21.63 ± 4.23 |
a P-value less than 0.05 was considered statistically significant.
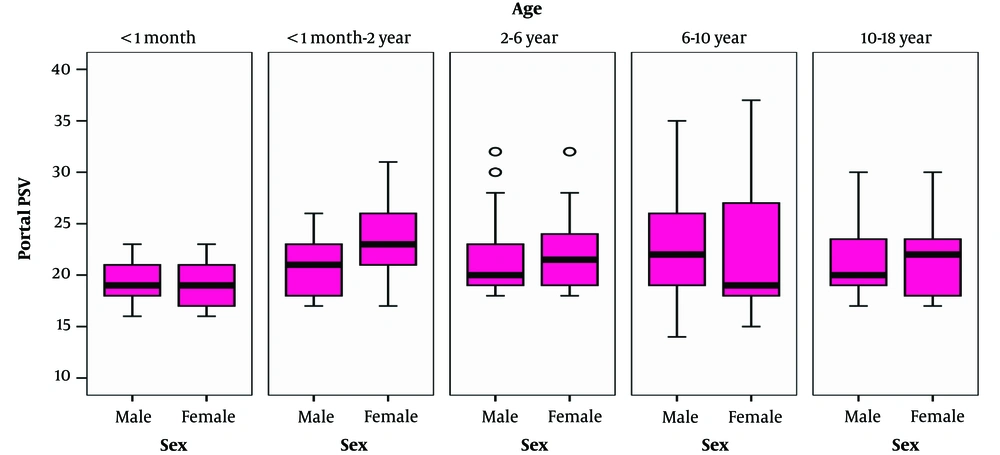
The difference in the mean PSV of portal vein in each age group in terms of gender indicated that the mean PSV was higher in girls in the age group of one month to two years (P = 0.007); however, no statistically significant difference was found in other age groups (P > 0.05) (Table 2 and Figure 6).
To examine the effect of confounders on the model, we performed a multiple linear regression model. We adjusted for the sex variable, and this difference remained significant. The results are summarized in Tables 3 and 4.
4.1. For Diameter
| Source | Type III | ||
|---|---|---|---|
| Wald chi-Square | df | P-Value | |
| Intercept | 4309.955 | 1 | < 0.001 |
| Age | 232.004 | 4 | < 0.001 |
| Sex | 0.326 | 1 | 0.568 |
a Dependent variable: Portal diameter; Model: intercept, age, sex.
By entering the gender confounder into the regression model, the age variable remained significant. In other words, the effect of the sex variable in the regression model was not significant.
In a more detailed examination of age groups, it was found that all age groups were significant before and after entering the confounder (Table 3).
4.2. For Peak Systolic Velocity
| Source | Type III | ||
|---|---|---|---|
| Wald chi-Square | df | P-Value | |
| Intercept | 7477.285 | 1 | < 0.001 |
| Age | 24.172 | 4 | < 0.001 |
| Sex | 0.555 | 1 | 0.456 |
a Dependent variable: Portal PSV; Model: Intercept, age, sex.
By entering the sex confounder into the regression model, the age variable remained significant. In other words, the effect of the sex variable in the regression model was not significant. In a more detailed examination of age groups, it was found that the significance of age groups did not change significantly with addition of confounders to the regression model.
As a result, by entering the sex confounder into the regression model, there was still a significant difference between the age groups (Table 4).
5. Discussion
According to the results of the present study, the mean was 4.08 mm in children under one month, 5.64 mm in one-month to 2-year-old children, 6.14 mm in 2 to 6-year-old children, 7.50 mm in 6 to 10-year-old children, and 8.32 mm in 10 to 18-year-old children. In terms of gender, the mean values were 4.46, 5.61, 6.25, 7.41, and 8.26 mm in boys and 3.73, 5.67, 6.04, 7.62, and 8.39 mm in girls, respectively. In one study by Ghosh et al. in India, the PVD values were 3.35 mm in children under one month, 3.85 in 1 to 3-month-old children, 4.08 mm in 3 to 6-month-old children, 4.34 mm in 6 to 12-month-old individuals. Also measured values were 4.75 mm in 1 to 2-year-old children, 5.19 mm in 2 to 4-year-old children, 5.95 mm in 4 to 6-year-old children, 6.03 mm in 6 to 8-year-old children, 7.22 mm in 8 to 10-year-old children, and 7.67 mm in 10 to 12-year-old participants. Also, they were 3.29, 3.87, 4.08, 4.43, 4.82, 5.18, 5.89, 6.07, 7.21, and 7.72 mm in boys and 3.48, 3.83, 4.09, 4.21, 4.65, 5.21, 5.99, 5.98, 7.22, and 7.63 mm in girls, respectively. In this study, the mean PVD increased with age in Indian children; however, no difference was found between the mean PVD values in terms of gender in each age group, which is consistent with our study. In this study, the mean PVD was slightly lower in Indian children than in Iranian pediatric population; however, no significant difference was found between them based on different age groups (13). In Turkey, Soyupak et al. reported the mean PVD values of 4.68, 6.56, 7.84, and 8.83mm in 0 - 12, 13 - 60, and 61 to 120-month-old, and over 121 months of age children, respectively; also, they were 4.82, 6.73, 7.77, and 9.19 mm in boys and 4.40, 6.27, 7.89, and 8.42 mm in girls, respectively. In this study, the mean PVD increased with age; however, no statistically significant difference was found between the two genders (14), which is in line with our study.
Patriquin et al. also investigated the normal diameter of portal vein in children. Their results showed a linear relationship between the diameter of portal vein and age. The average diameter of the portal vein was 3 - 5 mm at birth, 4 - 8 mm at one year old, 6 - 8 mm at 5 years old, 6 - 9 mm at 10 years old, and 7 - 11 mm at 15 years old (15). In their study, no significant difference was detected between the two genders in the same age groups. The results of their studies are consistent with ours.
According to the findings of present study, the portal vein mean PSV values were 19.26, 22.20, 21.68, 22.86, and 21.48 cm/s in children under one month, one month to 2 years, 2 - 6 years, 6 - 10 years, and 10 - 18 years of age, respectively. The main goal of our study was to investigate sonographic indicators among the "healthy" pediatric population. As mentioned earlier, PSV indicates the blood flow velocity in portal vein. This velocity decreases in people with hepatic diseases such as cirrhosis, and the velocity and presence of a disorder can be examined using a Doppler ultrasound. Sugimoto et al. found that the mean PSV was much lower in individuals with liver cirrhosis and those with hepatic diseases than in healthy individuals (16). Rokni Yazdi and Sotoudeh investigated the diagnostic accuracy of portal vein parameters for liver cirrhosis and found that the mean PSV was lower in individuals with hepatic cirrhosis than in healthy people. The sensitivity, specificity, and diagnostic accuracy of PSV were also greater than 95% (17). Kagimoto et al. demonstrated that the mean PSV changed with age (18).
Among the studies that investigated these parameters in cirrhotic children, we can refer to the study by Tuney et al. that diagnosed cirrhosis in children based on Doppler ultrasound results and its correlation with histopathological findings. According to their study, the PSV of portal vein was 62 cm/s in normal children, 40 cm/s in children with chronic active hepatitis, and 34 cm/s in cirrhotic children, and the differences were statistically significant. Also, the mean velocity of portal vein was 34 cm/s in normal children, 24 cm/s in children with chronic active hepatitis, and 18 cm/s in cirrhotic children. The results showed that if the average velocity of portal vein is below 20 cm/s, it can be an indicator for cirrhosis diagnosis (19).
According to the study of Gorka et al., the average velocity of portal vein was 20.8 cm/s in patients with early cirrhosis, 15.1 cm/s in patients with established cirrhosis, 30.8 cm/s in patients without cirrhosis in pathology, and 31 cm/s in the control group. They showed that a decrease in the speed of portal vein was directly related to the severity of cirrhosis, and this relationship was statistically significant in patients with established cirrhosis (20).
Riahinezhad et al. found that the mean PVD was statistically different between the two groups (8.3 ± 2.5 mm in cirrhotics vs. 5.9 ± 1.8 mm in controls) (21). The average velocity of the portal vein was 15.03 cm/s in the cirrhotic population and 16.47 cm/s in the control group. The results of their studies showed that measurement of portal vein parameters, such as speed and diameter, can be a good indicator in diagnosing cirrhosis and esophageal varices in children. It was also found that mean PVD increased with children's age; however, no significant difference was found between the two genders, being consistent with the results of other study.
In this article, we tried to examine the ultrasound parameters in main portal vein in the pediatric population. Few articles have analyzed the ultrasound parameters in other vascular structures, such as portal branches or hepatic arteries. Verhagen et al. examined the PSV of main portal vein and PSV and RI of the hepatic artery in children aged 0 - 17 years. According to the results of their study, PSV of the portal vein has no significant relationship with age, which is inconsistent with the results of our study, but PSV and RI of the hepatic artery increase significantly with age (22).
Vocke et al. assessed sonographic parameters in the portal vein and its branches in pediatric population. The results showed that diameter of the main portal vein and its branches increased significantly with increase in the patient's age and weight (23). Regarding the relationship between PDV and age, the results are congruent with our study.
Chau et al. examined the diameter, length, and cross-sectional area of the portal vein and its right and left branches in pediatric and adult populations, where the average diameters of left and right branches of the portal vein were 8.27 mm and 8.33 mm, respectively. The results of their study showed that diameter of the main portal vein was significantly greater in the adult population than in children. This was also the only article we could find that examined and compared diameter of the portal vein in other modalities (CT scan and MRI) among the pediatric population. According to their results, PVD measured by CT scan modality (13.28 mm) was significantly higher than that measured by MRI (10.5 mm) and ultrasound (9.81 mm) methods (24).
Generally, few studies have determined the mean PSV in children worldwide. Thus, the present study examined and determined the mean PSV in Iranian children and proposed that it could be used as a scale to investigate changes in PSV and diagnosis of hepatic disorders. Results of the present study revealed that the mean PSV changed with age.
In almost all of our studied age groups, the values of PSV and portal vein diameter were not significantly different between the two genders, and this was consistent with previous studies. Only two exceptions were observed: One in boys with the age group of less than one month, in which PVD was higher than in girls, and another in girls with the age group of one month to two years, in which the mean PSV was higher than in boys.
The difference observed only in these two age ranges is probably due to the small sample size and problems such as sampling bias. It is hoped that future studies with larger sample sizes, more idealized randomized sampling, and more complex statistical calculations will give more accurate results concerning the difference in these indicators between two genders.
5.1. Limitations and Directions for Future Research
One of the limitations of our study is the relatively small sample size from a single center, which could introduce sampling bias and not be easily generalized to the whole Iranian pediatric population. A more comprehensive randomized sampling method from several hospitals with different demographic and geographical situations representative of the entire Iranian children population can be used in subsequent studies to complete the results of the above article.
Another limitation of our study is its retrospective cross-sectional nature without longitudinal follow-up. We tried to overcome this limitation by standardizing methods and procedures. Future studies with prospective nature and longitudinal follow-ups can be very useful. Another limitation is that all measurements were performed by only one radiologist, which decreases interobserver reliability. In future studies, we could consider having 2 radiologists evaluate the subset for consistency. Future studies on this issue could benefit from multivariate analysis, which minimizes the effect of potential confounding factors in different age groups.
5.2. Conclusions
In conclusion, the normal PVD and PSV in healthy Iranian children were relatively similar to those in their non-Iranian counterparts, and their mean values increased with age. In terms of gender, no significant difference was found between the mean PVD and PSV in boys and girls. The indices calculated in the present study can be used as a basic scale to examine the abnormal changes in the PVD and PSV of Iranian children to diagnose hepatic disorders.