1. Background
Vascular access is essential for children on maintenance hemodialysis (HD). Although arteriovenous fistula (AVF) is the preferred choice for long-term HD in children with chronic kidney disease (1), using central venous catheters (CVCs) for HD vascular access is more common (2). The 2011 Annual Dialysis Report of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) indicated that CVCs accounted for 79% of the 3 363 reported cases of HD (3). Borzych-Duzalka (4) found that 73% (404 cases) of maintenance HD patients in the International Pediatric Hemodialysis Network (IPHN) database between December 2012 and September 2017 received a CVC. The IPHN identified several reasons for the use of CVCs: AVFs require several months to mature, vascular conditions in children may be insufficient for AVF creation, and placing AVFs is technically challenging in young children weighing less than 10 - 15 kg. Additionally, children may be unable to tolerate the pain associated with intubation (5). Therefore, clinicians often require short-term intravenous access. CVCs are a suitable option for vascular access in children who are transitioning to peritoneal dialysis (PD), have a mature AVF, are awaiting immediate kidney transplantation, or require emergency HD.
CVCs remain an essential component of HD in pediatric patients with complex underlying diseases despite the high incidence of venous thromboembolic complications and long-term sequelae (6-9). Increased rates of thrombotic complications have been reported with peripherally inserted central catheters (PICCs) and non-tunneled CVCs compared to tunneled and totally implantable CVCs (10). However, Kanin and Young recently found no difference in CVC-related thrombotic complication rates between PICCs and tunneled CVCs (11). Fadel et al. (12) indicated that long-term vascular access via tunneled cuffed catheters (TCC) remains the preferred choice for CVC selection. The 2019 Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines recommend tunneled CVCs as the preferred choice for long-term HD treatment patients (13).
According to the 2006 National Kidney Foundation's Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines (14), the size of the TCC should be determined based on the child's age and weight. Children's most commonly used chronic catheters are the Ash Split, Bio-Flex Tesio, and Quinton Permcath. The types and sizes of tunneled CVCs will be limited due to economic conditions and emergencies, such as the 2019 Novel Coronavirus outbreak. The 10F Quinton Permcath was inserted as a central line for chronic HD in our institution's children who did not have an AVF suitable for HD access, primarily because of its relatively simple procurement process and cost-effectiveness.
2. Objectives
The present study aimed to analyze the appropriate catheter tip and complications of patients with catheters placed in the last 5 years at our institution in children requiring chronic HD.
3. Methods
The 10F Quinton Permcath was inserted as a central line for chronic HD in all children weighing more than 10 kg who did not have a suitable AVF for HD access. All catheters were placed in the internal jugular vein (IJV) by an experienced intensivist under ultrasonographic vein localization at our hospital between June 2017 and June 2021. Catheters placed in the right IJV were inserted without real-time radiologic guidance, while those placed in the left IJV underwent digital subtraction angiography (DSA).
The 10F Quinton Permcath is a pediatric double-lumen cuffed catheter (Medtronic, Minneapolis, Minnesota, USA) with a total length of 28 cm and a tip-to-cuff length of 13 cm.
We collected clinical data, including patients’ gender, age, weight, and height, and data on early catheter dysfunction and acute complications. Additionally, a chest X-ray examination was performed after catheterization in each case to determine the position of the catheter tip. We also collected imaging data from the patients, comparing the catheter's imaging route and tip position in each case to analyze the characteristics of vascular access establishment and its correlation with catheter-related complications. We subsequently summarized the appropriate surgical methods for vascular access.
When selecting patients, we applied the following inclusion criteria: Children aged < 18 years with chronic kidney disease (glomerular filtration rate (GFR) < 10) who underwent HD treatment at our hospital. Patients meeting the following criteria were excluded: Children with established temporary vascular access by CVC and those with catheters of different sizes and types.
Data were expressed as median and interquartile range.
4. Results
After applying the inclusion and exclusion criteria, 11 children were selected, comprising five males and six females, with a median age of 9 (range: 8 - 10). The median body weight of the included patients was 23.00 (range: 19.95 - 24.30), and the median body height was 122.00 (range: 118.5 - 133.25). The primary morbidity of these 11 children is detailed in Table 1.
| Case | Sex | Age (Y) | Height (cm) | Weight (kg) | Cause of Chronic Renal Failure |
|---|---|---|---|---|---|
| 1 | Male | 8 | 118 | 22 | Unknown |
| 2 | Male | 10 | 121 | 23 | Nephrotic syndrome |
| 3 | Male | 7 | 122 | 23.8 | Antineutrophil cytoplasmic antibody-associated vasculitis |
| 4 | Female | 9 | 134.5 | 26.3 | Nephrotic syndrome |
| 5 | Female | 4 | 87 | 13 | Nephrotic syndrome |
| 6 | Male | 11 | 137 | 21.2 | IgA nephropathy |
| 7 | Female | 14 | 141 | 24.8 | Nephrotic syndrome |
| 8 | Female | 10 | 115.8 | 18.7 | Renal coloboma syndrome |
| 9 | Female | 10 | 122 | 18 | Interstitial nephritis |
| 10 | Male | 9 | 119 | 23 | Right renal agenesis or cystic left kidney |
| 11 | Female | 8 | 132 | 26.3 | Unknown |
Clinical Characteristics of 11 Included Children who Underwent 10F Quinton Permcath placement
Among the 11 cases, eight involved TCC placement in the right IJV, with the catheter tip located at the level of T8 in two cases, T5 in one case, and T7 in the remaining cases. There were no instances of early catheter dysfunction in these cases. Three patients underwent catheter placement in the left IJV when the right IJV could not provide vascular access due to poor vascular conditions, with the catheter tip located at the level of T5, T4, and the T7/T8 intervertebral space, respectively (Table 2). In two patients, there was inadequate blood flow, necessitating the reversal of lumens (using the outflow lumen for blood inflow into the dialyzer). There were no acute complications among the 11 cases where the catheter was inserted.
| Case | Catheter Placement Site | Catheter Location and Depth | Early Catheter Dysfunction | Acute Complications | Type of RRT Before This Surgery |
|---|---|---|---|---|---|
| 1 | Right IJV | Level of the superior margin of T8 | No | No | HD with temporary catheter |
| 2 | Left IJV | Level of the superior margin of T5 | Yes (inadequate blood flow) | No | HD with temporary catheter |
| 3 | Right IJV | Level of the inferior margin of T7 | No | No | HD with temporary catheter |
| 4 | Right IJV | Level of T9, inside the right atrium | No | No | KT |
| 5 | Right IJV | Level of T5 | No | No | HD with temporary catheter |
| 6 | Left IJV | Level of inferior end of T4 | Yes (inadequate blood flow) | No | HD with temporary catheter |
| 7 | Right IJV | Inferior end of T7 | No | No | HD with temporary catheter |
| 8 | Left IJV | Level of T7/T8 intervertebral space | No | No | HD with temporary catheter |
| 9 | Right IJV | Level of the center of the T7 vertebra | No | No | HD with temporary catheter |
| 10 | Right IJV | Level of the superior margin of T7 | No | No | HD with temporary catheter |
| 11 | Right IJV | Level of the superior margin of T7 | No | No | HD with temporary catheter |
Characteristics of 10F Quinton Permcath Placement and Vascular Access in 11 Included Patients
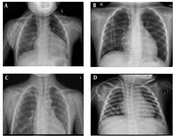
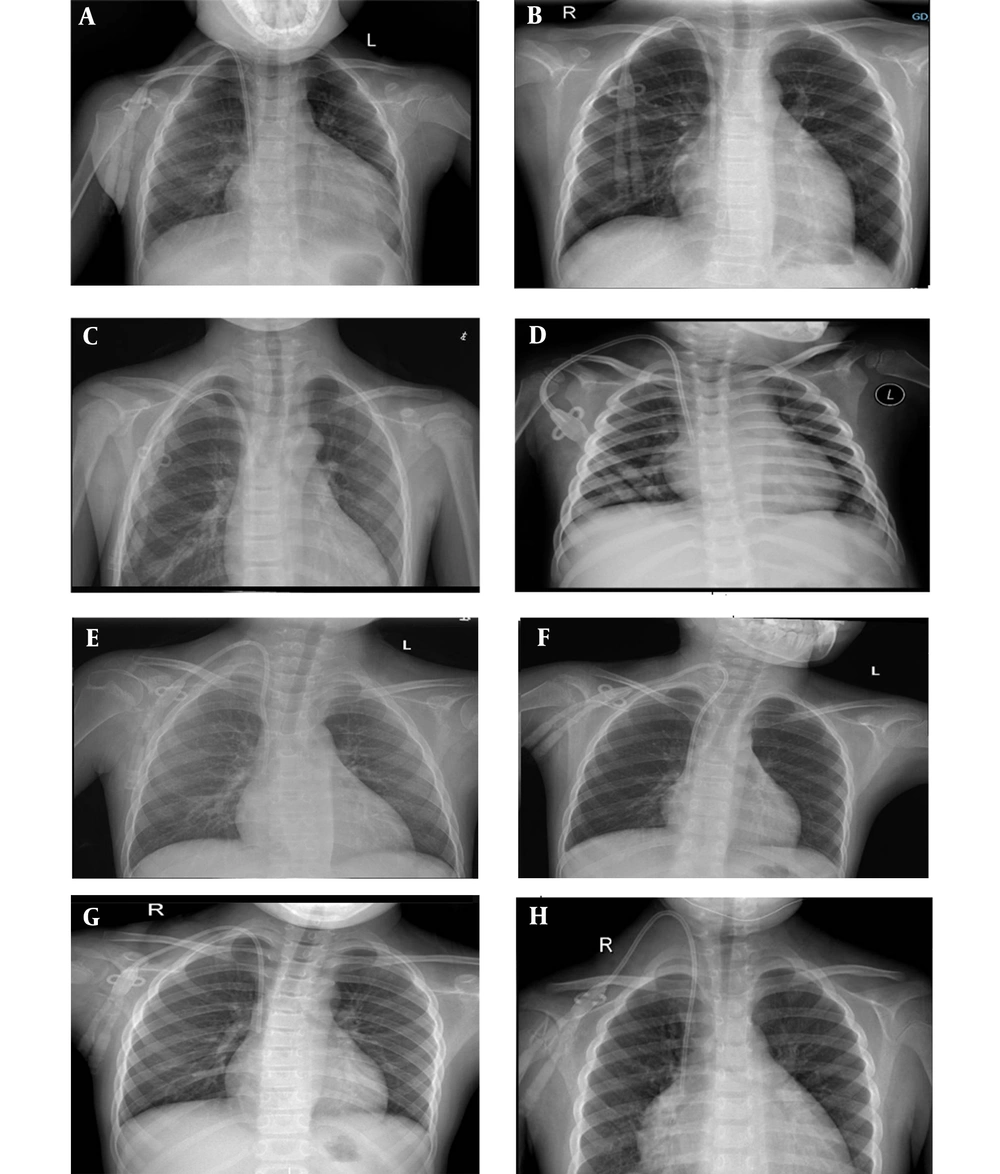
The imaging data of the patients are presented, with eight cases showing catheter placement in the right IJV (Figure 1) and three patients undergoing catheter placement in the left IJV (refer to Figure 2).
5. Discussion
According to the 2019 KDOQI guidelines (13), the tip of a jugular indwelling catheter should be positioned in the mid-superior part of the right atrium. Proper placement of the central venous catheter tip holds crucial clinical significance. A low catheter position in the right atrium can potentially lead to cardiac arrhythmias due to mechanical stimulation of the right atrium (15). Malpositioning of the catheter tip, either below the pericardial reflection or at an acute angle with the vessel wall, is also believed to increase the risk of the rare complication of cardiac perforation (16).
In our study, eight cases involved TCC placement in the right IJV, with the catheter tip located at the level of T8 in two cases, T5 in one case, and T7 in the remaining cases. While previous studies often identified the vertebral level of the cavoatrial junction (CAJ) at T5 or T6 in younger patients (17), Ridge et al. more frequently localized the CAJ at the level of the T7 or T8 vertebral body (18). These eight cases with appropriately placed central venous catheter tips in the right IJV experienced no acute complications or early catheter dysfunction.
The position of the catheter tip may change when patients shift between standing and prone positions, as catheter placement is dynamic and may move 2 - 3 cm in most patients and up to 7 - 10 cm in rare cases.
Subsequently, we conducted a retrospective analysis of the characteristics of CVC implantation in each patient. We compared patient 4 with patient 11 (two individuals with the same weight) and patient 4 with patient 5 (two individuals with a significant weight difference). Patients 4 and 11 weighed 26.3 kg, whereas patient 5 was the lightest at 13 kg. All three individuals underwent long-term catheterization via the right IJV. Chest radiography images of the three cases indicated that the catheter length in the tunnel was shorter in patient 4 than in patients 5 and 11, where the catheter route displayed a curved, C- or U-shaped pattern (Figure 1). The catheter traveling through the blood vessels was relatively shorter compared to case 4, with its tip positioned more shallowly. Within a specific range of patient weights, the position of the catheter tip correlated with the catheter's curvature in the tunnel, allowing for length adjustment in patients with varying weights.
We had concerns regarding the potential impact on blood flow following the creation of curvature in the catheter tunnel. Schon and Whittman found that pre-implantation bending of the catheter into a C- or U-shape could prevent kinking (19). Furthermore, this curved configuration allowed for a continuous curve, preventing luminal constriction. Among the eight individuals in whom the catheter was placed in the right IJV to create a curved trajectory, no early catheter dysfunction was observed. This procedure can be carried out at our center using the 10F Quinton Permcath in patients within a specific range of body weights.
From June 2017 to June 2023 at our center, there were only three cases of TCC placement in the left IJV. Ultrasound assessed bilateral internal jugular vessels before opting for left internal jugular vein insertion. It was discovered that the right vascular stenosis or even occlusion in these three patients resulted from the prolonged presence of temporary tubes in the right internal jugular vein during their previous hospitalizations.
Compared to the right IJV, the left IJV is situated farther from the junction of the superior vena cava and the right atrium. This difference contributes to a decreased likelihood of successful catheter placement on the left side compared to the right side. The route of catheter placement is more curved on the left side than on the right side. There are two bends in the left brachiocephalic vein and at the junction between the brachiocephalic vein and the superior vena cava, resulting in an S- or L-shaped curve in the catheter’s route. As the curves approach 90°, the difficulty of the operation and its associated risks increase. Compared to the right side, catheter placement on the left involves a longer path, more venous tributaries, and increased curvature, raising the risk of positional abnormalities during guide wire or catheter placement.
Schon and Whittman discovered that CVCs placed in the right IJV had a stenosis rate of 27%, while CVCs placed in the left IJV had a stenosis rate of 40% (19). Cui et al. (20) found that out of 1 598 cases of tunnelled central venous catheterization of the jugular vein in adults, the overall success rate of right IJV catheterization was higher than that of left IJV catheterization. However, radiography indicated no significant difference in success rates between the right and left sides.
In the three cases where left IJV catheterization was performed under DSA, percutaneous transluminal angioplasty (PTA) was performed to alleviate catheter stenosis. During the placement of these patients, adjustments were made several times to the curvature of the catheter tunnel. However, the distance from the catheter tip to the cuff was only 13 cm, resulting in a shorter catheter tip length compared to cases involving the left IJV. Patient 8, who weighed less than another patient, had a catheter placed with its tip in an appropriate location (Figure 2). A retrospective study demonstrated a significant reduction in left-sided catheterization failures when the catheter tip terminated in the right atrium as opposed to the superior vena cava or its junction with the atrium (21). Early catheter dysfunction, necessitating the occasional use of reverse lumens (outflow lumens used for blood inflow), was observed in patients 2 and 4 because the catheter tip was not positioned in the superior right atrium. Hence, to enhance the success rate and diminish complications of TCC placement in the left IJV, various sizes of tunnelled cuffed CVCs are required to cater to children of varying ages and weights.
One important limitation of our study is that we did not analyze the outcomes, efficacy, and complications of the tunneled CVCs. This remains a subject for further investigation to determine whether this catheter is a superior choice for children undergoing hemodialysis.
In conclusion, when opting to use the 10F Quinton Permcath, our assessment suggests that the right IJV should be the preferred choice for TCC placement in children with end-stage renal disease. Surgeons should adjust the curvature of the catheter tunnel to place the catheter tip in the appropriate position for patients of different ages and body weights. When poor vascular conditions render the right IJV inaccessible, the left IJV should be considered for long-term hemodialysis access. To enhance the success rate of left IJV placement, in addition to employing DSA technology, dialysis tubes of varying sizes and lengths should be employed for older and heavier children.