1. Background
Congenital abnormalities (CAs), also known as congenital malformations or birth defects, are structural or functional abnormalities present at or before birth, or they may be diagnosed only later in life (1). These defects constitute significant causes of infant and childhood morbidity, disabilities, and deaths, generating a real social impact and requiring long-term specialized care.
An estimated 6% of babies worldwide are born with a congenital anomaly (CA) (2). The prevalence varies by country, with nine out of ten children born with a serious birth defect in low- and middle-income countries (3). Neural tube defects (NTDs) and Down syndrome are among the most common types of CAs (3). While the etiology of most cases remains unknown, it is multifactorial, involving both environmental and genetic factors (4). It is estimated that 30% of CAs are due to recognized genetic factors, 10% to environmental factors, and about 50% remain unexplained (5). Many risk factors have been associated with CAs, including maternal age, environmental pollution, nutrition, medications and use of herbal remedies, maternal chronic diseases, infections contracted by the mother during pregnancy, maternal overweight and obesity, exposure to radiation, and consanguinity (5).
Prevention of some CAs is possible. Folic acid supplementation before and during the first months of pregnancy has proven effective in preventing NTDs and other CAs sensitive to folic acid, such as congenital heart defects and urinary tract anomalies (6).
Recognizing this public health issue, the Moroccan Ministry of Health and Social Protection is committed to implementing prevention programs and early detection of pathologies that cause disability (7). Several preventive measures have been taken, including the fortification of flour with folic acid since 2006, folic acid supplementation since 2008, and a policy of rubella vaccination. Additionally, neonatal screening for congenital hypothyroidism is being generalized throughout the country. Recently, screening for deafness has been implemented in the capital, Rabat, with hopes to extend it nationwide.
Understanding the epidemiological situation and risk factors is crucial for implementing specific prevention measures, thereby reducing neonatal and infant mortality and morbidity.
In Morocco, a system for notifying CAs has been in place since 2012, but it identifies only NTDs and orofacial clefts without providing details about other CAs. According to a recent study by Kannane et al. (8), based on data from the national CA surveillance system, the estimated national prevalence of CAs in Morocco is 3.91 per 1,000 live births (LBs). The study highlights a significant underestimation, noting that the majority of CAs are unspecified congenital malformations (68.55%). Other local studies based on hospital retrospective data have estimated regional prevalence rates between 0.57% and 1.02% of births (9-11). For example, between 2011 and 2014, the nervous system was the most affected system in the Rabat-Salé-Kénitra region, with a prevalence of 19.4% (9). In the same region, a 2020 study found that musculoskeletal anomalies predominated, with a rate of 33% (10). In contrast, during 2022, NTDs were the most common anomalies in the Marrakech-Safi region, with a prevalence of 3.65 per 1,000 births (11).
According to the initial situational analysis (8), the prevalence of CAs in the Beni Mellal-Khenifra region was 5.54 per 1,000 births from 2017 to 2021. However, there is currently no data on the exact regional prevalence of CAs, their distribution, or their risk factors.
2. Objectives
This study aims to report the prevalence of clinically visible CAs by type of anomaly, their distribution, and their risk factors in the Beni Mellal-Khenifra region of central Morocco.
3. Methods
3.1. Study Area and Population
The study was conducted in seven health facilities providing antenatal care in the Beni Mellal-Khenifra region, located in central Morocco. This region covers an estimated area of 28,088 km² and is divided into five provinces: Beni Mellal, Fquih Ben Saleh, Azilal, Khenifra, and Khouribga (12, 13). The region reports a high number of LBs, with 28,020 recorded in 2021, representing 7.3% of the LBs recorded nationally (14). The region has one regional hospital center, four provincial hospitals, six local medical emergency centers, and 52 delivery structures distributed between rural and urban areas.
3.2. Data Collection
3.2.1. Cross-Sectional Study
This retrospective epidemiological study was designed to include 163,842 deliveries from delivery structures between January 2017 and December 2021. Data were obtained from delivery files recorded by local medical services. Clinically detectable cases of CAs were initially screened by midwives through a systematic examination, and all cases were subsequently confirmed by pediatricians and/or general practitioners. All confirmed cases of CAs were included, regardless of whether they were born alive or stillborn, while delivery records indicating that the newborn was normal or the status was unknown were excluded. The types of birth defects were classified according to the diagnostic standards of CAs from the International Classification of Diseases (ICD-10) codes (15).
3.2.2. Case-control Study
For the analytical part of the study, "cases" were defined as any newborns born after 22 weeks of amenorrhea at one of the 63 delivery structures within the study site during the study period (January 2017 to December 2021) who presented with at least one clinically visible CA. Malformed newborns were identified through a systematic examination performed by midwives, and the diagnosis was subsequently confirmed by a pediatrician and/or general practitioner. "Controls" were defined as newborns of the same sex, without any clinically visible CAs at birth, born during the same period and at the same study site. Each identified "case" of CA was compared with three "controls."
The variables included were: Socio-demographic characteristics (such as maternal age and residence area), CAs (type and number of CAs by system and name, newborn sex and weight, etc.), and conditions of delivery (including parity, maternal disease, pregnancy monitoring, consanguinity, medication and plant intake, etc.).
3.3. Ethical Considerations
The researchers obtained permission from Morocco's Ministry of Health and Social Protection to collect the data (Ref. N°482/2021). The principle of anonymity was maintained in the processing of delivery records for mothers with newborns affected by congenital malformations.
3.4. Data Analysis
Collected data were entered and analyzed using SPSS 26 software for Windows. An exhaustive sampling approach was employed for the cases, while random sampling was used to select the controls. To achieve this, all children of the same age and sex were identified, and then three newborns were randomly chosen from among them.
A descriptive analysis was conducted to outline the characteristics of both cases and controls, followed by a bivariate analysis to identify variables for inclusion in the multivariate model.
In the multivariate analysis, conditional logistic regression with sex matching was utilized to explore factors associated with malformations. This approach was chosen for its ability to control for matching effects and minimize potential biases in estimating associations.
4. Results
4.1. Prevalence of Clinically Visible Congenital Abnormalities
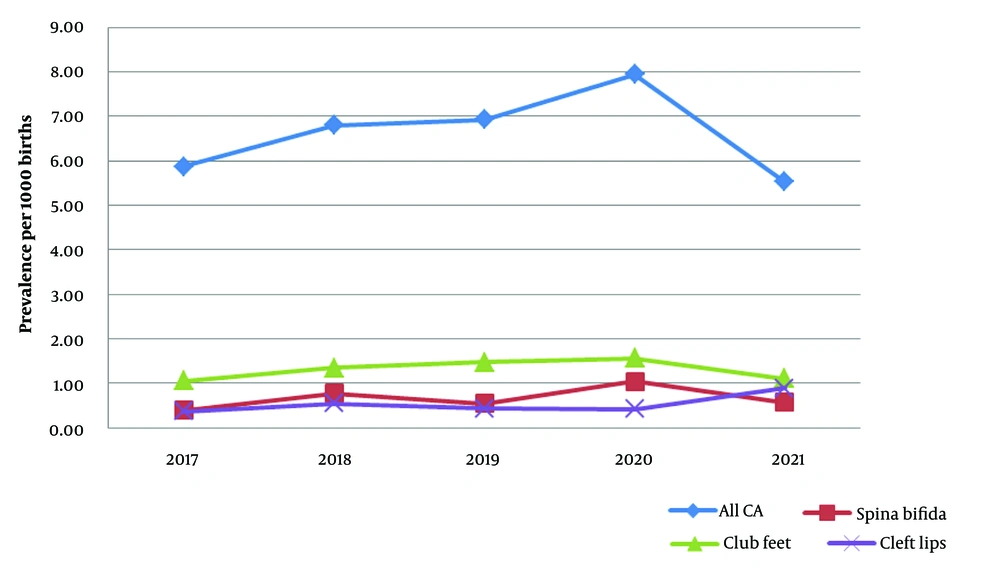
In the entire region over 5 years, 1,085 out of 163,842 delivery files were found to have clinically visible malformations, resulting in an overall prevalence of 6.02 per 1,000 births. The prevalence of CAs ranges from 5.36 to 9.52 per 1,000 births depending on the province, with Khenifra reporting the lowest prevalence at 5.36 per 1,000 births, while Azilal recorded the highest prevalence at 9.52 per 1,000 births (Figure 1).
A progressive increase in annual prevalence was observed between 2017 and 2020, with the maximum annual prevalence of CAs recorded in 2020 (7.94 per 1,000 births), followed by the lowest prevalence in 2021 (5.53 per 1,000 births) (Figure 2). Similar trends were observed for spina bifida and clubfeet, while an opposite trend was noted for cleft lips.
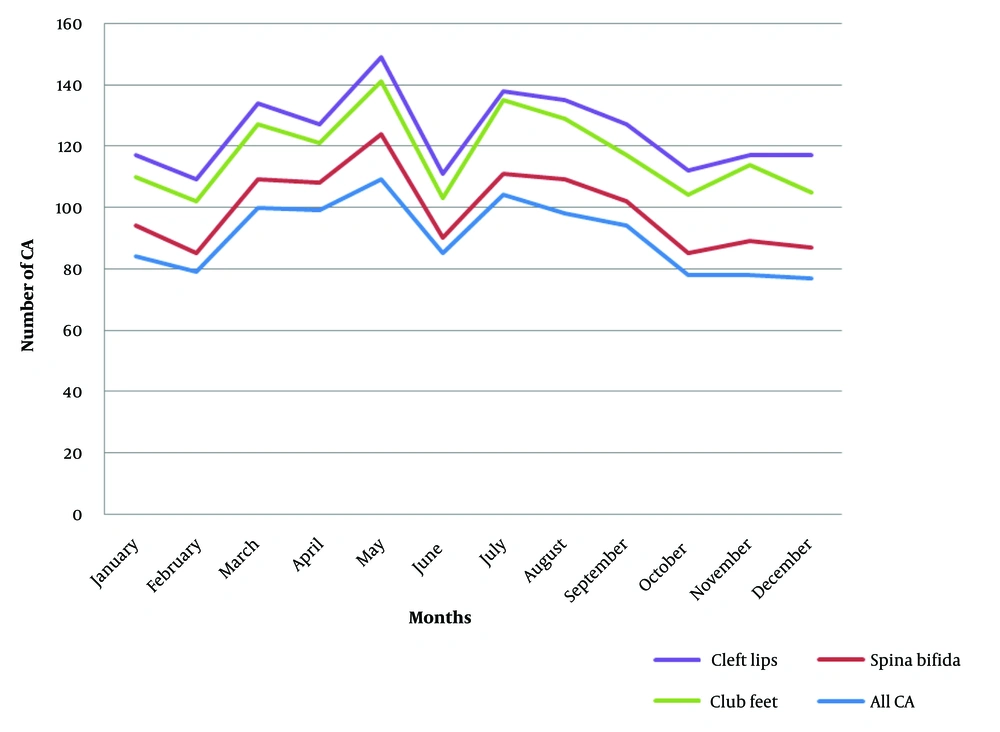
According to the monthly distribution of CAs (Figure 3), the total number of CAs peaked in March, May, and July, and was lowest in February, June, and October. Similar variations were observed for spina bifida, clubfeet, and cleft lips.
4.2. Distribution of Clinically Visible Congenital Abnormalities
Among these newborns with CAs, and according to the ICD-10 classification presented in Table 1, out of 1,085 cases, 1,180 types of CAs were recorded. Of these cases, 17.14% involved polymalformations (at least two malformations), and 70% of the newborns with CAs were from rural areas. Musculoskeletal anomalies were the most common CAs, representing 32.88% of cases. The second most common anomalies were those of the nervous system, accounting for 22.20%. Abnormalities of the genital organs represented 7.37%, while cleft lip and palate accounted for 7.03%. Chromosomal anomalies were present in 5.42% of cases.
| Malformation According to the International Classification ICD-10 | Number of Births with Malformation | Prevalence per 1000B | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Q00-Q07 nervous system | 262 (22.20) | 1.60 | 1.597 | 1.602 |
| Q10-Q18 eye, ear, face and neck | 27 (2.29) | 0.16 | 0.162 | 0.167 |
| Q20-Q28 circulatory system | 12 (1.02) | 0.07 | 0.071 | 0.076 |
| Q30-Q34 respiratory system | 25 (2.12) | 0.15 | 0.15 | 0.155 |
| Q35-Q37 cleft lip and palate | 83 (7.03) | 0.51 | 0.504 | 0.509 |
| Q38-Q45 digestive system | 72 (6.10) | 0.44 | 0.437 | 0.442 |
| Q50-Q56 genital organs | 87 (7.37) | 0.53 | 0.529 | 0.533 |
| Q60-Q64 urinary system | 47 (3.98) | 0.29 | 0.284 | 0.289 |
| Q65-Q79 musculoskeletal system | 388 (32.88) | 2.37 | 2.366 | 2.371 |
| Q80-Q89 other cas | 113 (9.58) | 0.69 | 0.687 | 0.692 |
| Q90-Q99 chromosomal anomalies | 64 (5.42) | 0.39 | 0.388 | 0.393 |
| Total | 1180 (100.00) | 6.02 | 6.018 | 6.022 |
Abbreviations: CAs, congenital abnormalities; ICD-10, International Classification of Diseases.
a Values are expressed as No. (%).
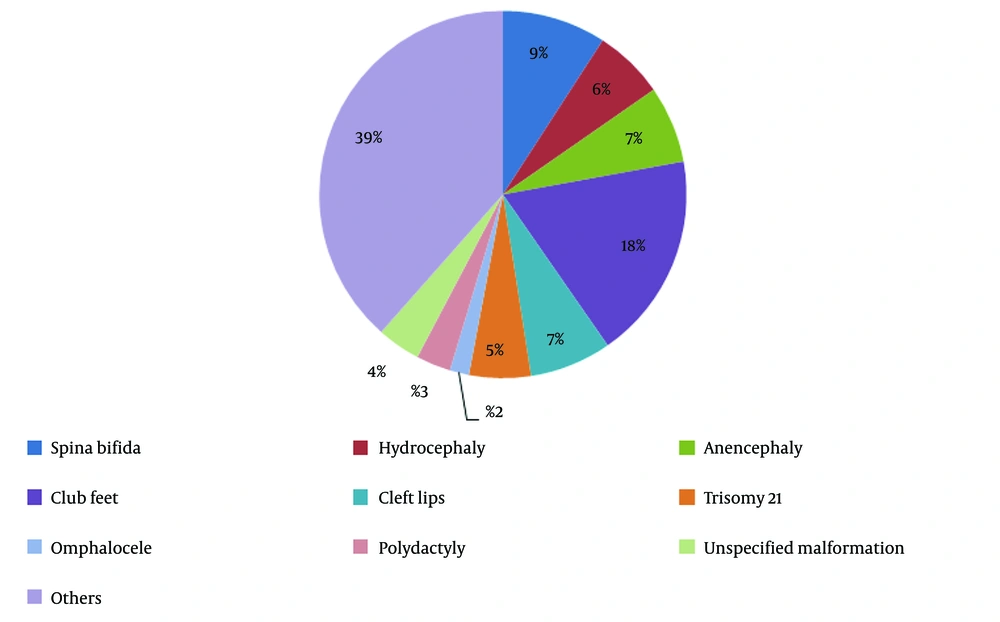
Analysis by type of CAs (Figure 4) revealed that the most frequent CA was clubfoot, found in 18% of cases, followed by spina bifida (9%), anencephaly (7%), and cleft lips and palate (7.9%). Other CAs, such as polydactyly, malformations of the hand, hypospadias, laparoshisis, and choanal atresia, represented 39% of cases. The circulatory system anomalies represented only 1.02% of cases.
Maternal factors associated with CAs included residency (P < 0.050), maternal age over 35 years (P < 0.001), parity (P < 0.05), consanguinity (P < 0.001), a family history of CAs (P < 0.001), medication use before and during pregnancy (P < 0.001), and infection episodes during pregnancy (P < 0.001) (Table 2).
| Variables | Cases; N = 267 (25%) | Control; N = 801 (75%) | Total | P-Value |
|---|---|---|---|---|
| Age class (y) | < 0.001 | |||
| Mother ≥ 35 | 60 (22.5) | 73 (9.1) | 133 | |
| Mother < 35 | 207 (77.5) | 728 (22.5) | 935 | |
| Residence | 0.005 b | |||
| Urban | 74 (27.7) | 156 (19.5) | 230 | |
| Rural | 193 (72.3) | 645 (80.5) | 838 | |
| Matrimonial status | 0.703 nt | |||
| Single | 6 (2.2) | 15 (1.9) | 21 | |
| Married | 261 (97.8) | 786 (98.1) | 1047 | |
| Consanguinity | < 0.001 | |||
| Yes | 39 (14.6) | 24 (3.0) | 63 | |
| No | 228 (85.4) | 777 (97.0) | 1005 | |
| Parity | < 0.001 | |||
| Grand multiparous | 10 (3.7) | 44 (5.5) | 54 | |
| Multiparous | 32 (12) | 215 (26.8) | 247 | |
| Pupiparous | 99 (37.1) | 182 (22.7) | 281 | |
| Prim parous | 126 (47.2) | 360 (44.9) | 486 | |
| Maternal pathology | 0.874 ns | |||
| Yes | 35 (13.1) | 102 (12.7) | 137 | |
| No | 232 (86.9) | 699 (87.3) | 931 | |
| Family history of CA | < 0.001 | |||
| Yes | 9 (1.1) | 44 (16.5) | 53 | |
| No | 792 (98.9) | 223 (83.5) | 1015 | |
| Usage of medication before pregnancy | < 0.001 | |||
| Yes | 9 (52.9) | 8 (47.1) | 46 | |
| No | 241 (90.3) | 781 (97.5) | 1022 | |
| Usage of medication during Pregnancy | < 0.001 | |||
| Yes | 89 (33.3) | 109 (13.6) | 198 | |
| No | 178 (66.7) | 692 (86.4) | 870 | |
| Infection during pregnancy | 39 | < 0.001 | ||
| Yes | 133 (49.8) | 82 (10.2) | 215 | |
| No | 134 (50.2) | 719 (89.8) | 853 |
Abbreviations: nt, not significant; CA, congenital anomaly.
a Values are expressed as No. (%).
b P < 0.050.
The results of the conditional binary regression model, which included socio-demographic and biological factors, indicated that maternal age, consanguinity, parity, maternal pathology, family history, medication taken before and during pregnancy, and infections during pregnancy played roles in the development of congenital malformations. The regression model results (Table 3) show that, in order of significance, infections during pregnancy (χ² = 48.5), family history, medication taken before and during pregnancy, and maternal age are significantly associated with congenital malformations. It appears that infections during pregnancy are most strongly associated with an increased risk of developing a congenital malformation.
The study found that having a family history of CAs increases the risk of birth defects by 10 times. This risk is 6 times higher for babies whose mothers suffered from infections during pregnancy, 5 times higher for those whose mothers used medication before pregnancy, and 3 times higher for those whose mothers used medication during pregnancy. Additionally, being a woman over 35 years old increases the risk of having a malformed baby by 3 times. Similar risks were observed for multiparous mothers and for consanguineous parents.
| Variables | B | SD | χ2 | dl | P-Value | Odds Ratio (CI à 95%) |
|---|---|---|---|---|---|---|
| Residence (ref : Rural) | 0.093 | 0.272 | 0.117 | 1 | 0.732 ns | 1.097 (0.644-1.869) |
| Age range -mother (ref : < 35 y) | 1.098 | 0.328 | 11.238 | 1 | < 0.001 | 2.999 (1.578-5.698) |
| Consanguinity (ref : No) | 1.115 | 0.488 | 5.222 | 1 | < 0.050 | 3.051 (1.172-7.941) |
| Parity (ref : Primiparous) | 1.204 | 0.386 | 9.737 | 1 | < 0.050 | 3.332 (1.565-7.096) |
| Family history of CA (ref : No) | 2.305 | 0.495 | 21.733 | 1 | < 0.001 | 10.029(3.804-26.435) |
| Usage of medication before pregnancy (ref : No) | 1.726 | 0.506 | 11.642 | 1 | < 0.001 | 5.620 (0.574-39.254) |
| Usage of medication during pregnancy (ref : No) | 1.217 | 0.266 | 20.893 | 1 | < 0.001 | 3.376 (2.004-5.688) |
| Infections during pregnancy (ref : No) | 1.792 | 0.257 | 48.510 | 1 | < 0.001 | 6.000 (3.624-9.933) |
Abbreviations: Ref, reference class; B, constant; SD, sum of deviations; dl, degree of liberty; P, significance level of the test of χ2; CI, confidence interval; CA, congenital anomaly.
5. Discussion
Congenital malformations are a major cause of reduced life expectancy and disability. In Morocco, CAs remain a significant health issue due to the lack of a national CA registry. Consequently, epidemiological surveillance primarily focuses on notifying NTDs and orofacial clefts, without specifying other types of CAs. A study conducted in 2014 categorized Morocco as having modest prevention efforts for birth defects (16).
The present study aimed to prospectively investigate the prevalence, distribution, and risk factors of clinically visible CAs in the Beni Mellal-Khenifra region. Out of 163,842 examined LBs, CAs were observed in 1,085 cases, resulting in a prevalence of 6.02 per 1,000 LBs, which is higher than the prevalence estimated for the study region by the national surveillance system (5.54/1,000 births) (8). This discrepancy may be attributed to notification omissions in some cases.
The prevalence found in our study is lower compared to the 10.2/1,000 LBs reported by Elghanmi et al. (9) for the 2011–2014 period at the Souissi Maternity in Rabat. However, our prevalence is relatively higher than the 5.58/1,000 LBs reported by Forci et al. (10) for the 2011 - 2016 period in Rabat. Additionally, a recent study conducted by our laboratory in the Marrakech-Safi region in 2022 reported a CA prevalence of 9.2/1,000 births, with NTDs being the most frequent (3.65/1,000 births), followed by musculoskeletal and digestive tract anomalies. Despite similarities in socio-demographic data (14) between the regions—such as poverty rate, urbanization rate, total fertility rate, and literacy rate—the Marrakech-Safi region exhibited a much higher prevalence. This discrepancy may be due to the Marrakech University Hospital serving multiple regions and the presence of additional risk factors that warrant further investigation.
Notably, the prevalence found in our study remains higher than the national prevalence of 3.91/1,000 LBs estimated for the same period by the national surveillance system. Similar prevalence rates were observed in other studies, such as 6.5/1,000 LBs reported by Ekwochi et al. (17) in a tertiary healthcare facility in South-East Nigeria and 0.62% reported by Mekonnen et al. (4) in Ethiopia.
The highest prevalence was recorded in Azilal province (9.52/1,000 births), known for its challenging conditions, including high poverty rates, high illiteracy rates, and limited geographical and cultural access to healthcare.
The maximum annual prevalence of CAs peaked in 2020 (7.94/1,000 births) and decreased in 2021 (5.53/1,000 births). Similar trends were observed for spina bifida and club feet, although no seasonal variations were detected in our data analysis.
In our study, the most common CAs were musculoskeletal system anomalies (32.88%), followed by nervous system anomalies (22.20%). This aligns with Forci et al. (10), who reported musculoskeletal abnormalities as the most frequent, followed by neurological abnormalities. Conversely, Elghanmi et al. (9) found that neurological abnormalities were the most common, followed by musculoskeletal abnormalities. In Nigeria, Ekwochi et al. (17) reported that more than half of the anomalies involved the musculoskeletal system. A 2020 meta-analysis by Adane et al. (18) found that musculoskeletal system defects were the most prevalent type of CA in sub-Saharan Africa (3.90/1,000 births), while Down syndrome was the least prevalent (0.62/1,000 births).
Many studies have reported that congenital heart malformations are the most common defects (19-21). In contrast, only 1.02% of the CAs detected in our study were circulatory system abnormalities, which is likely an underestimation given the prevalence of congenital heart disease. One reason for this underestimation is the difficulty in diagnosing such conditions clinically, as they are often associated with fetal asphyxia and are usually identified only after transfer to a tertiary hospital.
In our study, the most frequent congenital malformation was club feet (18%), followed by spina bifida (10%), anencephaly (7%), and cleft lip and palate (7.9%). A retrospective 21-year study conducted in Tunisia found that limb defects were the most frequently detected malformations (22).
The high prevalence of NTDs (1.15/1,000 births) may be attributed to the consumption of fenugreek, a teratogenic plant commonly used in Morocco (23). Skalli (24) and Seddiki et al. (25) observed a correlation between the consumption of fenugreek and the occurrence of NTDs. Conversely, a 2021 Moroccan study found that there was no effective prevention of NTDs with folic acid in the preconception period, as only 41% of mothers had taken it during the first trimester of pregnancy (26).
Our study found that males are more likely to have CAs than females, a trend also observed in other Moroccan and international studies (9, 10, 27-31). However, a one-year Moroccan study by Sabiri et al. (32) found a sex ratio of 1.
Most women who gave birth to malformed newborns lived in rural areas (72.3%), where the urbanization rate is low (41%), in contrast to studies conducted in Morocco’s capital where urbanization is very high. These findings suggest that in rural areas, the high prevalence of CAs can be attributed to poor living conditions, lack of hygiene, and inadequate medical monitoring during pregnancy.
Our results also indicated that mothers over 35 years old are more likely to have newborns with CAs, consistent with other studies showing that this age group is more commonly represented among mothers (9, 33, 34). However, this finding contradicts several studies (17, 35, 36) that have reported higher CA rates in mothers under 35 years. Our findings align with a study conducted in Ethiopia (4), which concluded that maternal age and residence significantly affect the risk of CAs. In addition to age, our study identified other maternal risk factors, including multiparity, consanguinity, genetic factors, medication use before and during pregnancy, maternal pathology, and infection episodes during pregnancy. These findings highlight the need to adopt and adapt CA prevention measures contextually for greater effectiveness.
Our study is the first in the Beni Mellal-Khenifra region to provide an overview of CAs and analyze the associated risk factors. However, the prevalence in our study is likely underestimated due to the non-inclusion of abortions involving CAs; this information is not available in our context. Additionally, the study did not include home births, which account for 25% of deliveries in Morocco (37), nor did it include data from the private sector.
Based on our results, we recommend establishing a CA registry to prevent missed notifications and obtain more detailed case information. We also suggest implementing prenuptial and preconception consultations, improving pregnancy monitoring, especially in rural areas, and conducting a study to identify risk factors associated with the most common malformation in our context, which is club feet.
5.1. Conclusions
Our study is the first to describe the epidemiology of congenital abnormalities and their risk factors in the study area. The relatively high prevalence of congenital abnormalities in our study highlights the need for improved prevention strategies, including preconception care, enhanced pregnancy monitoring, folic acid supplementation, avoidance of consanguineous marriages, and careful consideration of medication and plant use, particularly in disadvantaged areas.